Is your blood pressure truly normal, or are you relying on outdated information? Do you know which number in your blood pressure reading—systolic or diastolic—matters more at your age? Can normal blood pressure vary between men and women? And perhaps most importantly: how can understanding your blood pressure readings help prevent the “silent killer” that affects billions worldwide?
These questions aren’t merely academic—they’re at the heart of cardiovascular health. Blood pressure is one of the most critical vital signs, yet it remains widely misunderstood. Many people check their blood pressure regularly without truly comprehending what the numbers represent or how to interpret variations. This knowledge gap isn’t just confusing—it can be dangerous.
At IFitCenter, we’ve found that clarifying these fundamentals of normal blood pressure helps our clients make better health decisions. Understanding whether your blood pressure falls within the normal range for your demographic can provide early warning signs of cardiovascular issues or reassurance that your health is on track.
In this comprehensive guide, we’ll address these critical questions about normal blood pressure. We’ll explore how blood pressure is measured, what the numbers actually mean, how normal ranges vary across different groups, and which factors can affect your readings. By the end, you’ll have a clearer understanding of this vital health indicator and be better equipped to monitor your cardiovascular wellbeing.
What Is Blood Pressure and How Is It Measured?
Blood pressure is essentially the force that blood exerts against the walls of your arteries as it travels through your body. Think of it like water flowing through a garden hose—the pressure inside the hose changes depending on how forcefully the water is pumped and how narrow the hose is. Similarly, your blood pressure changes based on how strongly your heart pumps and the condition of your arteries.
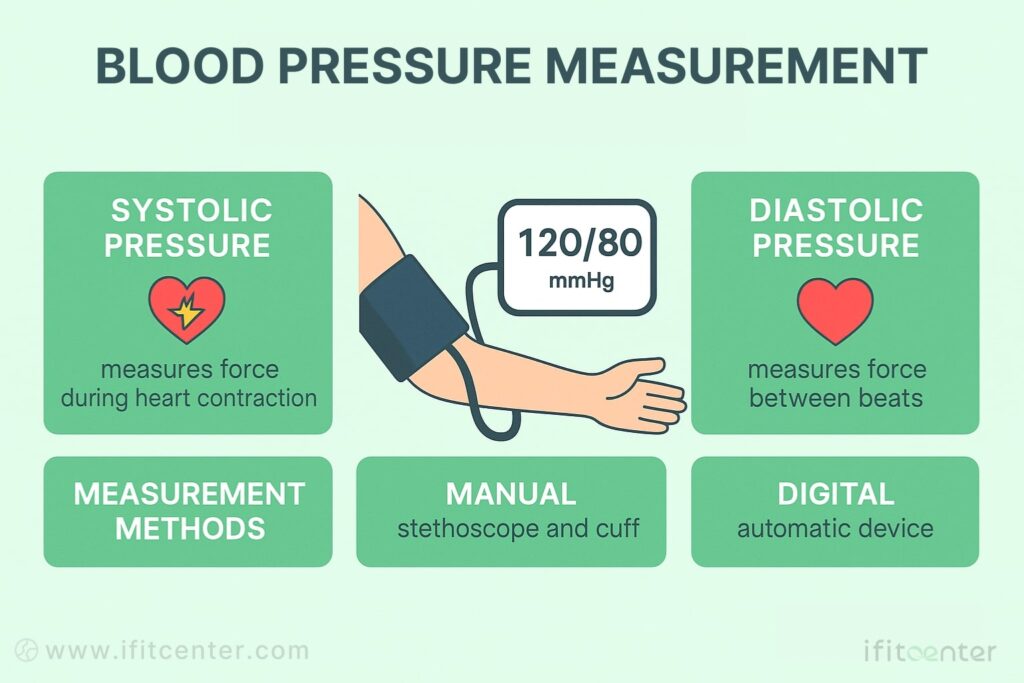
When your doctor says your blood pressure is “120 over 80,” they’re referring to two different measurements that capture the dynamic nature of blood flow:
- Systolic pressure (the top number): This measures the force your blood exerts against artery walls when your heart contracts or beats. It’s like the surge of pressure in that garden hose the moment you turn the faucet on full force.
- Diastolic pressure (the bottom number): This measures the pressure when your heart is resting between beats. Continuing our garden hose analogy, it’s like the residual pressure that remains in the hose even when water flow is at its minimum.
