“Fasting is dangerous for people with high blood pressure”—this widely repeated medical advice has kept many hypertension sufferers from exploring one of the most powerful natural interventions available. Yet groundbreaking research reveals that properly implemented fasting protocols may actually normalize blood pressure more effectively than many medications. At IFitCenter, we’ll explore this fascinating paradox and the science behind it.
The evidence is compelling: in a landmark study of 174 hypertensive patients who underwent medically supervised fasting, 89% achieved normal blood pressure readings—with an average systolic reduction of 37 points—even after discontinuing their medications. From intermittent fasting to time-restricted eating, specific protocols have demonstrated remarkable effects on blood pressure, but understanding the correct implementation is crucial. This comprehensive guide examines the powerful connection between fasting and blood pressure, providing evidence-based insights for those seeking natural approaches to cardiovascular health.
Very Important Note: This article is purely educational and is based on research conducted on the relationship between fasting and blood pressure. Under no circumstances should you implement fasting on your own or without medical supervision, nor should you make any changes to your medication regimen.
What effect does fasting have on blood pressure?
Beyond Medication: A Different Approach
Conventional approaches to treating hypertension focus primarily on medication—diuretics, ACE inhibitors, calcium channel blockers, and beta-blockers—that address symptoms rather than root causes. While these medications can be effective, they often come with unwanted side effects and may require lifelong use.
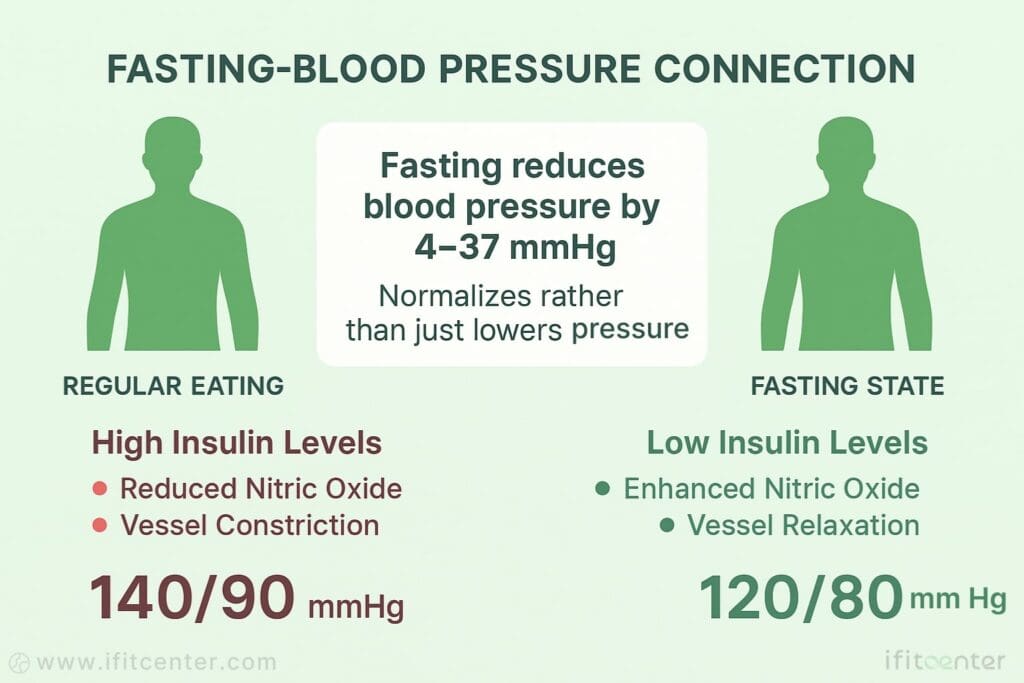
Fasting offers a fundamentally different approach that targets the underlying metabolic mechanisms of hypertension. When we fast, our body undergoes a metabolic shift where insulin levels drop significantly, allowing several beneficial processes to unfold. This fasting state enhances fat burning, reduces inflammation, and improves cellular repair processes—all with potential benefits for blood pressure regulation.
