You wake up with a throbbing headache and immediately wonder: “Is my blood pressure high?” This common belief—that headaches are a reliable warning sign of hypertension—is so widespread that it brings countless concerned patients through our doors every week. Yet surprisingly, scientific research tells a completely different story.
Contrary to popular belief, most people with high blood pressure never experience headaches at all. In fact, research suggests the relationship might even be reversed—with higher blood pressure sometimes associated with fewer headaches. This counterintuitive finding challenges everything most people think they know about “hypertension headaches.”
This is a common concern we address at IFitCenter. Many individuals assume they can rely on headaches as warning signals for high blood pressure, potentially missing the importance of regular monitoring. In this article, we’ll explore what medical science reveals about the connection between blood pressure and headaches, clarifying when a headache might genuinely indicate a blood pressure issue—and when it likely points to something else entirely.
The Relationship Between Blood Pressure and Headaches
What Science Really Shows About Hypertension Headaches
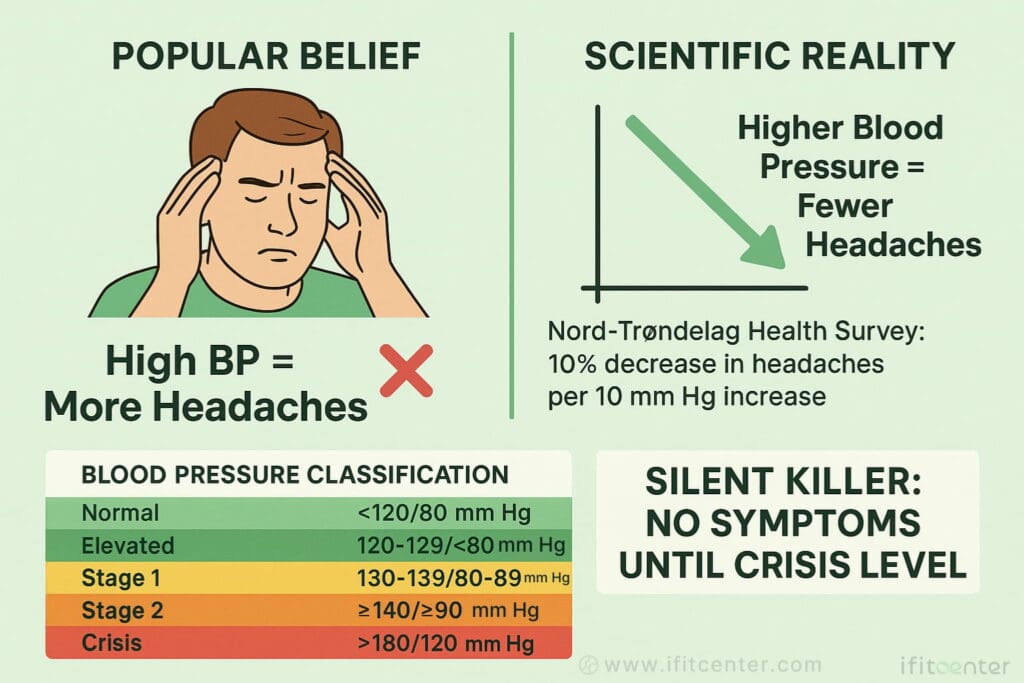
Blood pressure is measured with two numbers – like 120/80 mm Hg. The top number (systolic) measures pressure during heartbeats, while the bottom number (diastolic) measures pressure between beats. Understanding these readings helps determine if headaches might be BP-related.
Blood pressure falls into these categories:
- Normal: Below 120/80 mm Hg
- Elevated: 120-129/below 80 mm Hg
- Stage 1 Hypertension: 130-139/80-89 mm Hg
- Stage 2 Hypertension: 140+/90+ mm Hg
- Hypertensive Crisis: Above 180/120 mm Hg – medical emergency
Contrary to popular belief, research shows that headaches and high blood pressure often don’t go together. The Nord-Trondelag Health Survey found something surprising: people with higher BP actually reported fewer headaches than those with normal readings. For every 10 mm Hg increase in systolic pressure, headache prevalence decreased by 10%.
This contradicts what many believe about hypertension headaches. While most mild to moderate high BP doesn’t cause headaches, there’s an important exception: diastolic pressure may increase migraine risk, which we’ll explore later.