According to the American Heart Association, “Diastolic blood pressure measures the pressure your blood is pushing against your artery walls while the heart muscle rests between beats,” while systolic pressure measures this force during active heart contraction.
Both numbers are measured in millimeters of mercury, abbreviated as “mmHg.” This unit has historical roots—early blood pressure measurements used columns of mercury that would rise and fall with pressure changes. Though modern digital devices no longer use mercury, we’ve kept this standard unit for consistency.
How Blood Pressure Is Measured
There are two primary methods for measuring blood pressure:
- Manual/Auscultatory Method: This traditional approach uses a stethoscope and a sphygmomanometer (the inflatable cuff with a pressure gauge). A healthcare provider listens for specific sounds (called Korotkoff sounds) that indicate systolic and diastolic pressure points as the cuff slowly deflates.
- Digital/Oscillometric Method: Modern automated devices detect oscillations (small vibrations) in the arteries when the cuff inflates and deflates. These devices calculate your blood pressure using algorithmic interpretations of these oscillations, displaying the results digitally without requiring someone to listen with a stethoscope.
Home blood pressure monitors typically use the digital method, making them user-friendly even without medical training. However, the accuracy of these devices can vary, which is why periodic calibration against professional equipment is recommended.
As noted in a recent scientific statement from the American Heart Association, using a cuff that’s too small can result in artificially elevated readings, while using a cuff that’s too large can give readings that are artificially low. Other factors can similarly affect accuracy—talking during measurement or having your arm positioned below heart level can raise your blood pressure reading by 10-15 mmHg.
Understanding both what blood pressure is and how it’s measured gives you valuable context for interpreting your readings and recognizing what constitutes normal blood pressure—which we’ll explore in the next section.
What Is Considered Normal Blood Pressure Range?
Normal blood pressure is defined as a reading less than 120/80 mmHg. This means your systolic pressure (top number) should be below 120 and your diastolic pressure (bottom number) should be below 80. When your blood pressure falls within this range, it indicates that your heart is working efficiently and your blood vessels are functioning properly.
Blood Pressure Categories
| Category | Systolic (mmHg) | Diastolic (mmHg) |
|---|---|---|
| Normal | Less than 120 | Less than 80 |
| Elevated | 120-129 | Less than 80 |
| Hypertension Stage 1 | 130-139 | 80-89 |
| Hypertension Stage 2 | 140 or higher | 90 or higher |
| Hypertensive Crisis | Higher than 180 | Higher than 120 |
According to the American Heart Association and the American College of Cardiology guidelines updated in 2017, hypertension now begins at 130/80 mmHg rather than the previous threshold of 140/90 mmHg. This change reflects growing evidence that damage to blood vessels can occur even at lower pressure levels than previously thought.
On the IFitCenter blog, we have prepared a free information database about various diseases, including high blood pressure, for you, our dear readers. By reviewing these resources, you will gain valuable information for controlling and preventing these conditions. To access the first part of the information, you can use the links below:
- What Causes High Blood Pressure?
- Blood Pressure Chart
- How to Measure Blood Pressure
- Hypertension symptoms
- How to Lower Blood Pressure
- Which oil is best for heart and cholesterol
What These Numbers Mean for Your Health
Your blood pressure reading provides important insights into your cardiovascular health:
- Normal blood pressure (below 120/80): Your cardiovascular system is functioning well, with minimal strain on your heart and blood vessels.
- Elevated blood pressure (120-129/below 80): While not yet hypertension, this category signals potential health concerns and increased risk of developing high blood pressure if lifestyle changes aren’t made.
- Hypertension Stage 1 (130-139/80-89): At this stage, your doctor may recommend lifestyle changes and possibly medication, depending on your overall cardiovascular risk.
- Hypertension Stage 2 (140+/90+): This level often requires both lifestyle modifications and medication to reduce the risk of heart attack, stroke, and other complications.
- Hypertensive Crisis (above 180/120): This dangerous condition requires immediate medical attention, as it can lead to organ damage and life-threatening complications.
While 120/80 mmHg is the general threshold for normal blood pressure, it’s important to understand that individual health factors can influence what’s considered optimal for you. Your healthcare provider might recommend different target ranges based on your age, medical history, and other health conditions.