Fasting Approaches That Lower Blood Pressure
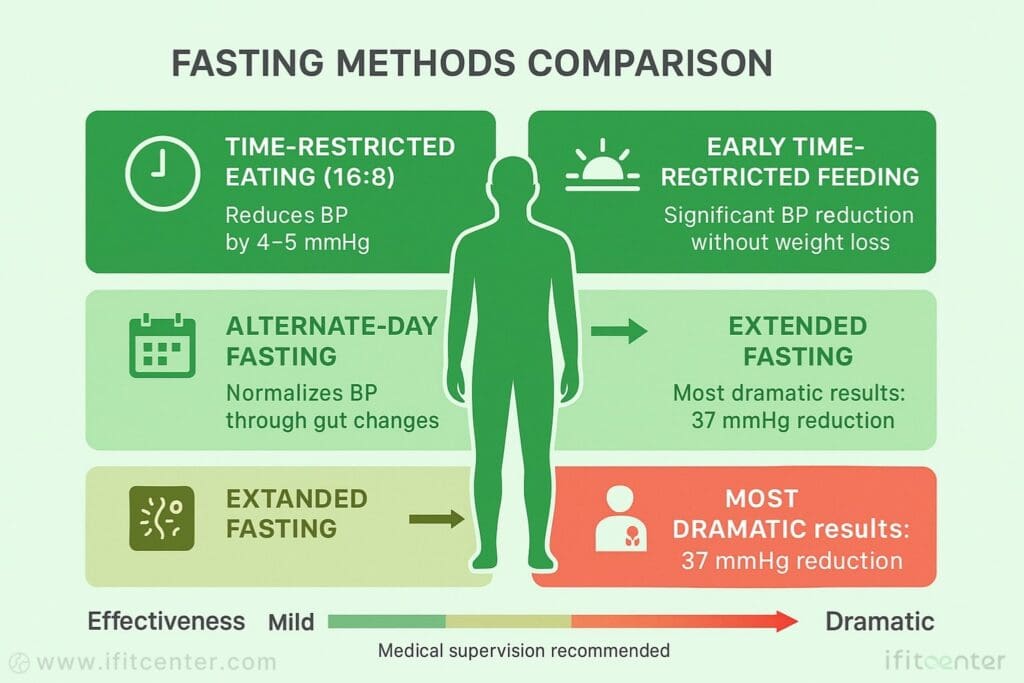
Several fasting approaches have shown promising results for blood pressure management. Time-restricted eating (limiting daily food intake to a specific window, typically 6-10 hours) has been shown to reduce systolic blood pressure by approximately 4-5 mmHg in clinical studies. Intermittent fasting (alternating between fasting and eating days) and extended fasting (periods without food lasting 24+ hours) have demonstrated even more substantial effects in some research.
The Evidence: What Research Shows
The scientific evidence for fasting’s effect on blood pressure is compelling. A comprehensive study published in the Journal of the American Heart Association examined 1,610 participants undergoing fasting periods ranging from 4-21 days. The results showed that mean blood pressure decreased from 126.2/81.4 to 119.7/77.6 mmHg. Most remarkably, those with severe hypertension (>160/100 mmHg) experienced reductions of 24.7/13.1 mmHg—comparable to what’s typically achieved with medication.
What makes fasting unique is its ability to normalize blood pressure. Studies have consistently observed that individuals with high blood pressure experience significant reductions, while those with low blood pressure may see slight increases. This suggests fasting helps restore proper blood pressure regulation rather than simply forcing numbers lower.
The Insulin Connection
Insulin resistance appears to be a key link between modern eating patterns and hypertension. When we eat frequently, especially carbohydrate-rich foods, insulin levels remain chronically elevated. High insulin reduces nitric oxide production in blood vessels, causing them to constrict and blood pressure to rise. Fasting breaks this cycle by dramatically lowering insulin levels, allowing blood vessels to relax and blood pressure to normalize.
On the IFitCenter blog, we have prepared a free information database about various diseases, including high blood pressure, for you, our dear readers. By reviewing these resources, you will gain valuable information for controlling and preventing these conditions. To access the first part of the information, you can use the links below:
- what is normal blood pressure
- high blood pressure symptoms
- bp chart
- cause of hypertension
- how to measure blood pressure at home
- healthy eating to lower blood pressure
- foods to avoid with high blood pressure
Additional Mechanisms and Rapid Benefits
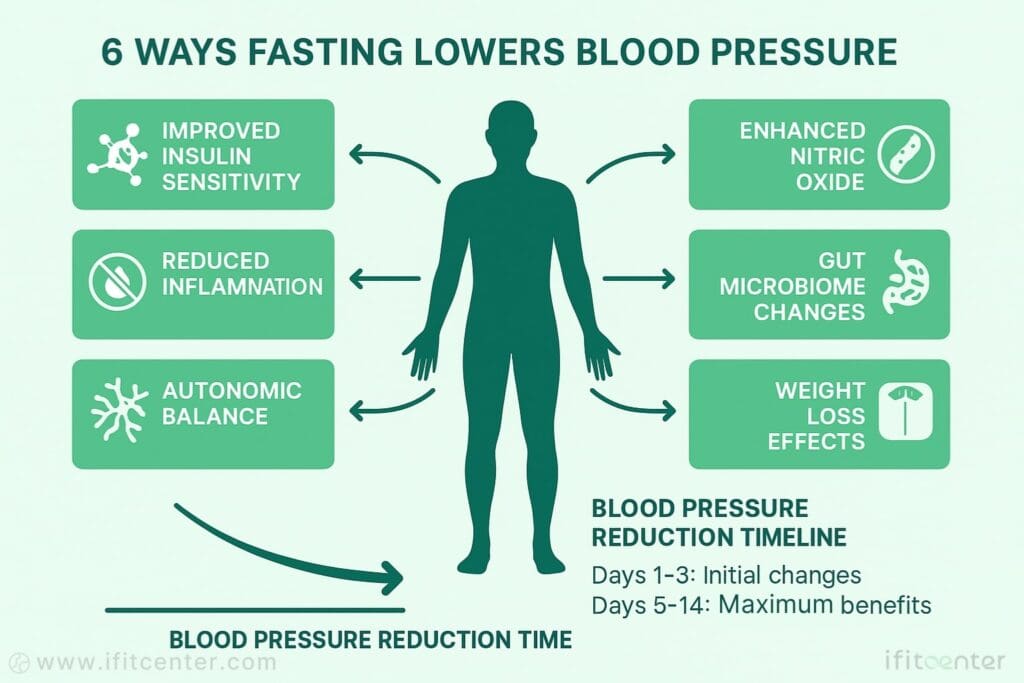
Other mechanisms behind fasting’s blood pressure effects include increased sodium excretion associated with ketosis, enhanced sensitivity to natriuretic peptides (hormones that regulate sodium balance), and positive changes in the autonomic nervous system that governs blood vessel tone. Recent research has also identified beneficial changes in the gut microbiome that contribute to improved blood pressure regulation during fasting periods.