On the IFitCenter blog, we have prepared a free information database about various diseases, including high blood pressure, for you, our dear readers. By reviewing these resources, you will gain valuable information for controlling and preventing these conditions. To access the first part of the information, you can use the links below:
- blood pressure normal range
- high blood pressure symptoms
- blood pressure chart
- hypertension causes
- how to measure blood pressure at home
- breathing exercises to lower blood pressure
- foods to avoid with high blood pressure
High BP: The Silent Danger
High blood pressure earned its “silent killer” nickname because it typically causes no symptoms – including headaches – while damaging your cardiovascular system. This absence of warning signs makes regular BP monitoring essential.
Many people mistakenly rely on headaches to alert them to high blood pressure. This dangerous misconception leads many to assume their BP is normal simply because they don’t have headache symptoms, potentially delaying diagnosis until significant damage occurs.
Why does this headache-hypertension myth persist? Several factors contribute:
- People with newly diagnosed hypertension often retroactively attribute past headaches to high BP
- Hypertensive crisis (180/120+ mm Hg) can cause severe headaches, reinforcing the misconception
- Stress can trigger both headaches and temporary BP spikes, creating a false connection
- The belief continues spreading through popular health discussions
This misunderstanding has real consequences. Waiting for a headache before checking your blood pressure could mean missing early treatment opportunities. Similarly, blaming frequent headaches on hypertension might lead you to overlook their actual cause.
In the following sections, we’ll explore when blood pressure genuinely does cause headaches and how to recognize these specific situations.
“Many patients are surprised when I tell them that mild to moderate hypertension rarely causes headaches. In fact, research shows quite the opposite—people with higher blood pressure often report fewer headaches than those with normal readings. This misconception leads many to delay proper blood pressure monitoring because they’re waiting for a headache that may never come. Regular monitoring remains essential regardless of symptoms.”
Dr. Babak Jamalian, Family Physician.
When High Blood Pressure DOES Cause Headaches
Hypertensive Crisis and Headache
While everyday high blood pressure rarely causes headaches, there’s an important exception: hypertensive crisis. This dangerous condition occurs when blood pressure suddenly spikes to 180/120 mm Hg or higher, creating a genuine medical emergency.
Hypertensive crisis comes in two forms:
- Hypertensive urgency: Extremely high BP without immediate organ damage
- Hypertensive emergency: Extremely high BP with evidence of organ damage
During a hypertensive crisis, the extreme pressure can cause blood to leak from blood vessels in the brain, creating swelling. Since the brain sits within the skull with no room to expand, this swelling creates intense pressure that triggers a severe headache.
BP Headache Symptoms
Headaches caused by severe high blood pressure differ from ordinary headaches. Recognizing these differences could potentially save a life.
Typical hypertension headache characteristics include:
- Location: Usually affects both sides of the head
- Sensation: Pulsating or throbbing pain that worsens with physical activity
- Timing: Often occurs upon waking in the morning
- Duration: Can persist until blood pressure is lowered
When a hypertensive headache strikes, it rarely comes alone. Watch for these additional warning signs:
- Visual disturbances (blurred vision or seeing spots)
- Chest pain or tightness
- Shortness of breath
- Nausea or vomiting
- Confusion or difficulty speaking
- Numbness or weakness
If you experience a sudden, severe headache along with any of these symptoms, check your blood pressure immediately if possible. Readings above 180/120 mm Hg require emergency medical attention – don’t attempt to lower your blood pressure at home, as reducing it too quickly can be dangerous.
