Think insulin resistance only affects people with diabetes? Think again. This common belief could be preventing millions from recognizing early warning signs of a condition that affects their daily health. While many believe insulin resistance is simply a precursor to diabetes, groundbreaking research from 2023 reveals it’s actually a complex metabolic condition that can impact everything from your energy levels to your ability to maintain a healthy weight – even if your blood sugar levels appear normal.
Another widespread misconception? That insulin resistance only develops in people who are overweight. The reality is far more complex. Studies show that up to 20% of individuals with normal body weight show signs of insulin resistance, a phenomenon scientists now call “metabolically unhealthy normal weight.” At IFitCenter, we’ve seen firsthand how this silent condition can affect people of all body types and lifestyles.
Understanding insulin resistance means looking beyond these common myths to discover what’s really happening in your body. In this comprehensive guide, we’ll explore the science behind this condition, decode its early warning signs, and reveal why it matters for your overall health – regardless of your current health status.
Understanding Insulin’s Role in Body
Your body has a remarkable system for managing energy, and at the center of this system is a hormone called insulin. Before we can understand insulin resistance, we need to grasp how insulin normally works in your body.
The Basic Function of Insulin
Imagine your bloodstream as a busy delivery system, constantly transporting glucose (sugar) to all your body’s cells. Insulin acts as the delivery manager, making sure this precious energy source reaches its destination. Without insulin, glucose would remain stuck in your bloodstream, unable to reach the cells that need it.
How Does This Process Work?
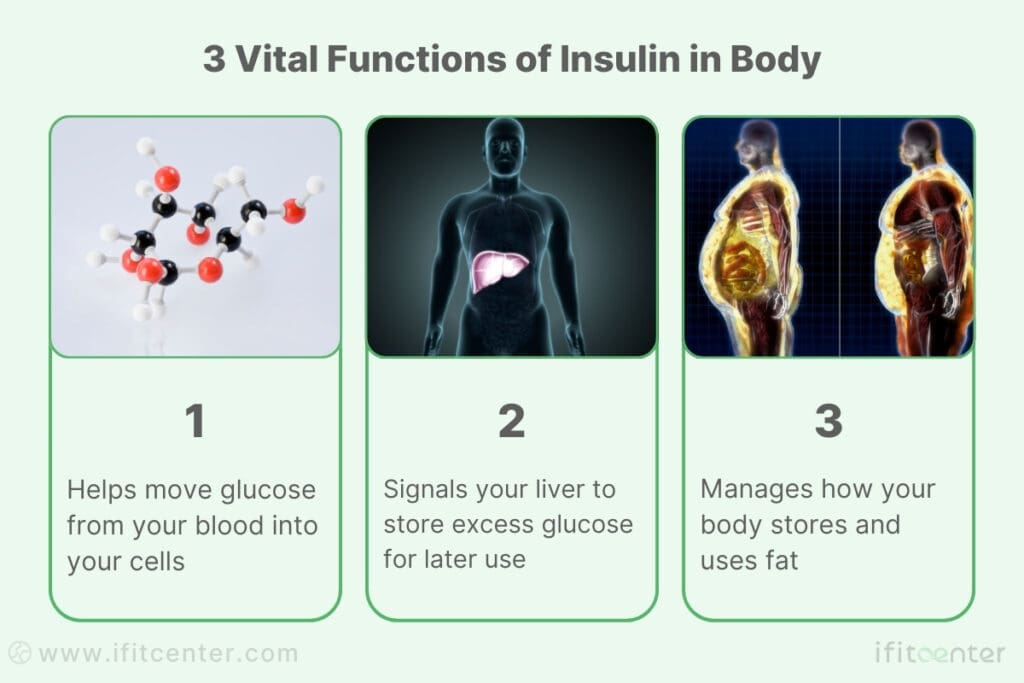
When you eat a meal, especially one containing carbohydrates, your digestive system breaks down the food into glucose. As this glucose enters your bloodstream, your pancreas releases insulin, which performs three vital functions:
- Helps move glucose from your blood into your cells
- Signals your liver to store excess glucose for later use
- Manages how your body stores and uses fat
Energy Storage and Management
Your body operates like a sophisticated energy bank:
- Short-term storage: Glucose is stored in your liver and muscles as glycogen (like keeping cash in your wallet)
- Long-term storage: Extra energy is stored as fat (like money in a savings account)
- Energy release: When needed, your body can access these stores between meals
Cellular Response
Every cell in your body has special receptors that respond to insulin. When insulin arrives at a cell, it triggers these receptors to create openings for glucose to enter – much like a key unlocking a door. This process is essential for maintaining healthy blood sugar levels and providing your cells with the energy they need.