Perhaps most impressive is that these effects can occur rapidly—sometimes within days of beginning a fasting protocol—and often before significant weight loss. Early time-restricted feeding studies have demonstrated blood pressure improvements even in the absence of weight change, confirming that fasting’s benefits extend beyond simple calorie reduction.
Does fasting cause hypertension?
Common Misconceptions
Despite concerns that fasting might stress the cardiovascular system and raise blood pressure, research consistently shows the opposite effect. Multiple studies, including a large-scale analysis of 1,610 participants published in the Journal of the American Heart Association, demonstrate that properly implemented fasting protocols typically lower blood pressure rather than cause hypertension.
Normalizing Effect on Blood Pressure
Fasting appears to have a normalizing effect on blood pressure rather than simply reducing it. In the comprehensive Blood Pressure Changes study, participants with normal blood pressure experienced modest reductions of approximately 3.0/1.9 mmHg. Interestingly, subjects with very low baseline pressure (below 100/60 mmHg) actually saw increases of 6.3/2.2 mmHg. This suggests fasting helps restore proper blood pressure regulation rather than pushing readings to extreme lows.
Long-term Blood Pressure Effects
Research on longer fasting periods consistently demonstrates beneficial effects on blood pressure. In the study of 1,610 participants, blood pressure stabilized around 120/78 mmHg regardless of starting values. Follow-up assessments after fasting interventions indicate these improvements can persist when healthier eating patterns are maintained. The London Ramadan Study (LORANS) similarly found blood pressure reductions were maintained at four-week follow-up.
Hydration Considerations
Proper hydration remains essential during fasting to avoid potential hypotension (abnormally low blood pressure) or dehydration-related complications. The large-scale study of 1,422 individuals undergoing 4-21 day fasting periods reported no serious hypotensive events when proper hydration protocols were followed. Most fasting approaches allow water, herbal teas, and in some cases, limited electrolyte supplementation to maintain proper fluid balance.
Therapeutic Fasting vs. Starvation
It’s crucial to distinguish between therapeutic fasting and starvation, which have dramatically different physiological effects. The well-documented Buchinger fasting method, for example, provides approximately 200-250 calories daily through liquids while ensuring adequate hydration and electrolyte balance. This controlled approach allows for metabolic benefits without the cardiovascular distress associated with involuntary starvation, explaining why properly implemented fasting protocols support blood pressure regulation rather than causing hypertension.
Benefits of fasting in controlling and lowering blood pressure
Insulin Sensitivity: A Key Mechanism
Research identifies insulin resistance as a primary driver of hypertension. Studies show that fasting is remarkably effective at lowering insulin levels and improving sensitivity. In the INTERFAST-MI trial, researchers observed significant improvements in both insulin sensitivity and blood pressure with intermittent fasting. This connection exists because high insulin levels reduce nitric oxide production in blood vessels, causing constriction and elevated pressure.
Nitric Oxide and Vascular Function
Fasting enhances nitric oxide production, the body’s natural vasodilator. The Cell Metabolism study on early time-restricted feeding demonstrated that improved blood pressure occurred alongside reduced oxidative stress and enhanced vascular function, even without weight loss. This confirms fasting’s direct effect on the blood vessels’ ability to dilate properly, reducing resistance to blood flow.
Gut Microbiome Transformation
A groundbreaking study in Circulation Research demonstrated that intermittent fasting restructures the gut microbiota in ways that directly lower blood pressure. When microbiota from fasted animals was transplanted to hypertensive animals, their blood pressure normalized. The mechanism involves altered bile acid metabolism and activation of bile acid receptors that improve vascular function, offering a novel pathway for blood pressure reduction.