Diastolic Blood Pressure and Migraine
The Bottom Number Matters for Migraines
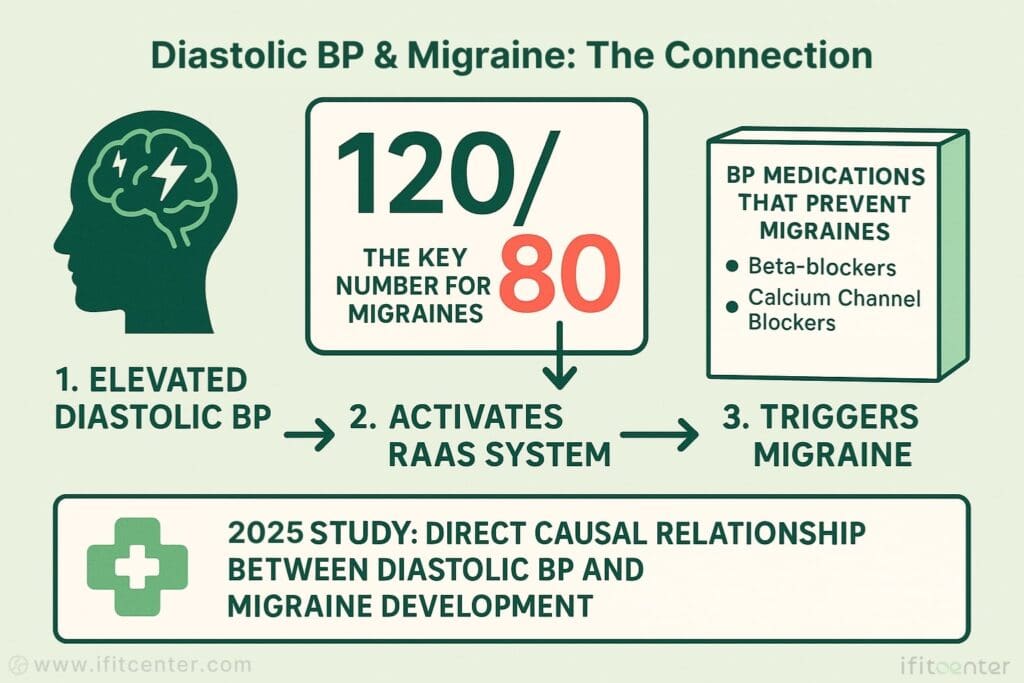
While systolic pressure (the top number) shows an inverse relationship with headaches, recent research reveals something surprising about diastolic pressure (the bottom number): it may actually trigger migraines in some people.
A comprehensive 2025 study published in the Journal of Translational Medicine found a significant causal relationship between diastolic blood pressure and migraine development. Unlike the top number, higher diastolic readings were associated with increased migraine risk.
The study showed a direct positive relationship between diastolic BP and migraine development. For each slight increase in diastolic pressure, migraine risk increased as well – creating a linear pattern that suggests a genuine connection rather than coincidence.
How Diastolic Pressure Triggers Migraines
Why does diastolic pressure specifically affect migraines? Research points to several biological mechanisms:
- The RAAS System: Diastolic hypertension activates the renin-angiotensin-aldosterone system, triggering inflammation in blood vessels
- Endothelial Dysfunction: Elevated diastolic pressure damages the inner lining of blood vessels
- Cortical Spreading Depression: These vascular changes can trigger waves of brain activity that cause migraine pain
This connection explains why certain blood pressure medications effectively prevent migraines. Beta-blockers, angiotensin receptor blockers, and calcium channel blockers have all shown benefits in reducing migraine frequency.
The 2023 meta-analysis of blood pressure medications for migraine prevention found that all major classes reduced monthly headache days, with calcium channel blockers showing the largest reduction. These medications appear to work by addressing the underlying vascular mechanisms connecting diastolic pressure and migraine pain.
If you experience migraines and have elevated diastolic pressure, discussing this connection with your healthcare provider could open new treatment possibilities that address both conditions simultaneously.
“While most people focus on the top number in blood pressure readings, recent research reveals something fascinating: it’s actually the bottom number—diastolic pressure—that shows a stronger connection to migraine development. This explains why certain blood pressure medications are so effective for preventing migraines. For patients suffering from both conditions, addressing diastolic pressure specifically may provide relief from both issues simultaneously.”
Dr. Babak Jamalian, Family Physician.
Low Blood Pressure and Headaches
Low BP Headache Causes
While much attention focuses on high blood pressure, low blood pressure (hypotension) can also trigger headaches. These low BP headaches often have distinctive patterns that differ from other headache types.
Hypotension headaches typically occur when blood pressure drops below 90/60 mm Hg. The most common type is related to orthostatic hypotension – a sudden drop in blood pressure that happens when you change positions, particularly when standing up quickly after sitting or lying down.
When you stand up, gravity naturally pulls blood downward. Normally, your body compensates by constricting blood vessels and increasing heart rate. But when this mechanism fails, blood pressure drops suddenly, reducing blood flow to the brain and triggering a headache.
Recognizing Low Blood Pressure Headaches
Low BP headaches have specific characteristics that help distinguish them from other types:
- Position-dependent: Worse when standing, better when lying down
- Timing: Often occur in the morning or after sitting/lying for extended periods
- Location: Typically felt across the forehead or at the back of the head
- Accompanying symptoms: Dizziness, lightheadedness, blurred vision, weakness, fatigue
Unlike hypertension headaches, which are rare except during crisis, low blood pressure frequently causes headaches as a primary symptom. This happens because the brain receives insufficient blood flow, triggering pain receptors.
