Have you ever wondered why diabetes is often called the “silent epidemic”? Or why some people can have diabetes for years without even knowing it? The reality might surprise you: according to the International Diabetes Federation, over 10% of the world’s adult population lives with diabetes—yet nearly half remain undiagnosed and unaware of their condition.
This alarming gap between those affected and those diagnosed raises critical questions: What makes diabetes so difficult to recognize? Why do early symptoms often go unnoticed? And most importantly, how can you identify the warning signs before serious complications develop?
At IFitCenter, we understand that recognizing diabetes early can make all the difference in managing the condition effectively. Our approach focuses on identifying the subtle signals your body sends when blood glucose regulation begins to falter—often long before conventional testing would detect a problem.
Drawing from Dr. Babak Jamalian’s extensive clinical experience and the latest research findings, this comprehensive guide will walk you through what diabetes really is, how it develops, the warning signs to watch for, and how proper diagnosis can set the foundation for effective management.
Whether you’re concerned about your own health, worried about a loved one, or simply want to be better informed, understanding diabetes is the first step toward taking control of your metabolic health.
What is Diabetes? Diabetes Explained in Simple Terms
Imagine your body as a sophisticated city with billions of cells, each requiring energy to function. Glucose—a type of sugar derived from the food you eat—is that essential energy source. But here’s the challenge: glucose can’t simply enter your cells on its own.
Think of it this way: If glucose is a visitor trying to enter a building (your cells), insulin is the key that unlocks the door. Without this key, glucose remains stuck outside, accumulating in your bloodstream while your cells essentially starve for energy.
“Many patients fixate on blood sugar numbers alone, but diabetes is fundamentally an energy distribution problem. When insulin function is compromised, your cells can be starving for energy even while glucose accumulates in your bloodstream. This paradox explains why untreated diabetes often causes both high blood sugar readings and extreme fatigue simultaneously.”
Dr. Babak Jamalian, Family Physician.
How Blood Glucose Regulation Works
In a healthy body, this system operates with remarkable precision. When you eat carbohydrates, your digestive system breaks them down into glucose, which enters your bloodstream. Your pancreas detects this rise in blood glucose and responds by producing insulin—the hormone that allows glucose to enter your cells.
As glucose moves from your bloodstream into your cells, your blood sugar levels naturally decline. Your body constantly balances glucose and insulin levels to keep your blood sugar within a narrow, healthy range—typically between 70 and 100 mg/dL when fasting.
When the System Malfunctions
Diabetes develops when this delicate balancing act breaks down in one of two fundamental ways:
- Insulin production problem: Your pancreas doesn’t produce enough insulin (or any at all)
- Insulin response problem: Your cells resist insulin’s effects, preventing glucose from entering efficiently
In either case, glucose accumulates in your bloodstream instead of entering your cells. This creates the paradoxical situation where your blood has excess glucose while your cells are essentially starving for energy—explaining why untreated diabetes often causes both high blood sugar readings and extreme fatigue simultaneously.
Over time, consistently elevated blood glucose levels damage blood vessels and nerves throughout your body. This progressive damage explains why uncontrolled diabetes can affect virtually every body system—from your eyes and kidneys to your heart and peripheral nerves.