Autonomic Nervous System Regulation
Fasting beneficially affects the autonomic nervous system that regulates blood pressure. A study in the American Journal of Physiology found that even a 24-hour fast enhanced vagal tone (parasympathetic activity) and improved cardiovagal baroreflex sensitivity. These changes help the body better regulate blood pressure fluctuations, contributing to more stable and typically lower readings.
Different Population Responses
Fasting’s effects vary across different populations. In the 1,610-participant study, normotensive subjects experienced modest blood pressure decreases of 3.0/1.9 mmHg. Hypertensive non-medicated subjects saw dramatic reductions of 16.7/8.8 mmHg, with those having severe hypertension (>160/100 mmHg) experiencing the most significant drops of 24.7/13.1 mmHg. For hypertensive medicated subjects, 23.6% were able to discontinue all medications while maintaining blood pressure control.
Timeframe and Sustainability
Blood pressure improvements begin remarkably quickly with fasting. The comprehensive study of hypertensive non-medicated subjects recorded significant decreases beginning from the first day of fasting. For those practicing early time-restricted eating, significant blood pressure changes were observed within 5 weeks. The meta-analysis of Ramadan fasting found benefits persisted up to four months after the fasting period ended, while other studies tracking participants for up to a year showed maintained improvements when healthier eating patterns continued.
“What many of my hypertensive patients find surprising is that fasting doesn’t just temporarily lower blood pressure—it actually helps normalize it. We’ve seen patients with very high readings experience dramatic reductions of 20-25 mmHg, while those with low blood pressure often see slight increases. This normalizing effect distinguishes fasting from medications that simply force numbers lower regardless of what your body needs”
Dr. Babak Jamalian, Family Physician
Restrictions of fasting in hypertension
Medical Contraindications
While fasting offers benefits for many with hypertension, certain medical conditions make it unsafe. According to clinical research, fasting is contraindicated for individuals with: BMI under 16 kg/m² or cachexia, anorexia nervosa or other eating disorders, advanced kidney or liver insufficiency, cerebrovascular disease, dementia or serious cognitive impairment, and during pregnancy or lactation. The safety study of 1,422 fasting participants specifically excluded these conditions from participation.
Medication Considerations
Certain blood pressure medications require special consideration during fasting. Diuretics may need adjustment to prevent dehydration and electrolyte imbalances. ACE inhibitors and ARBs can cause significant blood pressure drops when combined with fasting, potentially leading to hypotension. Research from the LORANS study emphasizes that treatment for hypertension needs careful monitoring and potential adjustment during fasting periods.
High-Risk Situations
Even without absolute contraindications, some situations warrant close medical supervision during fasting. These include: uncontrolled or severe hypertension (>180/120 mmHg), recent cardiovascular events, diabetes requiring medication, history of hypoglycemia, and advanced age with frailty. The INTERFAST-MI trial demonstrated that while fasting can be safe even for patients recovering from heart attacks, careful monitoring remains essential.
Warning Signs to Stop Fasting
Certain symptoms indicate fasting should be discontinued immediately: severe lightheadedness or dizziness, confusion or altered mental status, severe weakness preventing daily activities, heart palpitations or chest pain, and significant gastrointestinal distress. The large-scale safety study of 1,422 fasting subjects identified these as potential signs of adverse reactions requiring medical evaluation.
Personal Assessment
Determining if fasting is appropriate for your hypertension requires consideration of several factors: current blood pressure control, medication regimen, overall health status, and previous fasting experience. Clinical guidelines suggest starting with shorter fasting periods (12-14 hours) before attempting more extended protocols. A pre-fasting health assessment, including blood pressure monitoring, basic metabolic panel, and cardiovascular evaluation, provides important baseline information to ensure safety.
To access the second section of blood pressure articles, I invite you to use the links below:
- dash diet for hypertension
- Best foods for hypertension
- complications hypertension
- obesity and hypertension statistics
- Can high blood pressure cause headaches?
Which type of fasting is best for hypertension?
Time-Restricted Eating (TRE)
Time-restricted eating limits daily food intake to a specific window, typically 6-10 hours. A systematic meta-analysis found that TRE significantly reduces systolic blood pressure by approximately 3.45 mmHg on average. The 10-hour TRE protocol studied at Cell Metabolism demonstrated reductions of 5.12 mmHg systolic and 6.47 mmHg diastolic in patients with metabolic syndrome. This approach appears particularly effective when practiced for at least 12 weeks, making it sustainable for long-term blood pressure management.
Early Time-Restricted Feeding
This specialized form of TRE involves consuming all meals earlier in the day (e.g., between 8am-3pm). The pioneering Cell Metabolism study demonstrated that this approach significantly lowered both systolic and diastolic blood pressure in men with prediabetes, even without weight loss. By aligning eating with natural circadian rhythms, early TRE appears to enhance metabolic function and blood pressure regulation more effectively than later eating windows.