Global Standards and Guidelines
adopted the American Heart Association’s threshold of 130/80 mmHg for hypertension. The European Society of Cardiology and the International Society of Hypertension, for example, still maintain the traditional 140/90 mmHg threshold for diagnosing hypertension, though they have introduced categories like “high-normal” or “elevated” blood pressure for readings between 120-139/80-89 mmHg.
What’s most important to understand is that blood pressure guidelines are based on extensive research showing the relationship between blood pressure levels and cardiovascular risk. The current thresholds reflect the levels at which intervention has been shown to reduce complications from hypertension.
Normal Blood Pressure By Age and Gender
While 120/80 mmHg is the standard threshold for normal blood pressure in adults, this benchmark can vary based on age and gender. Understanding these differences is crucial for properly interpreting your blood pressure readings.
Normal Blood Pressure Ranges By Age
| Age Group | Normal Blood Pressure Range |
|---|---|
| Children (3-5 years) | 95-110/56-70 mmHg |
| Children (6-9 years) | 97-115/57-76 mmHg |
| Children (10-12 years) | 102-120/61-80 mmHg |
| Adolescents (13-15 years) | 110-131/64-83 mmHg |
| Adults (18-40 years) | Less than 120/80 mmHg |
| Adults (40-60 years) | Less than 140/90 mmHg* |
| Adults (60+ years) | Less than 150/90 mmHg* |
As the table shows, blood pressure tends to increase naturally with age. This doesn’t mean hypertension is inevitable or normal in older adults, but rather reflects physiological changes that occur throughout life.
Normal Blood Pressure Differences Between Men and Women
Research has consistently shown that blood pressure patterns differ between men and women:
- Men typically have higher blood pressure than women of the same age until around 65 years.
- Women often experience a more significant increase in blood pressure after menopause, sometimes surpassing men’s levels in older age groups.
- Young and middle-aged women generally have lower systolic pressure (by 5-10 mmHg) than men in the same age range.
Normal Blood Pressure For Elderly
For seniors (65+ years), blood pressure management requires special consideration. While the general threshold for high blood pressure remains 130/80 mmHg, some medical guidelines suggest slightly higher acceptable ranges for very elderly patients (75+ years) to prevent complications from blood pressure that’s too low.
However, it’s important to note that higher blood pressure in elderly individuals is not “normal” in the sense of being optimal for health. Rather, it represents a common age-related change that still increases cardiovascular risk but may be managed differently based on individual health factors.
To access the second section of blood pressure articles, I invite you to use the links below:
- dash diet for hypertension
- complications of hypertension
- Best foods for hypertension
- Foods to Avoid with hypertension
- is headache a sign of hypertension?
- Does being obese cause high blood pressure?
- Does fasting help with high blood pressure?
Why Blood Pressure Changes With Age and Differs By Gender
Several physiological factors explain these variations:
- Arterial stiffness: As we age, our arteries naturally become less elastic, creating increased resistance to blood flow and raising systolic pressure.
- Hormonal differences: Estrogen in women appears to have a protective effect on the cardiovascular system before menopause, contributing to generally lower blood pressure compared to age-matched men.
- Body composition: Men typically have greater muscle mass and different fat distribution patterns than women, which can influence blood pressure regulation.
- Vascular aging: The rate at which blood vessels age can differ between men and women, affecting how blood pressure changes over time.
Understanding these age and gender differences helps healthcare providers make more accurate assessments of cardiovascular risk and develop appropriate treatment strategies when needed.
Systolic vs. Diastolic Blood Pressure: Which Number Matters More?
When looking at your blood pressure reading of 120/80 mmHg, you might wonder which number deserves more attention. Both values provide important information about your cardiovascular health, but research suggests they may not carry equal weight in predicting health risks.
“The relative importance of systolic versus diastolic blood pressure changes throughout our lifetime. For most patients under 50, both numbers deserve equal attention. However, after 50, systolic pressure often becomes the more critical indicator as our arteries naturally stiffen with age. This doesn’t mean we ignore diastolic pressure—a healthy cardiovascular system requires both numbers to be within normal ranges.”