On the IFitCenter blog, we have published a free content bank about insulin resistance that can have a significant impact for you in controlling and preventing this metabolic disease. For access, simply use the links below:
- how to reverse insulin resistance
- symptoms of insulin resistance
- testing for insulin resistance
- worst foods for insulin resistance
- Can Fasting Reverse Insulin Resistance?
Insulin Resistance Definition
Think of insulin resistance as a communication breakdown in your body’s energy management system. While your pancreas is sending clear signals through insulin, your cells have essentially turned down the volume on these messages.
The Two-Sided Nature of Insulin Resistance
Recent research reveals that insulin resistance involves two critical changes in your body:
- Your cells become less responsive to insulin’s signals
- Your body produces more insulin to compensate for this reduced response
How Does Insulin Resistance Develop?
When your cells repeatedly receive high amounts of insulin, they begin to reduce their sensitivity to it – similar to how you might become less sensitive to a loud noise after prolonged exposure. As cells become more resistant, your pancreas responds by producing even more insulin, creating a cycle that can worsen over time.
The Metabolic Flexibility Connection
One of the most significant impacts of insulin resistance is how it affects your body’s metabolic flexibility – your ability to switch between using different fuel sources. When your cells respond properly to insulin, your body can easily transition between burning sugar and fat for energy. However, insulin resistance can lock your metabolism into primarily burning sugar, making it difficult to access stored fat for energy.
Breaking Common Misconceptions About Insulin Resistance
Many people believe insulin resistance only affects those with diabetes or obesity. However, research shows that:
- Insulin resistance can affect people of any weight
- It often develops years before blood sugar levels rise
- Regular exercise alone may not prevent it
- Even young, active individuals can develop insulin resistance
“Many patients are surprised when I tell them that their normal blood sugar readings don’t rule out insulin resistance. In fact, insulin levels can be elevated for up to 13 years before blood sugar shows any significant change. This is why we often see seemingly healthy individuals with normal glucose levels already developing early signs of metabolic dysfunction.”
Dr. Babak Jamalian, Family Physician.
Cellular Impact
At the cellular level, insulin resistance disrupts your cells’ ability to:
- Take in glucose efficiently
- Store energy properly
- Maintain normal metabolic function
- Respond to other important hormonal signals
How Does Insulin Resistance Develop?
Understanding how insulin resistance develops is like watching a slow-motion film of metabolic changes. This condition doesn’t appear overnight – it’s a gradual process that can take years to become noticeable.
The Progressive Journey to Insulin Resistance
Your body’s relationship with insulin can change gradually over time, often without any obvious signs. Think of it like slowly turning up the volume on your TV – you might not notice the small increases, but eventually, the volume becomes much louder than necessary.