Modified Fasting (Buchinger Method)
This approach allows approximately 200-250 calories daily from fruit juices and vegetable broths during fasting periods. The Journal of the American Heart Association study of 1,610 participants showed this method reduced blood pressure from 126.2/81.4 to 119.7/77.6 mmHg, with the greatest effects in those with severe hypertension. The modified nature of this fast makes it more accessible while still providing significant blood pressure benefits.
Extended Water Fasting
Medically supervised water-only fasting for periods of 10-11 days demonstrated the most dramatic blood pressure reductions in scientific literature. The landmark study of 174 hypertensive patients showed an average systolic reduction of 37 points, with those having severe hypertension experiencing approximately 60-point reductions. While highly effective, this approach requires strict medical supervision and is typically reserved for cases not responding to other interventions.
Religious Fasting (Ramadan-Style)
The LORANS study and associated meta-analysis examined Ramadan fasting, which involves abstaining from food and water from dawn to sunset for one month. This pattern reduced systolic blood pressure by 3.19 mmHg overall, with hypertensive individuals experiencing more substantial reductions of 8.44 mmHg. The cyclical nature of this approach may be culturally familiar and therefore sustainable for many individuals.
Comparative Effectiveness
When comparing approaches, the Nutrition Journal randomized controlled trial provides valuable insights by directly comparing DASH diet alone versus DASH with time-restricted eating. The combined approach produced significantly greater blood pressure reductions, suggesting that fasting enhances the effects of other dietary interventions. For most individuals with mild to moderate hypertension, time-restricted eating (especially earlier in the day) offers the optimal balance of effectiveness, safety, and sustainability for long-term blood pressure management.
“The timing of your eating window may be just as important as its duration. Early time-restricted feeding—where all meals are consumed before mid-afternoon—has shown remarkable blood pressure benefits even without weight loss. This approach aligns with our body’s natural circadian rhythms, enhancing metabolic function and nitric oxide production in ways that later eating windows don’t match, regardless of calorie content.”
Dr. Babak Jamalian, Family Physician
The correct way to perform fasting for hypertension
Preparation Steps
Before beginning any fasting protocol for hypertension, consult with a healthcare provider and obtain baseline measurements. Studies recommend a pre-fast assessment that includes blood pressure readings, basic metabolic panel, and review of current medications. The PLOS ONE study of 1,422 participants included a pre-fasting phase with light meals of fruits and vegetables to prepare the digestive system and prevent constipation during the fast.
Hydration Requirements
Proper hydration is critical during fasting periods. Research protocols typically recommend drinking 2-3 liters of water daily during fasting. The Buchinger method used in the 1,610-participant study allowed water, herbal teas, and small amounts of juice (approximately 250ml) to maintain hydration without significantly impacting the metabolic benefits of fasting.
Electrolyte Balance
Longer fasting periods require attention to electrolyte balance. The European Journal of Preventive Cardiology study noted that sodium excretion decreases during fasting, requiring less salt supplementation than many assume. For fasts extending beyond 5 days, however, small amounts of minerals may be necessary. The Buchinger protocol included vegetable broth (approximately 250ml daily) partly to provide these minerals in a natural form.
Blood Pressure Monitoring
Regular monitoring is essential during fasting. Research protocols typically measure blood pressure at the same time each day to account for natural circadian variations. The Hypertension in Time-Restricted Eating study found that morning readings provided the most consistent results. For those on medications, twice-daily measurements (morning and evening) help detect potential hypotension requiring medication adjustment.
Breaking the Fast Properly
How you end a fast is as important as how you begin it. The large-scale JAHA study implemented a structured 4-day refeeding phase after fasting to prevent digestive distress and blood pressure fluctuations. This typically involves starting with small portions of easily digestible foods like fruits, vegetables, and soups before gradually reintroducing other food groups.
Gradual Implementation
For beginners, research suggests starting with shorter fasting periods and gradually extending them. The time-restricted eating study showing blood pressure benefits began with a 12-hour fasting window before gradually extending to 10-hour and then 8-hour eating periods over several weeks. This gradual approach improves both safety and long-term adherence.
Individual Adaptations
Research indicates that fasting responses vary between individuals. The LORANS meta-analysis found that those with higher baseline blood pressure experienced the most significant improvements. This suggests fasting protocols should be customized based on baseline readings, medication status, and individual response. Regular reassessment allows for protocol adjustments to optimize blood pressure benefits.
Complementary Approaches
Multiple studies demonstrate enhanced results when fasting is combined with other lifestyle modifications. The Nutrition Journal randomized controlled trial found that combining time-restricted eating with the DASH diet produced superior blood pressure reductions compared to either approach alone. Similarly, research indicates that moderate physical activity during fasting periods enhances blood pressure improvements, with walking and light exercise being the most commonly recommended forms.
Complications of incorrect implementation of fasting in hypertension
Common Adverse Effects
While properly conducted fasting is generally safe for hypertension management, incorrect implementation can lead to adverse effects. The PLOS ONE safety study of 1,422 subjects reported that less than 1% of participants experienced adverse events, with the most common being sleep disturbances, fatigue, and dry mouth primarily occurring in the initial days. Improper fasting approaches may increase these symptoms or lead to more serious complications.