Dr. Babak Jamalian, Family Physician
What Each Number Represents Physiologically
To understand their relative importance, let’s revisit what each measurement indicates:
- Systolic pressure (top number): Represents the maximum force exerted on artery walls during heart contraction. This shows how hard your heart is working and the pressure your arteries must withstand during active pumping.
- Diastolic pressure (bottom number): Indicates the minimum pressure in your arteries between heartbeats when your heart is relaxing and refilling. This reflects the resistance in your blood vessels and how well your heart can rest.
Which Number Is More Predictive of Health Issues?
According to current research, the relative importance of these numbers depends largely on your age:
- For adults over 50: Systolic blood pressure is generally considered more important for predicting cardiovascular risk. This is because systolic pressure tends to rise naturally with age as arteries become stiffer and less elastic.
- For adults under 50: Diastolic pressure may be equally or more important, particularly in cases of isolated diastolic hypertension (elevated diastolic with normal systolic).
Medical research indicates that elevated systolic pressure is more strongly associated with the risk of heart disease, stroke, kidney damage, and other complications in most adults, especially those over 50 years of age.
When to Be Concerned About Each Measurement
High Systolic, Normal Diastolic (Isolated Systolic Hypertension)
This pattern is common in older adults and occurs when systolic reaches 130 mmHg or higher while diastolic remains below 80 mmHg. It’s primarily caused by arterial stiffening and is associated with increased risk of:
- Heart attack
- Stroke
- Heart failure
- Aortic aneurysms
Normal Systolic, High Diastolic (Isolated Diastolic Hypertension)
This pattern is more common in younger adults (under 50) and occurs when diastolic reaches 80 mmHg or higher while systolic remains below 130 mmHg. It can indicate:
- Increased peripheral resistance in blood vessels
- Potential early-stage cardiovascular disease
- Risk to smaller blood vessels in organs like the kidneys, brain, and eyes
Evidence-Based Findings
Research has consistently shown that systolic blood pressure rises steadily with age in most adults, while diastolic pressure tends to rise until about age 50 and then gradually decreases. This pattern explains why systolic pressure becomes a stronger predictor of cardiovascular risk in older adults.
Importantly, large-scale studies have found that for every 20 mmHg increase in systolic pressure or 10 mmHg increase in diastolic pressure, there is a doubling of mortality from stroke, heart disease, and other vascular complications.
While both numbers are significant, current medical guidelines place greater emphasis on controlling systolic pressure, especially in older adults, as this approach has been shown to significantly reduce cardiovascular complications.
Factors That Affect Blood Pressure Readings: Understanding Normal Variations

Blood pressure is not static—it fluctuates throughout the day and can be influenced by numerous factors. Understanding these variations is crucial for accurate monitoring and avoiding misdiagnosis of hypertension based on temporarily elevated readings.
In the second part of our blog content introduction, we have prepared valuable articles in the field of healthy nutrition and weight loss for you. To access them, simply use the links below:
- make healthy food taste good
- manage food cravings
- preserve muscle during medical weight loss
- why diet fails
Achieve Healthy Blood Pressure at IFitCenter
Maintaining normal blood pressure often requires more than regular checks—it involves targeted lifestyle adjustments. At IFitCenter, under the expert guidance of Dr. Babak Jamalian, we offer comprehensive weight-loss solutions designed to naturally improve your cardiovascular health:
✔ Personalized nutritional plans
✔ Effective weight management strategies
✔ Continuous health monitoring
Start your journey to optimal blood pressure and overall well-being today.
Common Blood Pressure Measurement Mistakes
Even small errors in measurement technique can significantly alter blood pressure readings:
- Incorrect cuff size: Using a cuff that’s too small can artificially raise readings by 2-10 mmHg, while an oversized cuff may give falsely low readings.
- Improper arm position: Your arm should be at heart level—too high gives lower readings, too low produces higher readings.
- Insufficient rest time: Not sitting quietly for 3-5 minutes before measurement can elevate readings.
- Talking during measurement: Conversation during the reading can raise blood pressure by 10-15 mmHg.
- Crossed legs: This position can increase readings by 5-8 mmHg.
Normal Daily Fluctuations
Your blood pressure naturally varies throughout the day following circadian rhythms:
- Morning surge: Blood pressure typically rises upon waking and peaks mid-morning.
- Afternoon dip: A slight decrease often occurs in the early to mid-afternoon.