To access the second section of blood pressure articles, I invite you to use the links below:
- dash diet for hypertension
- Best foods for high blood pressure
- untreated high blood pressure
- how does obesity raise blood pressure?
- fasting for lowering blood pressure
Managing Headaches from Low BP
Addressing low blood pressure headaches involves several practical approaches:
- Stay hydrated: Dehydration lowers blood volume and worsens hypotension. Aim for at least 8 glasses of water daily.
- Add salt: Unlike with high blood pressure, people with low BP often benefit from slightly increased sodium intake (consult your doctor first).
- Position changes: Rise slowly from sitting or lying positions. Sit on the edge of the bed for a minute before standing.
- Compression garments: Support stockings help prevent blood pooling in the legs.
- Smaller, frequent meals: Large meals can lower blood pressure as blood diverts to digestion.
For persistent low BP headaches, medical evaluation is important. Certain medications, heart conditions, endocrine disorders, or neurological problems can cause hypotension and should be properly diagnosed.
While most low blood pressure headaches can be managed with lifestyle adjustments, they should never be ignored – especially if they’re new, severe, or accompanied by unusual symptoms. These could indicate more serious underlying conditions that require medical attention.
Common Headache Types Often Misattributed to Blood Pressure
Tension Headaches vs BP Headaches
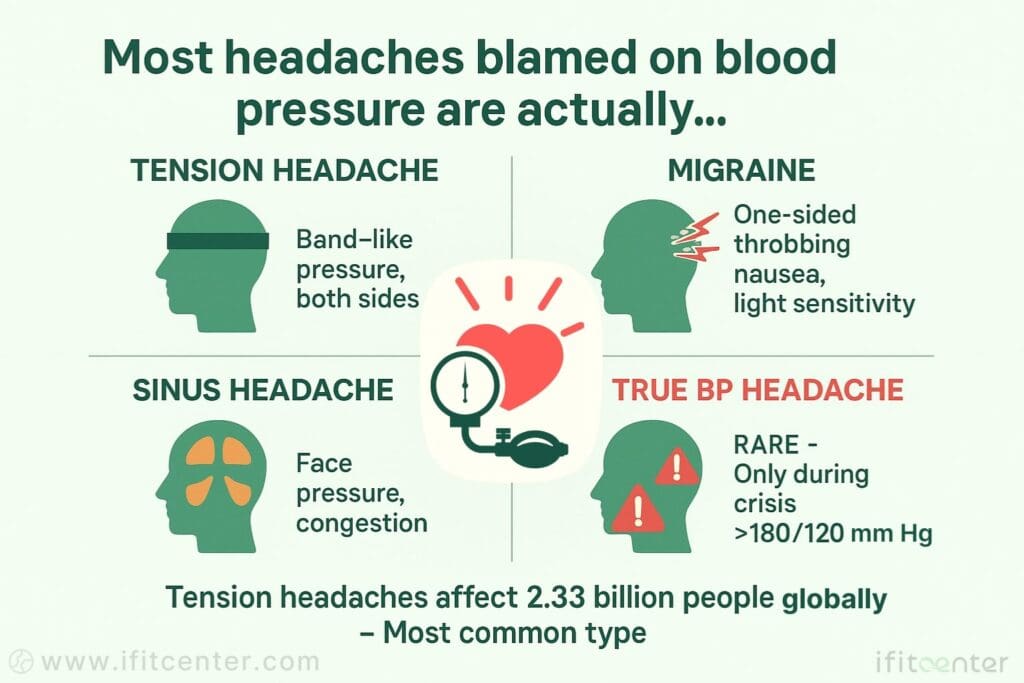
Tension-type headaches are the most prevalent primary headache globally – affecting approximately 2.33 billion people – and are frequently mistaken for blood pressure-related headaches. Understanding the key differences can prevent unnecessary worry.
Tension headaches typically cause:
- Sensation: Dull, pressing, band-like tightness (not pulsating)
- Location: Both sides of the head, often starting at the back of the head or neck
- Duration: 30 minutes to several days
- Triggers: Stress, poor posture, inadequate sleep, eye strain
The confusion arises because stress can temporarily raise blood pressure while simultaneously triggering tension headaches. This creates a misleading association between the two conditions, even though tension headaches occur regardless of blood pressure readings.
