Did you know that prediabetes affects 374 million adults worldwide—yet a staggering 90% have no idea they’re living with this condition? Even more alarming, studies show that without intervention, up to 70% of people with prediabetes will eventually develop type 2 diabetes. This silent metabolic condition represents a critical window of opportunity—a chance to reverse course before pancreatic damage occurs.
Prediabetes isn’t merely a “maybe someday” warning or a mild concern. It’s your body’s urgent alert system signaling that your cells are already struggling to process glucose properly. With blood sugar levels between 100-125 mg/dL or HbA1c between 5.7-6.4%, prediabetes sits in that crucial middle ground—no longer normal, but not yet diabetic.
At IFitCenter, we’re committed to providing comprehensive education on metabolic health conditions like prediabetes. In this expert guide, we’ll explore what prediabetes really means for your body, how to recognize its subtle warning signs, and most importantly, evidence-based strategies to reverse this condition before it progresses to diabetes.
What is Prediabetes? Understanding the Basics
Imagine your body as a car with a sophisticated fuel system. In a properly functioning car, when you add fuel (food), the fuel gauge (blood sugar) rises temporarily, then returns to normal as the fuel is distributed to power your engine. Prediabetes is like having a fuel system that’s starting to malfunction—your fuel gauge stays elevated longer than it should after refueling, but your car can still run. If left unaddressed, this problem eventually damages the system permanently (diabetes), where your fuel gauge remains stuck at high levels regardless of what you do.
From a scientific perspective, prediabetes is a metabolic condition where blood glucose levels are consistently above normal but not yet high enough to meet the criteria for diabetes. It represents a critical warning stage in the progression toward type 2 diabetes, but importantly, it’s a stage where the process is still reversible.
“The critical distinction between prediabetes and diabetes isn’t just in the numbers—it’s in the reversibility. Prediabetes represents cellular insulin resistance with functioning beta cells, while diabetes indicates irreversible pancreatic damage. This is why identifying prediabetes creates such a valuable window of opportunity. When we see patients with fasting glucose between 100-125 mg/dL or HbA1c between 5.7-6.4%, we’re not just observing elevated numbers; we’re witnessing a metabolic state that can still be completely restored to normal through targeted interventions.”
Dr. Babak Jamalian, Family Physician Specialist.
The Three Stages of Blood Sugar Control
Your body’s relationship with glucose moves through three distinct stages:
- Normal glucose regulation: After eating, your blood sugar rises temporarily. Your pancreas releases insulin, which acts like a key, unlocking cells so they can absorb glucose from your bloodstream. Your blood sugar quickly returns to baseline levels (below 100 mg/dL when fasting).
- Prediabetes: Your cells begin developing resistance to insulin—like the locks on your cells are starting to jam. Your pancreas compensates by producing 5-7 times more insulin than normal. This keeps your blood sugar from rising too high, but the strain begins to wear on your pancreatic cells. Your fasting blood sugar stays in the 100-125 mg/dL range.
- Diabetes: After years of overworking, your pancreas can no longer produce enough insulin to overcome the resistance. The insulin “keys” dwindle in number, and your blood sugar remains consistently elevated above 126 mg/dL. At this point, the damage to your pancreatic beta cells is largely irreversible.
On the IFitCenter blog, we have prepared a comprehensive guide for pre-diabetes, completely free of charge. Using this guide will make controlling and preventing pre-diabetes much easier for you or your loved ones. To access the first part of the content, simply use the links below:
- signs of prediabetes
- test for prediabetes
- prediabetes can be reversed
- how to reverse prediabetes naturally?