- Evening variations: Readings may rise again in the early evening.
- Nighttime drop: During sleep, blood pressure typically falls by 10-20% (known as “dipping”).
Physical and Environmental Factors
Several temporary conditions can alter your blood pressure readings:
- Recent meals: Eating can temporarily lower or raise blood pressure.
- Full bladder: A distended bladder can raise readings by 10-15 mmHg.
- Caffeine consumption: Coffee and other caffeinated beverages can elevate readings for up to 25 hours.
- Tobacco use: Smoking causes an immediate spike that can last 15-30 minutes.
- Alcohol: Recent alcohol consumption can either raise or lower readings.
- Room temperature: Cold environments typically increase blood pressure.
- Exercise: Physical activity raises blood pressure during exertion, with readings remaining elevated for up to 2 hours afterward.
Stress and Blood Pressure
Psychological factors play a significant role in blood pressure readings:
- White coat hypertension: Blood pressure elevation specifically in medical settings, caused by anxiety about the examination.
- Acute stress: Temporary emotional stress activates the sympathetic nervous system, raising both heart rate and blood pressure.
Scientific Explanation for Variations
These fluctuations occur due to your body’s regulatory mechanisms:
- Autonomic nervous system: Controls involuntary functions and adjusts blood pressure through blood vessel constriction/dilation and heart rate changes.
- Baroreceptors: Pressure sensors in blood vessels that help maintain blood pressure within normal ranges by sending signals to the brain.
- Hormonal regulation: Hormones like adrenaline (during stress) and angiotensin (for fluid balance) influence blood pressure.
- Vascular elasticity: Blood vessels expand and contract to help regulate pressure throughout the circulatory system.
Understanding these factors helps explain why a single elevated reading doesn’t necessarily indicate hypertension. Most medical guidelines recommend taking multiple readings on different days before making a diagnosis, or using 24-hour ambulatory monitoring to capture the complete picture of your blood pressure patterns.
Common Questions About Normal Blood Pressure Readings
Many misconceptions exist about blood pressure, leading to unnecessary anxiety or inappropriate self-management. Let’s address some of the most frequently asked questions about normal blood pressure with evidence-based answers.
Is 120/80 the Only Normal Blood Pressure?
While 120/80 mmHg is often cited as the ideal blood pressure, normal readings can actually range below this threshold. A more accurate description of normal blood pressure is less than 120 mmHg systolic and less than 80 mmHg diastolic. Slightly lower readings (for example, 110/70) are perfectly healthy and often desirable.
Does a Single High Reading Mean I Have Hypertension?
No. Diagnosis of hypertension typically requires multiple elevated readings on different days. Blood pressure naturally fluctuates throughout the day and can be temporarily elevated due to stress, caffeine, physical activity, or improper measurement technique. This is why current guidelines recommend confirming high readings with repeated measurements before making a diagnosis.
Which Is More Dangerous: High Systolic or High Diastolic?
Both can indicate cardiovascular risk, but their relative importance varies with age. For adults over 50, elevated systolic pressure is generally considered a stronger predictor of heart disease and stroke. In younger adults, elevated diastolic pressure may be equally concerning. The best approach is to monitor both numbers and work with healthcare providers to keep both within normal ranges.
Can Blood Pressure Be Too Low?
Yes, though “too low” varies between individuals. Generally, blood pressure is considered too low when it causes symptoms like dizziness, fainting, nausea, or fatigue. For most adults, systolic pressure below 90 mmHg or diastolic below 60 mmHg might be concerning if accompanied by symptoms, but may be normal for others, particularly athletes or young adults.
Should Blood Pressure in Both Arms Be the Same?
Small differences (less than 10 mmHg) between arms are common and considered normal. However, consistent differences greater than 10 mmHg may indicate vascular problems like arterial narrowing and should be evaluated by a healthcare provider. Current guidelines recommend checking blood pressure in both arms during initial assessment.
Does Normal Blood Pressure Change With Age?
While the definition of hypertension doesn’t change with age (still 130/80 mmHg or higher), blood pressure tends to increase naturally as we age due to decreased arterial elasticity. However, this doesn’t mean hypertension should be considered “normal” for elderly individuals—elevated blood pressure remains a health risk at any age, though treatment approaches may differ.