Electrolyte Imbalances
Extended fasting without proper mineral intake can lead to electrolyte abnormalities. Warning signs include muscle cramps, weakness, irregular heartbeat, and headaches. The Buchinger protocol studied in the JAHA research specifically included vegetable broth and diluted juice to provide minimal essential electrolytes, indicating the importance of these elements even during fasting periods.
Hypotension Risks
Excessive blood pressure lowering (hypotension) can occur, particularly in medicated patients. The large study of 1,610 participants found that 23.6% of medicated hypertensive subjects were able to discontinue all medications during fasting, highlighting the need for medication adjustment. Symptoms of hypotension include dizziness, lightheadedness, blurred vision, and in severe cases, fainting.
Medication Interactions
Certain blood pressure medications require special monitoring during fasting. The European Journal of Preventive Cardiology study noted that diuretics may need dosage reduction or temporary discontinuation during fasting to prevent dehydration and electrolyte imbalances. Similarly, ACE inhibitors and ARBs may cause pronounced blood pressure drops when combined with fasting, necessitating careful monitoring and potential adjustment.
Managing Physiological Stress
Improperly implemented fasting can increase physiological stress, potentially counteracting blood pressure benefits. The Influence of Acute Fast study found that while 24-hour fasting enhances parasympathetic activity, longer unstructured fasting may increase sympathetic activation, potentially raising blood pressure. Structured protocols with appropriate caloric allowances (like the Buchinger method’s 200-250 calories) help minimize this stress response.
Normal vs. Concerning Symptoms
Distinguishing between normal adaptation symptoms and concerning side effects is crucial. Research indicates that mild hunger, slight fatigue, and minor headaches during the first 2-3 days represent normal adaptation to fasting. In contrast, severe weakness, persistent dizziness, heart palpitations, vomiting, or confusion are abnormal responses that warrant immediate medical attention and cessation of fasting.
When to Seek Medical Help
Clinical guidelines derived from fasting research recommend immediate medical attention if: blood pressure drops below 90/60 mmHg, heart rate becomes irregular or extremely slow/fast, severe lightheadedness or fainting occurs, chest pain develops, or confusion arises.
How to take blood pressure medications during fasting?
General Medication Principles
The relationship between fasting and blood pressure medications requires careful management. The large-scale study of 1,610 participants found that 23.6% of medicated hypertensive subjects completely discontinued medications during fasting while maintaining blood pressure control. Another 43.5% reduced their dosages significantly. These findings highlight the need for medication adjustment rather than simply continuing pre-fasting regimens, which could potentially lead to hypotension.
ACE Inhibitors and ARBs
These medications (examples include lisinopril, enalapril, losartan, valsartan) require special attention during fasting. Research indicates that fasting enhances their blood pressure-lowering effect, potentially due to improved insulin sensitivity. The INTERFAST-MI trial suggests these medications are typically taken with water even during fasting periods, but dosage reductions may be necessary if blood pressure drops below 110/70 mmHg.
Calcium Channel Blockers
Medications like amlodipine, nifedipine, and diltiazem generally cause fewer concerns during fasting than other classes. The hypertension fasting studies indicate these medications can typically be continued at regular doses, as their mechanism of action (blocking calcium entry into vascular smooth muscle cells) appears less affected by the metabolic changes of fasting.
Beta-Blockers
Fasting can enhance the effects of beta-blockers (such as metoprolol, atenolol, and propranolol). Studies indicate that monitoring heart rate becomes particularly important when using these medications during fasting, as excessive drops below 55-60 beats per minute may occur. According to the American Journal of Physiology study, fasting naturally decreases heart rate by approximately 4 beats/minute, which compounds beta-blocker effects.
Diuretics
Research consistently identifies diuretics (like hydrochlorothiazide, chlorthalidone, and furosemide) as the medication class requiring the most significant adjustments during fasting. The Buchinger study noted that fasting naturally enhances natriuresis (sodium excretion), potentially making diuretics redundant or excessive. Many protocols recommend temporary reduction or suspension of diuretics during fasting periods to prevent dehydration and electrolyte imbalances.
Medication Timing
For time-restricted eating protocols, the European Journal of Preventive Cardiology study suggests taking medications during the eating window when possible to minimize gastrointestinal discomfort. Long-acting medications taken once daily are preferred during fasting, as they maintain consistent blood pressure control regardless of meal timing. For medications requiring twice-daily dosing, spacing them at opposite ends of the eating window often provides optimal coverage.
Monitoring and Adjustment Protocol
Research protocols typically recommend measuring blood pressure twice daily during fasting—morning and evening. The JAHA study employed a stepwise approach to medication adjustment: if systolic readings dropped below 110 mmHg consistently, medication dosages were reduced by 25-50%. If readings fell below 100 mmHg, certain medications (typically diuretics or ACE inhibitors) were temporarily suspended. These adjustments required regular reassessment to ensure blood pressure remained in target range without excessive lowering.