- prediabetes weight loss
- prediabetes diet foods to avoid
Diagnostic Prediabetes Criteria: Understanding the Prediabetes Numbers
How do medical professionals distinguish between these three states? They rely on specific diagnostic criteria:
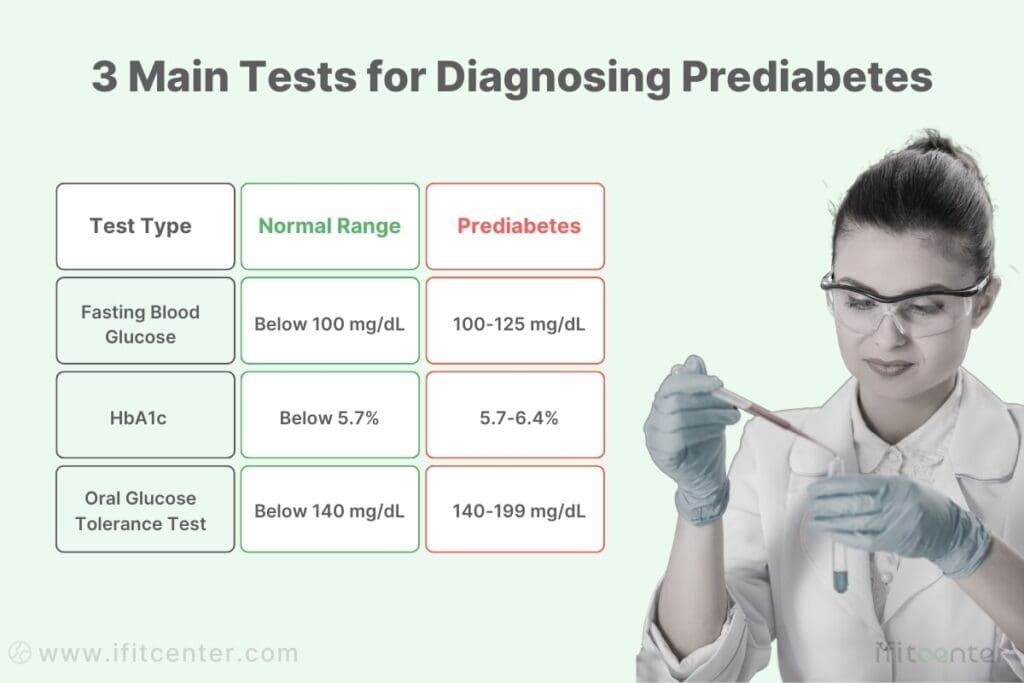
These numbers aren’t arbitrary—they represent thresholds where research has identified significant changes in how your body processes glucose and corresponding increases in health risks.
Why Prediabetes Often Goes Undetected
One reason prediabetes frequently remains undiagnosed is that your body is remarkably adaptable. During the prediabetic stage, your pancreas works overtime to compensate for insulin resistance, keeping your blood sugar from rising to obviously problematic levels. This compensation can continue for 10-15 years before your pancreas begins to fail.
Think of it like a championship runner who’s developing a leg injury. At first, they can still finish races by compensating with altered technique and extra effort. Their times might be slightly slower, but they’re still completing the course. The true extent of the injury only becomes obvious when they can no longer compensate, and their performance dramatically declines.
Unfortunately, by the time blood sugar levels rise to diabetic levels, significant damage has already occurred in multiple body systems. This is why early detection of prediabetes is so crucial—it allows for intervention while the process is still fully reversible.
The Critical Window of Opportunity
What makes prediabetes fundamentally different from diabetes is its reversibility. When detected early, prediabetes can be completely reversed through lifestyle modifications. Research shows that appropriate interventions can reduce progression to diabetes by up to 58%—significantly better than medication-only approaches, which typically reduce progression by about 31%.
This reversibility makes prediabetes detection a critical public health priority. It represents a window of opportunity where relatively modest changes can prevent the development of a chronic, progressive disease that requires lifelong management.
Warning Signs and Symptoms of Prediabetes
Prediabetes often develops silently, gradually affecting your body’s systems for years before blood sugar levels rise enough to trigger obvious symptoms. Recognizing the early warning signs can provide a critical opportunity for intervention before progression to diabetes occurs. Research indicates that 90% of people with prediabetes remain undiagnosed, largely because these subtle symptoms are easily overlooked or attributed to other causes.
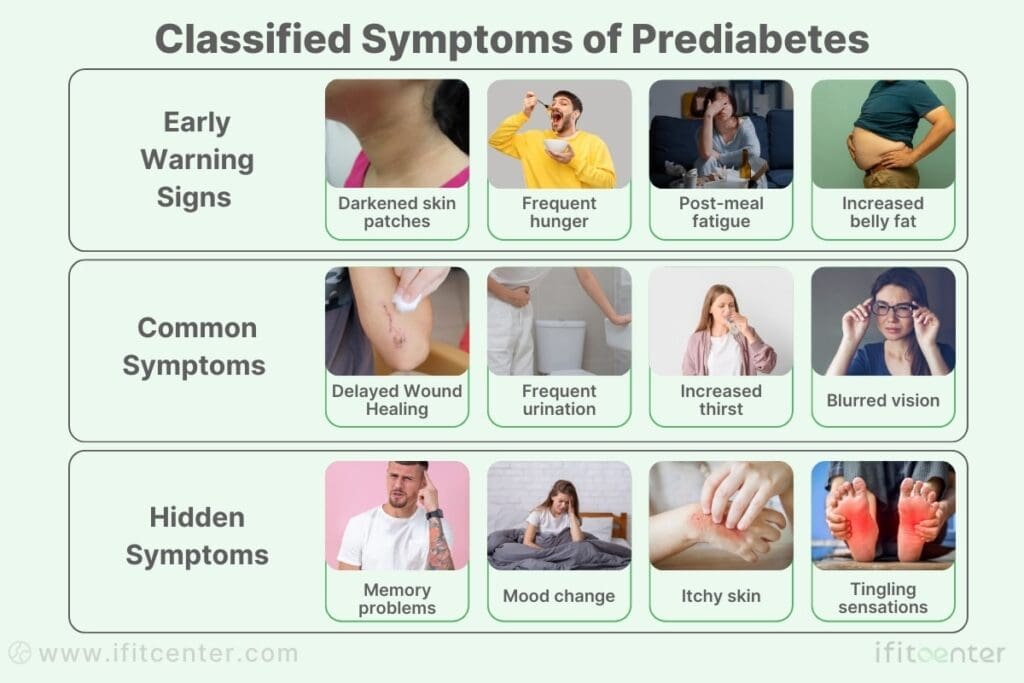
Early Warning Signs of Prediabetes to Watch For
The earliest indicators of prediabetes are often dismissed as normal aging, stress, or lifestyle factors. However, when these signs appear together, they merit attention:
- Darkened skin patches (acanthosis nigricans): Velvety dark patches in skin folds, particularly around the neck, armpits, or groin areas. This discoloration signals insulin resistance, as elevated insulin levels can stimulate skin cell growth in certain areas.