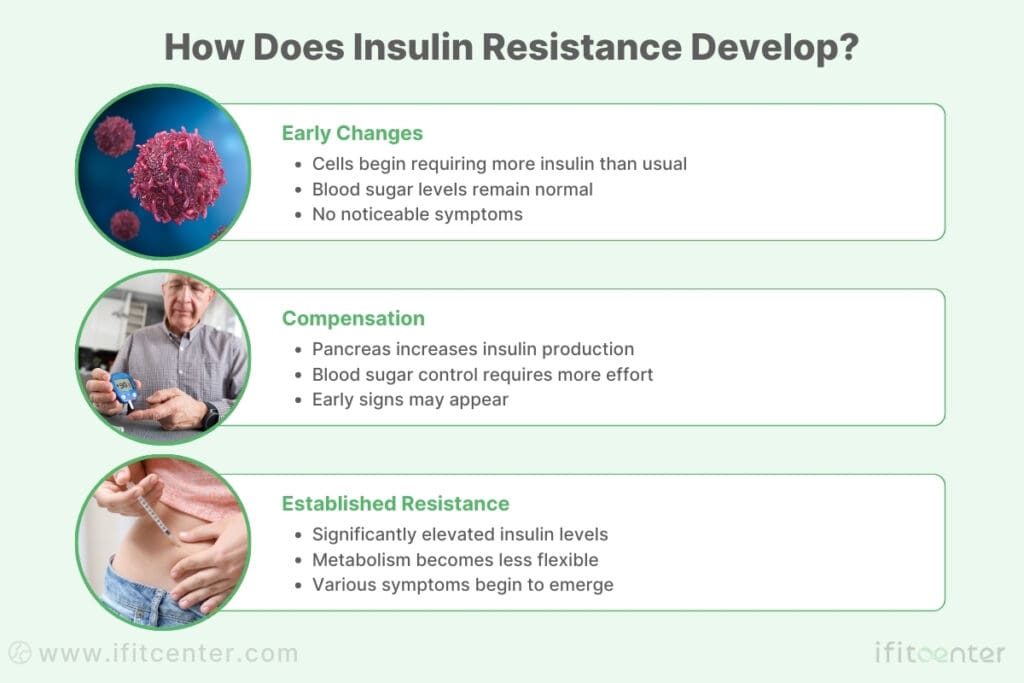
- Stage 1: Early Changes
- Cells begin requiring more insulin than usual
- Blood sugar levels remain normal
- No noticeable symptoms
- Stage 2: Compensation
- Pancreas increases insulin production
- Blood sugar control requires more effort
- Early signs may appear
- Stage 3: Established Resistance
- Significantly elevated insulin levels
- Metabolism becomes less flexible
- Various symptoms begin to emerge
Environmental Triggers
Modern life creates the perfect storm for insulin resistance development:
- Dietary Factors
- Frequent high-carb meals
- Processed food consumption
- Sugar-sweetened beverages
- Irregular eating patterns
- Lifestyle Elements
- Chronic stress
- Poor sleep quality
- Sedentary behavior
- Environmental toxins
Genetic Factors in Insulin Resistance
While we can’t change our genes, understanding their role helps explain why:
- Some people develop insulin resistance more easily than others
- Family history influences risk levels
- Different populations show varying susceptibility
- Response to lifestyle changes varies between individuals
Modern Lifestyle Impact
Today’s world presents unique challenges to metabolic health:
- Extended work hours disrupting natural rhythms
- Increased exposure to artificial light
- 24/7 food availability
- Reduced physical activity requirements
- Higher stress levels
Warning Signs and Symptoms of Insulin Resistance: What to Watch For
The challenge with insulin resistance is that early signs can be subtle and easily overlooked. Understanding these signs can help you identify potential issues before they progress to more serious conditions.
Early Warning Signs You Shouldn’t Ignore
Many people experience these initial indicators without realizing their significance:
- Increased hunger shortly after meals
- Afternoon energy crashes
- Difficulty concentrating
- Unexplained fatigue
- Sugar cravings, especially after meals
How Symptoms Progress Over Time
As insulin resistance develops, symptoms often appear in a predictable pattern:
- Physical Changes
- Gradual weight gain, especially around the midsection
- Difficulty losing weight despite diet changes
- Skin changes, particularly darkening in neck folds
- Unexpected fat accumulation in specific areas
- Energy and Mood Changes
- Consistent fatigue after meals
- Morning grogginess
- Irregular energy patterns throughout the day
- Mood fluctuations tied to eating
Observable Physical Signs
Physical manifestations often include:
- Skin Changes
- Skin tags appearing in neck area
- Dark patches (acanthosis nigricans)
- Changes in skin texture
- Body Composition Changes
- Increasing waist circumference
- Changes in fat distribution
- Muscle mass variations
“One of the most overlooked signs of insulin resistance is actually a skin condition called acanthosis nigricans. When patients come to me concerned about darkened skin patches around their neck or underarms, they’re often relieved to learn this isn’t just a cosmetic issue – it’s actually their body giving them an early warning signal about their metabolic health.”