Understanding your normal blood pressure range requires consideration of multiple factors, including age, gender, overall health, and proper measurement technique. For personalized guidance on interpreting your blood pressure readings, consider consulting with a cardiovascular specialist who can provide tailored recommendations based on your unique health profile.
Conclusion: Understanding Your Normal Blood Pressure Range
Understanding what constitutes normal blood pressure is essential for maintaining long-term cardiovascular health. As we’ve explored, normal blood pressure is generally defined as readings below 120/80 mmHg, though these values can vary based on age, gender, and individual health factors.
Key takeaways from our discussion include:
- Blood pressure consists of two measurements: systolic (pressure during heart contraction) and diastolic (pressure between beats)
- For most adults, systolic pressure becomes increasingly important with age, especially after 50
- Normal blood pressure ranges can vary by age and gender, though the threshold for hypertension remains consistent at 130/80 mmHg
- Multiple factors can affect blood pressure readings, from measurement technique to time of day
- A single elevated reading doesn’t necessarily indicate hypertension—regular monitoring provides a more accurate picture
Regular blood pressure monitoring is one of the simplest yet most powerful tools for cardiovascular health assessment. By understanding your personal normal range and tracking changes over time, you can detect potential issues early and take appropriate action.
Remember that maintaining normal blood pressure involves more than just knowing your numbers—it requires a holistic approach to health that includes proper diet, regular physical activity, stress management, and appropriate medical care when needed.
Take control of your cardiovascular health by understanding your blood pressure numbers and consulting with experts when needed. At IFitCenter, we believe that knowledge is the first step toward optimal health, and we’re committed to helping you understand the vital signs that matter most to your wellbeing.
To access other content on the IFitCenter’s blog, you can use the following links:
References
- Satoh M, Tatsumi Y, Nakayama S, et al. Self-measurement of blood pressure at home using a cuff device for change in blood pressure levels: systematic review and meta-analysis. Hypertens Res. 2025 Feb;48:574-591. DOI: 10.1038/s41440-024-01981-4
- Oommen John, Norm RC Campbell, Tammy M Brady, Margret Farrell, Cherian Varghese, Adriana Velazquez Berumen, Laura A Velez Ruiz Gaitan, Nicola Toffelmeire, Mohammad Ameel, Mulugeta Mideksa, Marc G Jaffe, Aletta E Schutte, Taskeen Khan, Laura Patricia Lopez Meneses. The 2020 “WHO Technical Specifications for Automated Non-Invasive Blood Pressure Measuring Devices With Cuff”. Hypertension. 2021 Feb 1;77(3):806-812. DOI: 10.1161/HYPERTENSIONAHA.120.166251
- Bo Y, Kwok KO, Chung VCH, Yu CP, Tsoi KKF, Wong SYS, Lee EKP. Short-term reproducibility of ambulatory blood pressure measurements: a systematic review and meta-analysis of 35 observational studies. Journal of Hypertension. 2020 Nov;38(11):2095-2109. DOI: 10.1097/HJH.00000000000025222
- Lin JY, Kuo KL, Kuo YH, Wu KP, Chu KC, Jiang YC, Chuang YF, Cheng HM. Association between real-world home blood pressure measurement patterns and blood pressure variability among older individuals with hypertension: A community-based blood pressure variability study. J Clin Hypertens (Greenwich). 2020 Dec 18;23(3):628-637. DOI: 10.1111/jch.141343
- Carey RM, Whelton PK. The evidence for a general blood pressure goal of < 130/80 mmHg is strong controversies in hypertension: pro. Hypertension. 2020 Sep 21;76(5):1384-1390. DOI: 10.1161/HYPERTENSIONAHA.120.14647
- Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, Myers MG, et al. on behalf of the American Heart Association Council on Hypertension; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; and Council on Quality of Care and Outcomes Research. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension. 2019 Mar 4;73(5). DOI: 10.1161/HYP.0000000000000087
- Murthy S, Rajwar E, Johnson R, Shrivastava K, Kamath P, Rahman R, Devaria A, Ismavel VA, Vetter BN, Jacob AG, John O. Validation of blood pressure devices as per 2020 World Health Organization technical specifications: a scoping review of global literature. Hypertension. 2023 May;80(5):1110-1116. DOI: 10.1161/HYPERTENSIONAHA.122.20425