- Frequent hunger: The inability to go 2-3 hours without feeling hungry, despite adequate caloric intake. This occurs because insulin resistance prevents glucose from effectively entering cells, leaving them “starving” despite available fuel in the bloodstream.
- Post-meal fatigue: Feeling unusually tired after eating, especially meals high in carbohydrates. This happens as your body struggles to process the glucose load, leading to energy fluctuations.
- Increased belly fat: Fat accumulation around the midsection, even if you’re not overweight elsewhere. Abdominal fat is both a cause and consequence of insulin resistance, creating a challenging cycle.
Common Symptoms of Prediabetes Explained
As prediabetes progresses, more noticeable symptoms may develop. These represent your body’s increasing difficulty in managing blood glucose:
- Slow healing: Cuts, bruises, or infections taking longer to heal. Elevated blood sugar impairs circulation and weakens immune response, slowing the healing process.
- Frequent urination: Particularly noticeable at night. As blood glucose rises, your kidneys work harder to filter and absorb the excess glucose. When they can’t keep up, this glucose is excreted into the urine, drawing water along with it and causing more frequent urination.
- Increased thirst: A natural response to the fluid loss from frequent urination. This creates a cycle of drinking and urinating that can be an important clinical indicator.
- Blurred vision: Fluctuating blood sugar levels can affect fluid levels in your eye tissues, including the lens, causing temporary vision changes.
Hidden Symptoms of Prediabetes Many People Miss
Some prediabetes symptoms are particularly easy to overlook because they affect areas not typically associated with blood sugar in the public mind:
- Memory problems: Subtle cognitive changes such as forgetfulness or difficulty concentrating. Research shows that insulin plays important roles in brain function, and insulin resistance can affect memory formation and neural health.
- Mood changes: Increased irritability, anxiety, or depressive symptoms. Blood sugar fluctuations can affect neurotransmitter balance and overall brain function.
- Dry mouth: Beyond just thirst, a persistently dry mouth occurs as your body attempts to conserve fluid.
- Itchy skin: Poor circulation and inflammatory responses to elevated blood sugar can cause generalized itchiness.
- Tingling sensations: Particularly in the feet and hands. Even moderately elevated blood sugar can begin affecting nerves, though full neuropathy typically doesn’t develop until diabetes progresses.
When Symptoms of Prediabetes Indicate Need for Medical Attention
While prediabetes itself rarely constitutes a medical emergency, certain symptom patterns warrant prompt medical evaluation:
- Symptom clusters: Experiencing three or more symptoms simultaneously, particularly if they include darkened skin patches, frequent urination, increased thirst, and persistent fatigue.
- Family history plus symptoms: Any symptoms in someone with a strong family history of type 2 diabetes (parents or siblings with the condition) deserve medical attention.
- Rapid symptom onset: Symptoms that develop suddenly or worsen quickly could indicate more advanced metabolic dysfunction.
- Persistent symptoms: Signs that don’t improve with basic lifestyle modifications like reduced sugar intake or increased activity.
It’s important to note that while individual symptoms might have alternative explanations, the constellation of multiple symptoms significantly increases the likelihood of prediabetes. According to research published in Diabetes Care, people presenting with a combination of abdominal obesity, darkened skin patches, and frequent thirst have up to an 89% probability of having prediabetes or early diabetes when tested.
Early detection through symptom recognition offers a critical opportunity to reverse prediabetes before permanent pancreatic damage occurs. Remember, the transition from prediabetes to diabetes represents a shift from a reversible condition to one that typically requires lifelong management.