Dr. Babak Jamalian, Family Physician.
Key Metabolic Markers
Several measurable indicators can signal insulin resistance:
- Blood Markers
- Fasting insulin levels
- Triglyceride to HDL ratio
- Blood pressure changes
- Fasting glucose levels
Connected Health Conditions
Insulin resistance rarely occurs in isolation. Watch for:
- Sleep disturbances
- Irregular menstrual cycles in women
- High blood pressure
- Persistent brain fog
- Unexplained inflammation
How Insulin Resistance Affects Your Health and Well-being
When insulin resistance develops, its effects ripple throughout your entire body. Understanding these impacts can help you recognize why addressing insulin resistance early is so crucial for your long-term health.
Day-to-Day Impact on Your Body
Your body’s struggle with insulin resistance begins to show itself in subtle ways that affect your daily life. Imagine trying to power your home with a weakened electrical system – some rooms might get enough power while others don’t. Similarly, when your cells resist insulin, they struggle to get the energy they need to function properly.
This energy disruption often shows up first in how you feel day-to-day. You might notice that after meals, instead of feeling energized, you experience unexplained fatigue. This happens because your cells aren’t efficiently processing the glucose from your food, leaving you feeling tired even though you’ve eaten plenty. Many people also experience sudden hunger or cravings, particularly for carbohydrates, as their cells signal that they need more energy despite having adequate fuel available in the bloodstream.
The Silent Progression
As insulin resistance continues, your body tries to compensate by producing more insulin. This increased production can lead to a cascade of effects that you might not immediately connect to insulin resistance:
Your blood pressure might begin to creep up, as insulin affects how your blood vessels function and how your body retains sodium. You might notice changes in your skin, particularly darkened patches around your neck or in body folds – a condition called acanthosis nigricans that directly results from high insulin levels.
Weight management becomes increasingly challenging. Even with careful eating habits, you might find that weight accumulates more easily, particularly around your midsection. This isn’t just about appearance – this pattern of weight gain is a sign that your metabolism is being significantly affected.
To access the second part of the insulin resistance content, I invite you to use the links below:
- insulin resistance in children
- supplements to reverse insulin resistance
- weight gain insulin resistance
- diabetes vs insulin resistance
- How Long Does It Take to Reverse Insulin Resistance?
Long-term Health Implications
Recent research has revealed just how extensively insulin resistance can affect your long-term health. Think of insulin resistance as a pebble creating ripples in a pond – its effects spread far beyond just blood sugar control:
Your cardiovascular system faces increased stress. High insulin levels can damage blood vessel walls and promote inflammation, potentially leading to heart disease over time. Your liver may begin accumulating excess fat, even if you don’t drink alcohol, leading to what doctors now call Metabolic Associated Fatty Liver Disease (MAFLD).
Perhaps most surprisingly, insulin resistance can affect your brain health. Scientists have discovered that insulin plays a crucial role in brain function, and when cells become resistant to its effects, it may contribute to cognitive decline and memory problems as you age.
Impact on Daily Quality of Life
Living with insulin resistance can significantly affect how you experience each day. Many people report:
- Unpredictable energy levels that make it hard to plan activities
- Difficulty concentrating at work or during important tasks
- Disrupted sleep patterns that leave them feeling unrested
- Mood changes that affect their relationships and daily interactions
These effects aren’t just inconveniences – they can impact your ability to enjoy life and perform at your best.