The Different Faces of Diabetes: Types and Their Distinctions
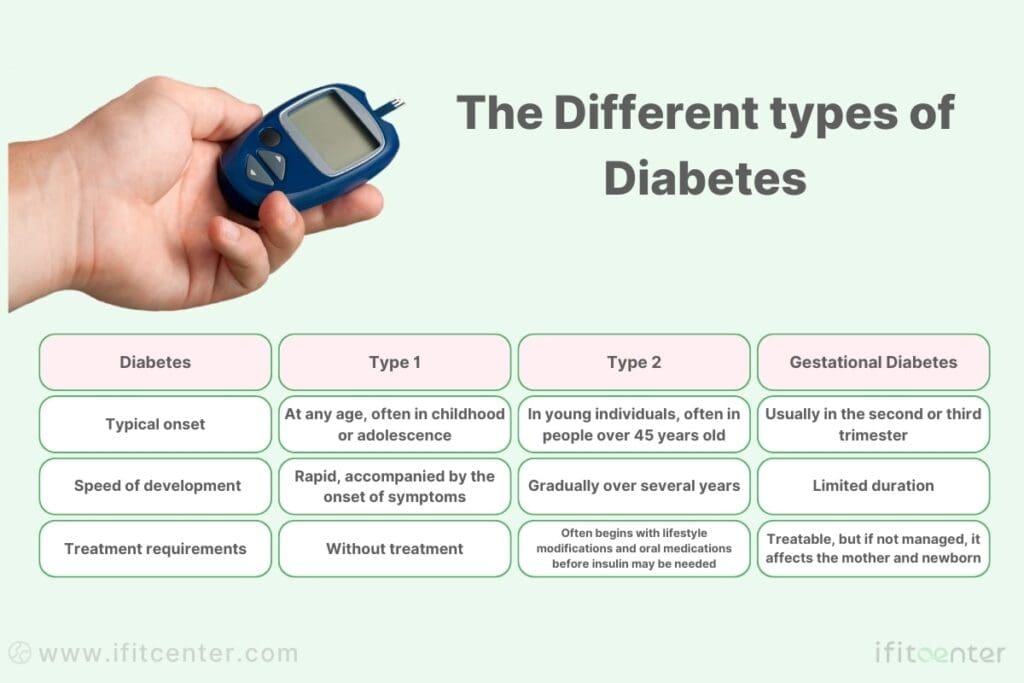
Diabetes isn’t a single condition but rather a group of metabolic disorders sharing the common feature of elevated blood glucose. Understanding the specific type of diabetes is crucial because it determines treatment approaches, progression patterns, and management strategies.
On the IFitCenter blog, we have provided a comprehensive guide for diabetes, completely free of charge and based on the latest research. By viewing these articles, in addition to increasing your general knowledge in this field, you can easily manage this disease in a principled manner. To access the first part of the articles, simply use the links below:
- Symptoms and Signs of Diabetes
- Difference Between Type 1 and Type 2 Diabetes
- What Are the Complications of Diabetes?
- Diabetes Diagnosis Method
- Is Diabetes Curable?
Type 1 Diabetes: When the Body Attacks Itself
Type 1 diabetes is fundamentally an autoimmune condition. The immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. Without these cells, the body cannot produce insulin, making external insulin administration essential for survival.
- Typical onset: Usually develops in childhood or adolescence, though it can appear at any age
- Speed of development: Often rapid, with symptoms appearing over days or weeks
- Treatment requirements: Lifelong insulin therapy, no known prevention method
Type 1 diabetes is not linked to lifestyle factors and cannot currently be prevented. However, with proper insulin management and regular monitoring, people with Type 1 diabetes can lead healthy, active lives.
Type 2 Diabetes: When Cells Stop Responding
Type 2 diabetes begins with insulin resistance—a condition where cells in the muscles, liver, and fat don’t respond properly to insulin. Initially, the pancreas compensates by producing more insulin, but over time, it cannot keep up with the demand, leading to elevated blood glucose levels.
- Typical onset: More common in adults over 45, but increasingly affecting younger populations
- Speed of development: Usually gradual, developing over years
- Treatment approach: Often begins with lifestyle modifications and oral medications before insulin may be needed
Unlike Type 1, Type 2 diabetes has strong connections to lifestyle factors including diet, physical activity levels, and body weight. This connection also means that Type 2 diabetes can often be prevented or its progression delayed through lifestyle modifications.
Gestational Diabetes: A Temporary But Serious Condition
Gestational diabetes develops during pregnancy when hormonal changes affect insulin function. While typically resolving after childbirth, it signals an increased risk for Type 2 diabetes later in life.
- Timing: Usually detected in the second or third trimester
- Risk factors: Previous gestational diabetes, family history of diabetes, PCOS, advanced maternal age
- Concerns: Can affect both mother and baby if not properly managed
Other Types: The Less Common Variants
Several less common forms of diabetes exist, including:
- MODY (Maturity-Onset Diabetes of the Young): Genetic forms that typically develop before age 25
- LADA (Latent Autoimmune Diabetes in Adults): A slow-progressing form of autoimmune diabetes often misdiagnosed as Type 2
- Secondary diabetes: Resulting from other conditions like pancreatic disease or certain medications.