Medical Supervision Importance
The combination of fasting and antihypertensive medications necessitates professional oversight. In the comprehensive blood pressure fasting study, 70.3% of medicated patients normalized their blood pressure despite medication reduction—highlighting both the potential benefits and the need for careful supervision. Self-adjustment of medication without proper monitoring can lead to dangerous blood pressure fluctuations and is strongly discouraged across all research protocols.
Considerations for implementing fasting for people with high blood pressure
Medical Supervision
Proper medical oversight is essential for hypertensive individuals beginning fasting. The 1,610-participant study emphasized that pre-fasting health assessments should include comprehensive blood pressure readings, basic metabolic panel, and cardiovascular evaluation. For those with existing hypertension or on medications, directly supervised protocols showed the best safety profiles. The degree of supervision can be tailored to individual risk factors, with more intensive monitoring for those with severe hypertension or multiple medications.
Blood Pressure Monitoring
Consistent monitoring forms the cornerstone of safe implementation. The INTERFAST-MI trial protocol recommended measuring blood pressure at the same time each day to account for natural circadian variations. For hypertensive individuals, twice-daily measurements (morning and evening) using properly calibrated equipment provides the most reliable data. Recording readings in a structured format helps identify patterns and facilitates appropriate adjustments to fasting protocols or medications.
Complementary Dietary Approaches
Research demonstrates that certain dietary patterns enhance fasting’s blood pressure benefits. The Nutrition Journal randomized controlled trial found that combining time-restricted eating with the DASH diet (rich in fruits, vegetables, whole grains, and low-fat dairy) produced superior blood pressure reductions compared to either intervention alone. Similarly, reducing processed foods and sodium intake during eating windows amplifies fasting’s positive effects on blood pressure regulation.
Key Nutrients
Several nutrients demonstrate particular importance for blood pressure regulation during fasting periods. Clinical research highlights potassium as crucial for arterial flexibility, with leafy greens being an excellent source. Magnesium supports healthy blood vessel function and helps prevent muscle cramps during fasting. Vitamin D influences renin-angiotensin-aldosterone system regulation, while vitamin K2 helps prevent arterial calcification—both important factors in long-term blood pressure control.
Physical Activity
Movement during fasting enhances blood pressure benefits. The PLOS ONE study protocol incorporated daily physical activity, alternating between light walks and gentle exercises like stretching or yoga. Research suggests that moderate-intensity activity (able to talk but not sing during exercise) for 30 minutes most days provides optimal benefits without excessive stress during fasting periods. Vigorous exercise is typically not recommended, particularly during extended fasts, as it may increase physiological stress.
Sleep Optimization
Quality sleep significantly impacts blood pressure regulation. The PLOS ONE fasting study found that participants reported improved sleep quality, which correlated with better blood pressure outcomes. The percentage of days with self-reported restful sleep increased from approximately 70% at baseline to 88% during time-restricted eating. Maintaining consistent sleep schedules that align with natural circadian rhythms appears particularly important during fasting protocols.
Stress Management
Stress reduction techniques complement fasting’s blood pressure benefits. The study of 1,422 fasting participants documented significant improvements in well-being and self-reported relaxation scores, which corresponded with better blood pressure control. Regular mindfulness practices, breathing exercises, or other relaxation techniques help mitigate stress hormones that can otherwise counteract fasting’s positive effects on blood pressure regulation.
Comprehensive Approach
Research consistently shows that fasting works best as part of an integrated approach to blood pressure management. The Buchinger method combined fasting with appropriate hydration, light physical activity, stress reduction, and a structured refeeding phase—achieving impressive blood pressure reductions across various participant groups. This multifaceted approach addresses multiple pathways of hypertension simultaneously, creating synergistic effects that exceed what any single intervention could achieve alone.
Conclusion
Key Research Findings
The scientific evidence demonstrates that properly implemented fasting protocols can significantly impact blood pressure regulation. From the dramatic reductions seen in medically supervised water-only fasting (averaging 37 points systolic) to the more moderate but sustainable improvements with time-restricted eating (4-8 mmHg), various approaches have proven effective. Particularly noteworthy is fasting’s normalizing effect—substantial improvements for those with hypertension while causing minimal changes in those with already optimal readings.
Personalized Implementation
The research clearly shows that no single fasting protocol works best for everyone. Individual factors including baseline blood pressure, medication status, metabolic health, and personal preferences should guide protocol selection. For many with mild to moderate hypertension, time-restricted eating provides an optimal balance of effectiveness and sustainability. Those with more severe hypertension may benefit from more intensive approaches under appropriate supervision.