Key Takeaways: How Insulin Resistance Affects Your Health
Understanding how insulin resistance affects your health is crucial for recognizing and addressing this condition early. Let’s summarize the main impacts:
- Daily Energy and Function
- Unexpected fatigue after meals
- Difficulty maintaining steady energy levels
- Problems with focus and concentration
- Irregular hunger patterns
- Physical Health Changes
- Gradual weight gain, especially around midsection
- Changes in blood pressure
- Skin changes like darkened patches
- Disrupted sleep patterns
- Long-term Health Risks
- Increased risk of cardiovascular issues
- Potential cognitive health effects
- Liver health concerns
- Higher risk of developing type 2 diabetes
Remember: These effects don’t happen overnight, and recognizing them early gives you the best opportunity to take action. Many of these impacts can be prevented or reversed with appropriate lifestyle changes and medical support.
Take Control of Your Metabolic Health Before It’s Too Late
Many people live with undiagnosed insulin resistance for years, unaware of its progressive impact on metabolism, energy levels, and long-term health. Left unaddressed, this condition can lead to weight gain, chronic fatigue, and increased risk of type 2 diabetes. However, research shows that targeted weight management can significantly improve insulin function and prevent further metabolic complications.
At IFitCenter, our medical team specializes in metabolism-focused weight loss programs, ensuring that every step is designed to help your body regain insulin efficiency naturally. If you’ve noticed symptoms such as constant fatigue, unexplained weight gain, or sugar cravings, don’t wait—get professional support today.
How is Insulin Resistance Diagnosed? Understanding Your Test Results
Diagnosing insulin resistance requires a comprehensive approach, as no single test can tell the complete story. Modern medical science has developed several effective ways to identify this condition, often before it progresses to more serious health issues.
Key Blood Tests for Insulin Resistance
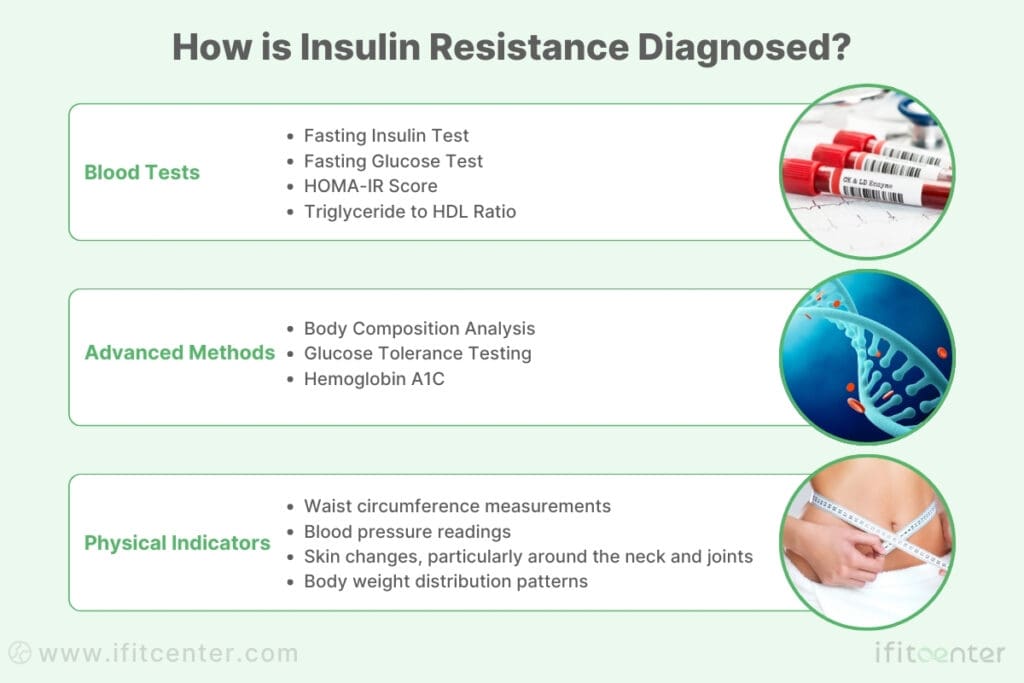
Blood testing provides crucial insights into how your body handles glucose and insulin. The most important markers include:
- Fasting Insulin Test: Measures insulin levels when you haven’t eaten, providing vital clues about your body’s insulin sensitivity
- Fasting Glucose Test: Shows how well your body maintains blood sugar levels without food
- HOMA-IR Score: Combines fasting insulin and glucose measurements to assess insulin resistance
- Triglyceride to HDL Ratio: An important indicator of metabolic health
Advanced Diagnostic Methods
Modern medicine offers sophisticated tools for more detailed analysis:
- Body Composition Analysis: Measures fat distribution patterns that may indicate insulin resistance
- Glucose Tolerance Testing: Evaluates how effectively your body processes sugar over time
- Hemoglobin A1C: Provides insight into your average blood sugar levels over the past three months
Physical Indicators and Examinations
Healthcare providers also look for physical signs during diagnosis:
- Waist circumference measurements
- Blood pressure readings
- Skin changes, particularly around the neck and joints
- Body weight distribution patterns
Understanding Your Test Results
Interpreting medical test results can be complex. Here’s what various markers typically indicate:
| Marker | Optimal Range | What It Indicates |
|---|---|---|
| Fasting Insulin | Less than 10 µIU/mL | How hard your body works to maintain blood sugar |
| Triglyceride/HDL Ratio | Less than 2 | Overall metabolic health |
| Fasting Glucose | 72-99 mg/dL | Blood sugar control |