Root Causes: Why Diabetes Develops
Understanding why diabetes develops requires examining multiple interconnected factors. While the two major types of diabetes have different primary causes, several underlying factors contribute to who develops diabetes and when.
Genetic Predisposition: The Blueprint of Risk
Genetic factors play a significant role in diabetes development across all types. Your genetic makeup can influence:
- Type 1 diabetes: The inheritance pattern involves multiple genes, particularly within the HLA complex related to immune function. Having a first-degree relative with Type 1 diabetes increases risk by approximately 15 times compared to the general population.
- Type 2 diabetes: Family history strongly influences risk, with multiple genes affecting insulin production, insulin sensitivity, and glucose metabolism. Having a parent with Type 2 diabetes increases lifetime risk to 40%, and this rises to nearly 70% if both parents have the condition.
genetic predisposition creates vulnerability, but it rarely determines destiny on its own. This explains why identical twins—sharing identical DNA—don’t always both develop diabetes, pointing to the crucial role of environmental factors.
Environmental Triggers: The Activation Factors
Environmental factors can trigger diabetes development in genetically susceptible individuals:
- For Type 1 diabetes: Viral infections, particularly enteroviruses, may trigger the autoimmune response in susceptible individuals. Early life exposures, including certain dietary factors during infancy, may also play a role.
- For Type 2 diabetes: Environmental factors are even more significant, with modern lifestyle changes driving the worldwide increase in prevalence. Urbanization, increased access to processed foods, and decreased physical activity create the conditions where genetic susceptibility translates into actual disease.
Lifestyle Elements: The Daily Choices That Matter
Lifestyle factors have a profound impact on Type 2 diabetes risk and, to some extent, can influence how Type 1 diabetes progresses:
- Dietary patterns: High consumption of refined carbohydrates, sugar-sweetened beverages, and processed foods is strongly linked to increased diabetes risk. These foods cause rapid blood glucose spikes, placing stress on insulin-producing cells.
- Physical inactivity: Regular physical activity enhances insulin sensitivity, while sedentary behavior promotes insulin resistance. Muscles that remain inactive require more insulin to absorb the same amount of glucose.
- Stress levels: Chronic stress increases cortisol production, which raises blood glucose levels and promotes abdominal fat storage—a significant risk factor for insulin resistance.
- Sleep patterns: Poor sleep quality and insufficient sleep duration are linked to impaired glucose tolerance and insulin resistance.
The Obesity-Insulin Resistance Connection
One of the strongest risk factors for Type 2 diabetes is excess weight, particularly when fat accumulates around the abdomen (visceral fat). This connection works through several mechanisms:
- Visceral fat releases inflammatory chemicals that interfere with insulin signaling
- Fat cells release fatty acids that promote insulin resistance in muscle and liver tissues
- Excess fat storage in the liver and pancreas directly impairs insulin production and function
It’s important to note that while obesity increases risk dramatically, not everyone with obesity develops diabetes, and not everyone with Type 2 diabetes is obese—again highlighting the interplay between genetic susceptibility and environmental factors.