Reversing Prediabetes—Beyond Just Diet and Exercise
Many people believe cutting sugar and exercising more is enough to reverse prediabetes. But the truth is prediabetes is a metabolic condition that requires a deeper approach—balancing insulin resistance, inflammation, and hormonal health.
At iFitCenter, we take a comprehensive approach to prediabetes reversal by offering:
✔ Advanced metabolic assessments to pinpoint the root causes of your insulin resistance
✔ Personalized nutrition plans designed for sustainable blood sugar control
✔ Expert medical guidance to track progress and ensure long-term success
Prediabetes is a critical stage where small changes can have life-changing results. Don’t wait for diabetes to develop—start your transformation today!
Prediabetes Blood Sugar Levels: Prediabetes Numbers
Blood sugar levels are the definitive measure for diagnosing prediabetes. Understanding these numbers is crucial, as they provide clear indicators of your metabolic health status and potential risk for diabetes progression. Research shows that each incremental rise in blood glucose carries corresponding increases in health risks, making precise measurement essential for proper evaluation.
To access the second part of pre-diabetes content, I invite you to use the links below:
- supplements for prediabetes
- fasting with prediabetes
- difference between prediabetes and diabetes
- can vitamin d deficiency cause prediabetes?
- prediabetes and obesity connection
- diabetes numbers explained
- hba1c testing
- Best cooking oil for heart and blood pressure
Prediabetes Blood Sugar Levels vs. Normal Ranges
Blood sugar exists on a spectrum, with clear threshold values differentiating between normal functioning, prediabetes, and diabetes. These ranges aren’t arbitrary—they’re established based on extensive research showing where metabolic changes and health risks significantly increase.
| Blood Sugar Measurement | Normal Range | Prediabetes Range | Diabetes Range |
|---|---|---|---|
| Fasting Plasma Glucose (FPG) | Below 100 mg/dL (5.6 mmol/L) | 100-125 mg/dL (5.6-6.9 mmol/L) | 126 mg/dL or higher (7.0 mmol/L or higher) |
| Hemoglobin A1c (HbA1c) | Below 5.7% | 5.7-6.4% | 6.5% or higher |
| Oral Glucose Tolerance Test (OGTT) 2-hour reading | Below 140 mg/dL (7.8 mmol/L) | 140-199 mg/dL (7.8-11.0 mmol/L) | 200 mg/dL or higher (11.1 mmol/L or higher) |
What’s particularly important to understand is that even within the prediabetes range, risk isn’t uniform. Research published in the American Diabetes Association’s Standards of Care indicates that someone with a fasting glucose of 124 mg/dL has a significantly higher risk of progression to diabetes than someone at 100 mg/dL, despite both being categorized as prediabetic.
Different Types of Prediabetes Tests and Their Significance
Multiple testing methods exist for evaluating blood glucose levels, each offering different insights into your metabolic health:
- Fasting Plasma Glucose (FPG): Measures your blood sugar after at least 8 hours without food or drink (except water). This test reveals your body’s baseline ability to manage glucose without the influence of recent food intake. A reading between 100-125 mg/dL indicates prediabetes. The FPG is commonly used due to its simplicity but may miss some cases of impaired glucose tolerance.
- Hemoglobin A1c (HbA1c): Measures the percentage of hemoglobin proteins in your blood that have glucose attached to them. Since red blood cells live approximately 3 months, this test provides an average of your blood sugar levels over the past 2-3 months rather than a single point in time. An A1c between 5.7-6.4% indicates prediabetes. This test doesn’t require fasting and provides a more stable measurement less affected by daily fluctuations.
- Oral Glucose Tolerance Test (OGTT): Evaluates how efficiently your body processes glucose. After fasting overnight, you drink a solution containing 75 grams of glucose, and your blood sugar is measured both before and 2 hours after consumption. A 2-hour reading between 140-199 mg/dL indicates prediabetes. The OGTT can identify abnormal glucose processing that might be missed by other tests and is considered the most sensitive for detecting early-stage prediabetes.
Research indicates that these tests don’t always identify the same individuals as having prediabetes. A study published in Diabetes Care found that among people with prediabetes, only 32% met all three diagnostic criteria, while 38% had discordant results across different tests. This highlights the importance of comprehensive testing when prediabetes is suspected.
How to Interpret Your Prediabetes Test Results
Receiving test results can be confusing without proper context. Here’s what your numbers mean in practical terms:
- Borderline Results: Values near cutoff points (e.g., fasting glucose of 99-101 mg/dL) warrant additional testing, as day-to-day variations can affect readings. If your results fall in this gray zone, consider repeating the test or using a different testing method for confirmation.