Safety First
While the safety profile of properly implemented fasting is impressive, certain precautions remain essential. Medical supervision is strongly recommended for those with existing hypertension, especially those taking medications. Individuals with certain conditions should avoid fasting entirely, including those with eating disorders, advanced kidney or liver disease, pregnancy, and severe underweight. Regular monitoring and knowing when to discontinue fasting are fundamental safety practices.
Part of an Integrated Approach
Fasting delivers the greatest cardiovascular benefits when implemented as part of a comprehensive approach. Research consistently shows enhanced results when fasting is combined with complementary strategies—nutrient-dense eating patterns, regular physical activity, stress management, and adequate sleep. The synergistic effects of these interventions target multiple pathways involved in blood pressure regulation simultaneously.
Natural Therapeutic Potential
Perhaps most significant is fasting’s ability to address underlying causes of hypertension rather than just managing symptoms. By improving insulin sensitivity, enhancing nitric oxide production, reducing inflammation, and beneficially restructuring the gut microbiome, fasting creates fundamental physiological changes that support long-term cardiovascular health. For many individuals, this approach offers a pathway to meaningful blood pressure improvement with fewer side effects than conventional treatments alone.
As research continues to evolve, the therapeutic potential of fasting for hypertension management becomes increasingly clear. When implemented with appropriate knowledge, guidance, and monitoring, fasting represents a powerful tool in the broader strategy for optimal cardiovascular health. The key lies in approaching this ancient healing tradition with modern scientific understanding—leveraging its benefits while respecting its limitations.
To access other content on the IFitCenter’s blog, you can use the following links:
References
- Dutzmann, J., Kefalianakis, Z., Kahles, F., Daniel, J. M., Gufler, H., Wohlgemuth, W. A., Knöpp, K., & Sedding, D. G. (2024). Intermittent Fasting After ST-Segment–Elevation Myocardial Infarction Improves Left Ventricular Function: The Randomized Controlled INTERFAST-MI Trial. Circulation: Heart Failure, 17(5). DOI: 10.1161/CIRCHEARTFAILURE.123.0109361
- Zhou, X., Lin, X., Yu, J., Yang, Y., Muzammel, H., Amissi, S., Schini-Kerth, V. P., Lei, X., Jose, P. A., Yang, J., & Shi, D. (2024). Effects of DASH diet with or without time-restricted eating in the management of stage 1 primary hypertension: a randomized controlled trial. Nutrition Journal, 17(23). DOI: 10.1186/s12937-024-00967-92
- Wang, W., Wei, R., Pan, Q., & Guo, L. (2022). Beneficial effect of time-restricted eating on blood pressure: a systematic meta-analysis and meta-regression analysis. Nutrition & Metabolism, 19(77). DOI: Not provided in the image3
- Isayeva, A., & Matiashova, L. (2022). Effect of one-day intermittent fasting on 24-hour blood pressure profile in hypertensive and normotensive patients with overweight and obesity. European Journal of Preventive Cardiology, 29(Supplement_1), zwac056.116. DOI: 10.1093/eurjpc/zwac056.116
- Gonzalez, J. E., & Cooke, W. H. (2022). Influence of an acute fast on ambulatory blood pressure and autonomic cardiovascular control. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology. DOI: 10.1152/ajpregu.00283.2021
- Al-Jafar, R., Themeli, M. Z., Zaman, S., Akbar, S., Lhoste, V., Khamliche, A., Elliott, P., Tsilidis, K. K., & Dehghan, A. (2021). Effect of Religious Fasting in Ramadan on Blood Pressure: Results From LORANS (London Ramadan Study) and a Meta-Analysis. Journal of the American Heart Association, 10(20). DOI: 10.1161/JAHA.120.021560
- Grundler, F., Mesnage, R., Michalsen, A., & Wilhelmi de Toledo, F. (2020). Blood Pressure Changes in 1610 Subjects With and Without Antihypertensive Medication During Long-Term Fasting. Journal of the American Heart Association, 9(23). DOI: 10.1161/JAHA.120.018649
- Kord-Varkaneh, H., Nazary-Vannani, A., Mokhtari, Z., et al. (2020). The Influence of Fasting and Energy Restricting Diets on Blood Pressure in Humans: A Systematic Review and Meta-Analysis. High Blood Press Cardiovasc Prev, 27, 271–280. DOI: 10.1007/s40292-020-00391-0
- Wilhelmi de Toledo, F., Grundler, F., Bergouignan, A., Drinda, S., & Michalsen, A. (2019). Safety, health improvement and well-being during a 4 to 21-day fasting period in an observational study including 1422 subjects. PLOS ONE. DOI: 10.1371/journal.pone.0209353
- Wilkinson, M. J., Manoogian, E. N. C., Zadourian, A., Navlakha, S., Panda, S., & Taub, P. R. (2020). Ten-Hour Time-Restricted Eating Reduces Weight, Blood Pressure, and Atherogenic Lipids in Patients with Metabolic Syndrome. Cell Metabolism, 31(1), P92-104.E5. DOI: 10.1016/j.cmet.2019.11.004