Migraine and Other Headache Types
Several other headache types are commonly misattributed to blood pressure issues:
- Migraine: Intense throbbing pain (usually one-sided), often with nausea, sensitivity to light/sound, and sometimes visual disturbances. While diastolic blood pressure may influence migraine development, most migraines aren’t directly caused by blood pressure fluctuations.
- Sinus headaches: Pain concentrated around the sinus areas (forehead, bridge of nose, cheekbones) that worsens with bending forward. Often accompanied by nasal congestion or discharge.
- Medication overuse headaches: Paradoxically, pain relievers taken too frequently (more than 15 days per month) can cause chronic headaches. Blood pressure medications rarely cause this type of headache.
Ironically, some blood pressure medications can cause headaches as a side effect, further complicating the relationship. Beta-blockers, calcium channel blockers, and diuretics occasionally trigger headaches, particularly when first starting treatment.
Distinguishing between these headache types requires careful attention to triggers, patterns, and accompanying symptoms. When in doubt, maintaining a headache diary that records blood pressure readings alongside headache episodes can help identify (or rule out) connections.
Conclusion
The relationship between blood pressure and headaches is more complex than commonly believed. Here’s what the evidence tells us:
- Most mild to moderate high blood pressure does NOT cause headaches
- Hypertensive crisis (180/120+ mm Hg) can trigger severe, distinctive headaches requiring emergency care
- Diastolic blood pressure specifically may influence migraine development
- Low blood pressure frequently causes position-dependent headaches
- Many common headache types are mistakenly attributed to blood pressure issues
Understanding these distinctions matters for your health. Don’t rely on headaches (or their absence) to gauge your blood pressure status. Regular monitoring remains the only reliable way to track your blood pressure.
If you experience frequent or severe headaches, consider keeping a journal that tracks symptoms alongside blood pressure readings. This information will help healthcare providers determine whether your headaches are truly blood pressure-related or have another cause entirely.
Remember that both high blood pressure and chronic headaches are treatable conditions. With proper diagnosis and management, you can effectively address both issues and improve your quality of life. When in doubt, seek professional medical evaluation – never attempt to self-diagnose the relationship between your blood pressure and headaches.
To access other content on the IFitCenter’s blog, you can use the following links:
References
- Xiao, G., Huang, Z., Lan, Q., Hu, J., Shi, H., Chen, Y., Zhou, C., Chenghua, L., & Zhou, B. (2025). Evidence supporting the role of hypertension in the onset of migraine. Journal of Translational Medicine, 23, 474. DOI: 10.1186/s12967-025-06187-x
- Mazzacane, F., Vaghi, G., Cotta Ramusino, M., Perini, G., & Costa, A. (2024). Arterial hypertension in the chronic evolution of migraine: bystander or risk factor? An overview. Journal of Headache Pain, 25(1), 13. DOI: 10.1186/s10194-024-01720-7
- Qin, L., Song, P., Li, X., Yang, L., Xu, F., Zhu, X., Cai, L., Hu, G., Sun, W., Zhang, Y., & Zhang, L. (2024). Tension-Type Headache Management: A Systematic Review and Network Meta-analysis of Complementary and Alternative Medicine. Pain Therapy, 13(4), 691-717. DOI: 10.1007/s40122-024-00600-x
- Carcel, C., Haghdoost, F., Shen, J., Nanda, P., Bai, Y., Atkins, E., Torii-Yoshimura, T., Clough, A. J., Davies, L., Cordato, D., Griffiths, L. R., Balicki, G., Wang, X., Vidyasagar, K., Malavera, A., Anderson, C. S., Zagami, A. S., Delcourt, C., & Rodgers, A. (2023). The effect of blood pressure lowering medications on the prevention of episodic migraine: A systematic review and meta-analysis. Cephalalgia, 43(6), 3331024231183166. DOI: 10.1177/03331024231183166
- Mohammadi, M., Ayoobi, F., Khalili, P., Soltani, N., La Vecchia, C., & Vakilian, A. (2021). Relation of hypertension with episodic primary headaches and chronic primary headaches in population of Rafsanjan cohort study. Scientific Reports, 11, 24071. DOI: 10.1038/s41598-021-03377-7
- Fagernæs, C. F., Heuch, I., Zwart, J-A., Winsvold, B. S., Linde, M., & Hagen, K. (2015). Blood pressure as a risk factor for headache and migraine: a prospective population-based study. European Journal of Neurology, 22(1), 156-62, e10-1. DOI: 10.1111/ene.12547