- Trend Analysis: A single elevated reading is less concerning than consistent increases over time. If your fasting glucose has risen from 90 mg/dL to 115 mg/dL over several years, this indicates progressive insulin resistance even if both values fall in different categories.
- Test Discordance: If one test indicates prediabetes while another shows normal results, the American Diabetes Association recommends treating the condition as present and taking preventive measures rather than waiting for multiple tests to confirm.
- Personal Context: Results should be interpreted in light of your unique risk factors. A “high-normal” reading in someone with multiple risk factors (family history, excess weight, sedentary lifestyle) warrants closer monitoring than the same reading in someone without these factors.
It’s worth noting that standard reference ranges are established for general populations. Certain groups—including pregnant women, children, and some ethnic populations—may have different thresholds. For instance, research indicates that Asian Americans may develop insulin resistance at lower BMI and blood glucose levels than Caucasian populations.
The Importance of Regular Blood Sugar Monitoring in Prediabetes
Regular monitoring serves multiple crucial purposes beyond initial diagnosis:
- Early Intervention: Monitoring allows detection of deteriorating glucose control before progression to diabetes. Research shows that early intervention can reduce progression to diabetes by up to 58%.
- Personalized Feedback: Regular testing provides immediate feedback on how specific lifestyle changes affect your blood sugar. This creates a clear cause-and-effect understanding that can motivate continued positive behaviors.
- Pattern Recognition: Multiple readings over time reveal patterns that single tests miss. For example, seasonal variations, stress-related fluctuations, or gradual improvements in response to lifestyle modifications become apparent only through consistent monitoring.
- Risk Stratification: Monitoring helps determine if you’re at the lower or higher end of the prediabetes spectrum, which affects treatment approaches and urgency. Someone with an A1c of 6.3% requires more aggressive intervention than someone at 5.8%.
For most people with prediabetes, experts recommend testing at least annually, with more frequent monitoring (every 3-6 months) for those at higher risk of progression or actively implementing lifestyle changes. Research indicates that this regular feedback loop significantly improves long-term outcomes by reinforcing beneficial behaviors and enabling timely adjustments when needed.
Understanding your blood sugar levels provides the concrete data needed to take control of your metabolic health. With proper interpretation and regular monitoring, you can track your progress, make informed decisions, and potentially reverse prediabetes before it progresses to diabetes.
What Causes Prediabetes?
Understanding what causes prediabetes is essential for effective prevention and treatment. At its core, prediabetes develops when your body’s relationship with insulin—the hormone responsible for regulating blood sugar—becomes dysfunctional. This complex condition results from a combination of physiological processes, risk factors, lifestyle choices, and genetic influences working together.
“What fascinates me about prediabetes is how the body compensates for insulin resistance without our awareness. Many patients are surprised to learn their pancreas has been producing 5-7 times more insulin than normal, sometimes for a decade, before showing clinical signs of glucose dysregulation. This metabolic adaptation explains why someone can develop significant insulin resistance without noticeable blood sugar elevation. It also explains why apparently ‘sudden’ diabetes diagnoses are actually the endpoint of a long-developing process—one we can detect and reverse if we know what early warning signs to look for.”
Dr. Babak Jamalian, Family Physician Specialist.
The Science Behind Insulin Resistance in Prediabetes
Insulin resistance is the primary mechanism underlying prediabetes. Under normal circumstances, when you consume food, your blood glucose levels rise, triggering your pancreas to release insulin. This insulin acts like a key, unlocking cells to allow glucose entry, which then powers cellular functions while keeping blood sugar levels balanced.
In prediabetes, this system begins to falter. Your cells gradually become less responsive to insulin’s signals—a state known as insulin resistance. Think of it as your cells “ignoring” the insulin message, like developing earplugs against a repeated signal. Research shows this resistance occurs at the cellular receptor level, where the normal insulin signaling cascade becomes disrupted.
In response to this resistance, your pancreas initially compensates by producing more insulin—up to 5-7 times the normal amount. This explains why many people with prediabetes actually have elevated insulin levels despite their rising blood sugar. It’s like shouting louder to be heard over background noise. For a period that can last 10-15 years, this compensation keeps blood sugar levels from rising dramatically, but the strain on your pancreas is significant.
Eventually, the insulin-producing beta cells in the pancreas begin to fatigue under this constant demand. As your pancreas struggles to maintain this heightened insulin production, blood sugar levels begin to rise, crossing from normal into the prediabetic range.
What makes insulin resistance particularly concerning is that it affects multiple body systems simultaneously. Insulin doesn’t just regulate blood sugar—it influences fat storage, vascular function, inflammatory responses, and even neurocognitive processes. This explains why prediabetes is associated with increased abdominal fat, elevated blood pressure, and other metabolic changes beyond just elevated blood sugar.