The Importance of Early Detection
Research shows that identifying insulin resistance early provides the best opportunity for successful intervention. Regular monitoring of these markers can help track changes over time and guide treatment decisions.
Key Points About Diagnosis
- Multiple tests provide a more complete picture than any single test
- Regular monitoring helps track changes over time
- Physical examinations complement laboratory testing
- Early detection increases treatment success rates
Can Insulin Resistance Be Reversed? Current Research and Treatment Options
One of the most encouraging discoveries in recent metabolic health research is that insulin resistance can be improved and, in many cases, reversed. Understanding your options and taking action early provides the best opportunity for positive outcomes.
What Science Tells Us About Reversing Insulin Resistance
Recent research has revealed that our bodies have remarkable capacity for metabolic recovery. Studies show that positive changes can begin within days of starting appropriate interventions, though lasting improvement typically requires consistent effort over time.
Key Factors in Metabolic Recovery
Current scientific evidence points to several crucial elements that influence success in addressing insulin resistance:
- Timing of Meals: Research shows that when you eat can be as important as what you eat
- Sleep Quality: Proper sleep directly impacts insulin sensitivity
- Stress Management: Chronic stress can significantly affect metabolic health
- Movement Patterns: Regular physical activity improves cellular response to insulin
The Role of Early Intervention
Clinical studies consistently show that early action provides the best outcomes. The sooner insulin resistance is addressed, the more likely positive changes can occur:
- Cellular insulin sensitivity can improve within weeks
- Metabolic flexibility often starts returning within months
- Long-term health markers show positive changes with consistent effort
Emerging Treatment Approaches
Current research is exploring several promising directions in treating insulin resistance:
- Chronobiology: Understanding how timing affects metabolic processes
- Personalized Nutrition: Tailoring approaches to individual metabolic responses
- Gut Health: Exploring the connection between microbiome and insulin sensitivity
- Environmental Factors: Addressing hidden influences on metabolic health
Understanding Your Journey to Metabolic Health
Improving insulin sensitivity is a gradual process that typically involves several stages:
- Initial metabolic reset period
- Gradual improvement in insulin sensitivity
- Restoration of metabolic flexibility
- Long-term maintenance and optimization
Future Directions in Treatment
Ongoing research continues to uncover new insights about insulin resistance and potential treatment approaches:
- Development of targeted lifestyle interventions
- Better understanding of individual metabolic variations
- Improved methods for early detection and monitoring
- Integration of technology in treatment monitoring
Key Takeaways About Treatment
Understanding current treatment approaches helps set realistic expectations and develop effective strategies:
- Improvement is possible with appropriate interventions
- Early action provides the best outcomes
- Multiple factors influence success
- Consistent effort yields lasting results
Preventing Insulin Resistance: Evidence-Based Strategies That Work
While genetic factors can influence insulin resistance, research shows that lifestyle choices play a crucial role in prevention. Understanding and implementing proven strategies can significantly reduce your risk of developing this metabolic condition.