Risk Factors That Cause Prediabetes

Several key risk factors significantly increase your likelihood of developing prediabetes. Understanding these can help identify who might benefit most from early screening and intervention:
- Age: Risk increases significantly after age 45. Research indicates that cellular insulin sensitivity naturally decreases with age, making older adults more susceptible.
- Weight status: Carrying excess weight, particularly around the abdomen, is strongly linked to insulin resistance. Visceral fat (fat surrounding internal organs) is metabolically active, releasing inflammatory compounds that directly interfere with insulin signaling.
- Physical inactivity: Regular muscle contraction plays a crucial role in glucose metabolism. Without adequate physical activity, muscles become less efficient at absorbing glucose, even in the presence of insulin.
- Past gestational diabetes: Women who developed diabetes during pregnancy face a 35-60% higher risk of developing prediabetes and type 2 diabetes later in life.
- Polycystic ovary syndrome (PCOS): This hormonal disorder affects up to 10% of women and creates a 3-7 times higher risk of developing prediabetes due to its association with insulin resistance.
- Sleep disorders: Chronic sleep deprivation and conditions like sleep apnea are linked to impaired glucose metabolism, with research showing that even one week of insufficient sleep can induce temporary insulin resistance.
- Certain medications: Some drugs, including certain antipsychotics, beta-blockers, and corticosteroids, can interfere with insulin sensitivity or increase blood glucose levels.
It’s important to note that risk factors often cluster together, creating a compounding effect. For example, someone with both a family history of diabetes and excess abdominal fat faces significantly higher risk than someone with just one of these factors.
Lifestyle Factors That Contribute to Prediabetes
Our modern lifestyle has created conditions particularly conducive to developing prediabetes. Several specific lifestyle factors have been scientifically linked to increased risk:
- Dietary patterns: Diets high in refined carbohydrates and added sugars produce repeated blood glucose spikes, eventually contributing to insulin resistance. Research shows the average person consumes approximately 31 teaspoons of sugar daily—far exceeding the recommended maximum of 6-9 teaspoons. Over time, this excessive carbohydrate intake forces the pancreas to continuously release insulin, contributing to cellular resistance.
- Sedentary behavior: Beyond just exercise, the total amount of time spent inactive has independent effects on metabolism. Extended sitting time reduces muscle activity, decreases glucose uptake, and promotes insulin resistance even in people who otherwise exercise regularly.
- Eating frequency and timing: Constant snacking and extended eating windows give your digestive system and pancreas little opportunity to rest. Research indicates that longer daily fasting periods may enhance insulin sensitivity and improve glucose regulation.
- Chronic stress: Persistent stress elevates cortisol levels, which directly increases blood glucose and promotes abdominal fat storage. Stress also frequently leads to disrupted sleep, emotional eating, and other behaviors that further compromise metabolic health.
- Environmental toxins: Emerging research suggests certain environmental contaminants, including some plastics, pesticides, and air pollutants, may act as “endocrine disruptors” that interfere with normal insulin signaling.
The good news about lifestyle factors is that, unlike genetics or age, they’re largely modifiable. Making targeted changes to these elements forms the foundation of effective prediabetes prevention and reversal strategies.
Genetic Predisposition to Prediabetes
While lifestyle plays a crucial role, genetic factors significantly influence prediabetes risk. Research, particularly from studies of identical twins, demonstrates that genetic factors account for 30-70% of diabetes risk, with similar patterns for prediabetes.
Several specific genetic influences have been identified:
- Family history: Having a first-degree relative (parent or sibling) with type 2 diabetes increases your risk by 2-6 times. This risk multiplies if multiple family members are affected.
- Ethnic background: Certain ethnic groups show higher prediabetes risk even when controlling for lifestyle factors. Research indicates that African Americans, Hispanic/Latino Americans, American Indians, Pacific Islanders, and Asian Americans develop insulin resistance at lower body weights and younger ages than Caucasians.
- Specific gene variants: Researchers have identified over 150 genetic variants associated with type 2 diabetes risk. One well-studied example is the TCF7L2 gene, which influences insulin production and glucose metabolism. Variations in this gene can increase diabetes risk by 30-50%.
- Epigenetic modifications: Environmental factors can cause changes in gene expression without altering the underlying DNA sequence. Research shows that factors like maternal nutrition during pregnancy can influence offspring’s diabetes risk through epigenetic mechanisms that may persist across generations.
Importantly, genetic predisposition doesn’t guarantee prediabetes development. Rather, genetics typically establishes susceptibility that environmental factors can either trigger or suppress. This interaction between genes and environment explains why some people with high genetic risk never develop prediabetes, while others with lower genetic risk do.
Health Risks of Untreated Prediabetes
Many people mistakenly view prediabetes as merely a “warning sign” without immediate health consequences. However, research clearly shows that prediabetes itself—even before progression to diabetes—carries significant health risks. Understanding these dangers provides powerful motivation for taking prediabetes seriously and implementing preventive strategies before complications develop.
Short-term Health Impacts of Prediabetes
Even in its early stages, prediabetes can affect your health and quality of life in several important ways:
- Metabolic inefficiency: The insulin resistance underlying prediabetes impairs your body’s ability to efficiently convert food into energy. This often manifests as unexplained fatigue, especially after carbohydrate-rich meals, when your cells cannot properly access the glucose in your bloodstream despite adequate caloric intake.
- Cognitive effects: Research published in Diabetes Care demonstrates that prediabetes is associated with subtle cognitive changes, including decreased processing speed and memory function. These effects occur because insulin plays important roles in brain metabolism and neural health beyond just glucose regulation.
- Immune system impairment: Even moderately elevated blood sugar can compromise immune function. Studies show that individuals with prediabetes experience slower wound healing and increased susceptibility to infections compared to those with normal glucose metabolism.
- Sleep disturbances: Prediabetes is linked to poorer sleep quality and increased risk of sleep disorders. This creates a concerning cycle, as sleep disruption further impairs glucose regulation, potentially accelerating prediabetes progression.
- Reduced exercise capacity: The metabolic inefficiency of prediabetes often reduces physical endurance and recovery, making exercise more challenging precisely when it’s most beneficial.
These short-term effects not only reduce quality of life but also create negative cycles that can accelerate prediabetes progression. For example, fatigue leads to less activity, which further worsens insulin resistance, creating a downward spiral of metabolic health.
Long-term Complications of Untreated Prediabetes
If prediabetes remains unaddressed, more serious health consequences can develop over time, even before progression to diabetes:
- Cardiovascular disease: Research published in the American Diabetes Association’s Standards of Care indicates that prediabetes increases cardiovascular disease risk by 13-30% compared to normal blood glucose levels. This elevated risk occurs because even modestly elevated blood sugar damages blood vessels and accelerates atherosclerosis (hardening and narrowing of arteries).
- Kidney damage: Studies show that 18% of people with prediabetes have evidence of chronic kidney disease—nearly twice the rate seen in those with normal blood sugar. This damage often begins silently, with no obvious symptoms until significant impairment has occurred.
- Neuropathy: Approximately 10-15% of people with prediabetes show early signs of peripheral nerve damage (neuropathy). This typically begins as subtle tingling or numbness in the extremities but can progress to more significant pain and sensory loss.
- Retinopathy: Early eye changes, including small hemorrhages and blood vessel damage in the retina, have been documented in people with prediabetes, potentially affecting vision over time.
- Increased cancer risk: Research has linked prediabetes to elevated risk for several cancer types, including pancreatic, colorectal, liver, and endometrial cancers. The mechanisms likely involve insulin’s growth-promoting effects and the chronic inflammation associated with impaired glucose metabolism.
What’s particularly concerning about these complications is that they often develop gradually and silently. By the time obvious symptoms appear, significant damage may have already occurred. Additionally, these complications don’t necessarily resolve completely even if blood sugar is later controlled—some damage may be permanent.
Connection Between Prediabetes and Other Health Conditions
Prediabetes rarely exists in isolation. It frequently occurs as part of a constellation of interconnected health conditions that collectively increase health risks:
- Metabolic Syndrome: Prediabetes is often one component of metabolic syndrome—a cluster of conditions that also includes abdominal obesity, high blood pressure, elevated triglycerides, and low HDL (“good”) cholesterol. Research shows that when prediabetes occurs alongside these other factors, cardiovascular risk increases dramatically—more than the sum of each individual risk factor.
- Fatty Liver Disease: Approximately 50% of people with prediabetes have non-alcoholic fatty liver disease (NAFLD), a condition where excess fat accumulates in liver cells. This creates a dangerous cycle, as fatty liver further impairs insulin sensitivity and glucose metabolism, potentially accelerating prediabetes progression.
- Obstructive Sleep Apnea: Studies show that 40-80% of people with type 2 diabetes have sleep apnea, with similar patterns emerging in prediabetes. Sleep apnea further impairs glucose metabolism and increases cardiovascular risk, creating another self-reinforcing cycle.
- Polycystic Ovary Syndrome (PCOS): This hormonal disorder affects up to 10% of women and frequently co-occurs with prediabetes. The insulin resistance underlying both conditions creates a bidirectional relationship where each condition can worsen the other.
- Depression and Anxiety: Research has identified significant bidirectional relationships between prediabetes and mood disorders. Insulin resistance affects neurotransmitter function, while stress hormones from anxiety and depression impair glucose regulation.