Key Prevention Principles
Scientific research has identified several core strategies that effectively help prevent insulin resistance. These approaches work together to support your body’s natural metabolic balance:
- Meal Timing: Creating natural periods of metabolic rest between meals
- Food Quality: Choosing foods that support metabolic health
- Movement Patterns: Incorporating regular physical activity
- Sleep Quality: Ensuring adequate restorative sleep
Daily Habits That Matter
Research shows that small, consistent actions can have powerful effects on preventing insulin resistance:
- Morning Routine
- Exposure to natural light
- Regular physical activity
- Protein-rich breakfast
- Throughout the Day
- Regular movement breaks
- Adequate hydration
- Stress management practices
- Evening Practices
- Light evening meals
- Digital device limitations
- Consistent sleep schedule
Monitoring Your Metabolic Health
Regular monitoring helps catch early signs of metabolic changes. Key areas to track include:
- Energy patterns throughout the day
- Changes in hunger and satiety signals
- Sleep quality and patterns
- Physical measurements like waist circumference
- Regular health marker checkups
Environmental Considerations
Modern research has identified several environmental factors that influence metabolic health:
- Light Exposure
- Natural daylight during morning hours
- Reduced blue light exposure in evenings
- Temperature Regulation
- Moderate temperature exposure
- Stress Management
- Creating calming environments
- Regular relaxation practices
Building Sustainable Habits
Prevention strategies work best when integrated naturally into your lifestyle. Consider these research-supported approaches:
- Start with small, manageable changes
- Build consistent routines gradually
- Focus on progress, not perfection
- Create supportive environments
- Develop backup plans for challenging situations
Understanding Prevention Benefits
Research shows that prevention offers significant advantages compared to treatment:
- Easier to maintain metabolic health than restore it
- Lower long-term health care costs
- Better quality of life outcomes
- Reduced risk of related health conditions
Key Takeaways for Prevention
Effective prevention of insulin resistance relies on:
- Regular implementation of evidence-based strategies
- Consistent monitoring of metabolic health markers
- Understanding and addressing environmental factors
- Building sustainable, long-term habits
Taking Control of Your Metabolic Health: Understanding and Acting on Insulin Resistance
As we’ve explored throughout this guide, insulin resistance is far more than just a precursor to diabetes – it’s a complex metabolic condition that can significantly impact your overall health and quality of life. Understanding its mechanisms, recognizing its signs, and knowing how to address it are crucial steps in maintaining long-term health.
Key Points to Remember
Let’s revisit the most important aspects of insulin resistance we’ve covered:
- Early Recognition Matters: Insulin resistance often develops silently, but early signs can be detected years before serious complications arise
- Beyond Blood Sugar: While glucose management is important, insulin resistance affects multiple body systems and aspects of health
- Prevention is Possible: Evidence-based lifestyle modifications can significantly impact your metabolic health
- Testing and Monitoring: Regular health assessments help track your metabolic health and guide interventions
Looking to the Future
Research continues to advance our understanding of insulin resistance. Emerging areas of study include:
- Personalized approaches to metabolic health
- Role of circadian rhythms in insulin sensitivity
- Impact of environmental factors on metabolic function
- New strategies for early intervention and prevention
Your Next Steps
Armed with this knowledge, you’re now better equipped to take control of your metabolic health. Consider these action steps:
- Assess your current health status and risk factors
- Implement evidence-based lifestyle modifications
- Establish regular health monitoring routines
- Work with healthcare professionals to develop personalized strategies
Remember, metabolic health is a journey, not a destination. Every positive step you take matters, and it’s never too early – or too late – to start improving your insulin sensitivity. Your actions today shape your health tomorrow.
By understanding insulin resistance and taking proactive steps to address it, you’re not just managing a health condition – you’re investing in your long-term wellbeing and quality of life. The science is clear: with the right knowledge and actions, you can make a significant difference in your metabolic health.
Moving Forward
Whether you’re just beginning to learn about insulin resistance or looking to deepen your understanding, remember that knowledge is power. Stay informed about the latest research, maintain open communication with healthcare providers, and most importantly, take consistent action toward better metabolic health.
Your journey to better metabolic health starts with understanding and continues with action. The steps you take today can lead to lasting improvements in your health and well-being.
To access other content on the IFitCenter’s blog, you can use the following links:
References for “Insulin Resistance in Simple Terms”
This article was developed using the following peer-reviewed research papers, books, and scientific resources:
- Zhang X, Zhang J, Yang X, et al. Trends in insulin resistance: insights into mechanisms and therapeutic targets. Signal Transduction and Targeted Therapy. 2022;7:1-32. DOI: 10.1038/s41392-022-01073-0.
- The crucial role and mechanism of insulin resistance in metabolic diseases. Frontiers in Endocrinology. 2023;14:1149239. DOI: 10.3389/fendo.2023.1149239.
- Spoto B, Pisano A, Zoccali C. Insulin resistance in chronic kidney disease: a systematic review. American Journal of Physiology-Renal Physiology. 2016;311(6):F1087-F1108. DOI: 10.1152/ajprenal.00340.2016.
- Pan PH, Liu YW, Chan YF, et al. Insulin resistance reduction, intermittent fasting, and human growth hormone: a randomized clinical trial. Nature Communications. 2024;15:1025. DOI: 10.1038/s44324-024-00025-2.
- Torjesen EA, Birkeland KI, Anderssen SA, et al. Lifestyle Changes May Reverse Development of the Insulin Resistance Syndrome: The Oslo Diet and Exercise Study: a randomized trial. Diabetes Care. 1997;20(1):26-31.





6 comments
Carmen Ruiz
Does stress really affect insulin resistance, or is that just a myth?
Dr.babak Jamalian
This is definitely not a myth. Chronic stress has a significant and well-documented impact on insulin sensitivity through multiple physiological pathways. When you experience prolonged stress, your body releases cortisol and other stress hormones that directly interfere with insulin signaling in your cells. This creates a metabolic environment that promotes glucose production by the liver while simultaneously reducing glucose uptake in muscle tissue-essentially a perfect storm for insulin resistance. Furthermore, stress often disrupts sleep patterns and promotes inflammatory processes, both of which further compromise insulin sensitivity. In our clinical practice, we consistently observe improvements in metabolic markers when patients implement effective stress management techniques alongside nutritional and exercise interventions. That’s why our approach to addressing insulin resistance always includes stress management strategies such as mindfulness practices, adequate sleep hygiene, and appropriate physical activity.
haifa
If I’ve been diagnosed with insulin resistance, how long would it take to reverse it with lifestyle changes?
Dr.babak Jamalian
Metabolic recovery follows a timeline that varies between individuals, but current research provides encouraging insights. With consistent implementation of appropriate interventions, cellular insulin sensitivity can begin improving within weeks. However, it’s important to understand this is a gradual process that typically progresses through several stages. Many patients notice initial improvements in energy levels and hunger patterns within the first month of intervention. More substantial metabolic flexibility usually begins returning within 2-3 months of consistent effort. Complete reversal depends on multiple factors including the severity and duration of insulin resistance, genetic factors, and adherence to therapeutic interventions. The key principle to remember is that early intervention yields better outcomes, and consistency matters more than intensity in achieving lasting metabolic health.
kevin
I’m at a healthy weight according to BMI charts, so I shouldn’t worry about insulin resistance, right?
Dr.babak Jamalian
This is actually a common misconception that I address frequently in my practice. While excess weight is certainly a risk factor, our recent research shows that approximately 20% of individuals with normal body weight demonstrate signs of insulin resistance-what we now term “metabolically unhealthy normal weight.” Your body composition, particularly visceral fat distribution, genetic factors, and lifestyle choices all play significant roles in developing insulin resistance, regardless of your BMI classification.