These interconnections explain why addressing prediabetes often requires a comprehensive approach that considers these related conditions. Treating prediabetes in isolation without addressing these connected factors typically yields less effective results.
Importance of Prediabetes Prevention and Early Intervention
The cascade of health risks associated with prediabetes underscores the critical importance of prevention and early intervention. Research provides compelling evidence for prioritizing these efforts:
- Reversibility Window: The defining characteristic separating prediabetes from diabetes is reversibility. While diabetes represents permanent pancreatic damage, prediabetes involves reversible metabolic dysfunction. Research from the Diabetes Prevention Program demonstrates that appropriate interventions can reduce progression to diabetes by up to 58%—a success rate higher than many medical treatments for established diseases.
- Cost-Effectiveness: Preventing prediabetes progression is dramatically more cost-effective than treating diabetes and its complications. Economic analyses estimate that preventing one case of diabetes saves approximately $124,600 in lifetime healthcare costs.
- Quality of Life Impact: Early intervention preserves quality of life by preventing debilitating complications that can affect mobility, vision, comfort, and independence. Research shows that people who successfully reverse prediabetes report significantly higher quality of life scores than those who progress to diabetes.
- Systemic Health Benefits: The lifestyle modifications that prevent prediabetes progression—improved nutrition, increased physical activity, stress management, and adequate sleep—provide broad health benefits beyond just glucose control, including reduced cancer risk, improved mental health, and enhanced longevity.
The most effective prevention strategies are those implemented earliest, ideally before significant metabolic dysfunction has occurred. This reinforces the importance of regular screening, particularly for those with risk factors, to identify prediabetes in its earliest, most reversible stages.
Understanding the serious health risks associated with prediabetes transforms it from an abstract “pre-condition” to a concrete health priority demanding attention. By recognizing these risks, you can make informed decisions about implementing preventive strategies to protect your health before complications develop.
Conclusion: Taking Control of Prediabetes
Prediabetes represents a critical crossroads in metabolic health—a condition where blood sugar levels are elevated but haven’t yet reached diabetic levels. As we’ve explored throughout this article, prediabetes is far more than just a “pre-condition” or minor concern. It’s a distinct health state with real physiological effects and potential complications if left unaddressed.
The key takeaways about prediabetes include:
- It’s common but often undetected: With approximately 374 million adults worldwide having prediabetes and 90% unaware of their condition, proactive testing is essential, especially for those with risk factors.
- It’s defined by specific blood sugar ranges: Fasting glucose between 100-125 mg/dL or HbA1c between 5.7-6.4% indicate prediabetes—numbers that require attention but don’t yet represent permanent damage.
- It presents through subtle symptoms: From darkened skin patches to post-meal fatigue, frequent hunger, and memory issues, prediabetes often signals its presence through easily overlooked signs.
- Its primary mechanism is insulin resistance: Cells becoming resistant to insulin’s signals forces the pancreas to compensate by producing more insulin—a pattern that can continue for years before eventual pancreatic fatigue.
- It carries significant health risks: Even before progression to diabetes, prediabetes increases cardiovascular disease risk by 13-30% and is associated with early kidney, nerve, and eye damage.
- It’s largely reversible: Unlike diabetes, which represents permanent pancreatic damage, prediabetes can be completely reversed through appropriate interventions.
The most important message about prediabetes is one of empowerment: this condition represents an opportunity to reclaim metabolic health before permanent damage occurs. With early detection, proper understanding, and appropriate lifestyle modifications, the progression from prediabetes to diabetes can be halted and even reversed in many cases.
Whether you’ve recently been diagnosed with prediabetes, are concerned about your risk factors, or simply want to optimize your metabolic health, taking action now provides the greatest chance for long-term wellness. Knowledge is the first step—and with the information in this guide, you’re better equipped to work with healthcare professionals to protect your metabolic health for years to come.
To access other content on the IFitCenter’s blog, you can use the following links:
Sources for Prediabetes Definition
- American Diabetes Association. Standards of Care in Diabetes—2025. Diabetes Care. 2024;47(Suppl 1):S1-S312. doi:10.2337/dc24-SINT.
- Li Y, Zhang Y, Wang Y, et al. Prevalence of Prediabetes by Fasting Plasma Glucose and HbA1c Screening Criteria Among Children and Adolescents in Shenzhen, China. Front Endocrinol (Lausanne). 2024;15:1301921. doi:10.3389/fendo.2024.1301921.
- University of California Health. Feasibility and Preliminary Effects of Fasting-Mimicking Diet in Asian Americans With Prediabetes. ClinicalTrials.gov identifier: NCTXXXXXXX. Updated February 24, 2025. Accessed February 24, 2025.