To access the second part of the articles related to diabetes, you can use the following links:
- The Difference Between Prediabetes and Diabetes
- Insulin Resistance and Diabetes
- Understanding Blood Sugar Numbers
- Weight Loss for Type 2 Diabetes
- What is Type 2 Diabetes
- Best Fruits for Blood Sugar Control
Diabetes Early Warning Signs: Diabetes Symptoms You Shouldn’t Ignore
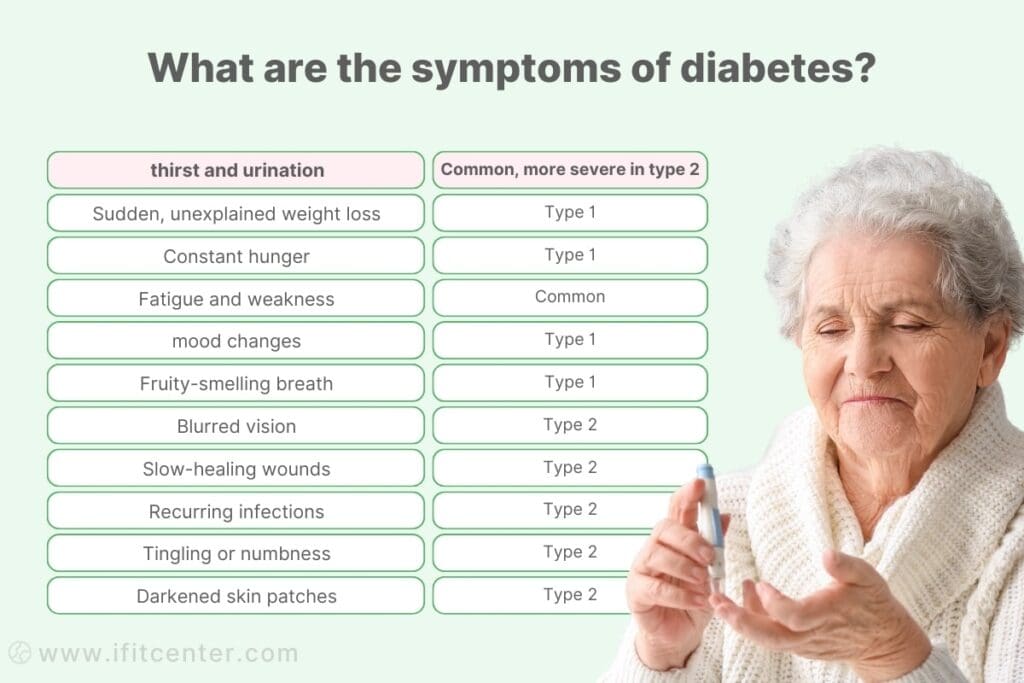
Diabetes often develops silently, with symptoms that are easy to dismiss or attribute to other causes. Recognizing these warning signs early can lead to prompt diagnosis and treatment, potentially preventing serious complications. Here’s what to watch for:
Type 1 Diabetes: Rapid Onset Symptoms
Type 1 diabetes typically presents with symptoms that develop relatively quickly—often over days to weeks. Because the body stops producing insulin almost completely, symptoms tend to be more severe and noticeable:
- Extreme thirst and frequent urination: When blood glucose levels are high, the kidneys work overtime to filter and absorb the excess glucose. When they can’t keep up, this excess glucose is excreted into the urine, drawing water along with it. This triggers more frequent urination, which may lead to dehydration and extreme thirst.
- Sudden, unexplained weight loss: Without insulin, the body cannot use glucose for energy, so it begins breaking down fat and muscle tissue instead. This can cause rapid weight loss even without changes in eating habits.
- Constant hunger: Despite eating normally or even more than usual, the cells are starving because they cannot access glucose without insulin.
- Fatigue and weakness: When cells cannot access glucose for energy, extreme fatigue and weakness result.
- Irritability and mood changes: Fluctuating blood sugar levels can affect mood and mental clarity.
- Fruity-smelling breath: When the body breaks down fat for energy, ketones are produced and can cause breath to smell fruity or like acetone.
Type 1 diabetes can sometimes develop extremely rapidly, leading to a life-threatening condition called diabetic ketoacidosis (DKA). Seek immediate medical attention if severe symptoms appear, especially in children and young adults.
Type 2 Diabetes: The Gradual Progression
Type 2 diabetes often develops much more gradually, with symptoms that may be subtle and easy to overlook for years. Many people discover they have Type 2 diabetes during routine blood tests before they notice any symptoms. Common signs include:
- Increased thirst and urination: Similar to Type 1 but often less dramatic
- Fatigue: Persistent tiredness that doesn’t improve with rest
- Blurred vision: Fluctuating blood glucose levels can cause temporary changes in eye fluid, affecting vision clarity
- Slow-healing wounds: High blood glucose impairs circulation and immune function, making healing slower
- Recurring infections: Particularly yeast infections, urinary tract infections, and skin infections
- Tingling or numbness in hands and feet: An early sign of nerve damage from elevated blood glucose
- Darkened skin patches: Particularly in the neck, armpits, and groin—a condition called acanthosis nigricans that signals insulin resistance
Lesser-Known Warning Signs
Beyond the classic symptoms, several lesser-known signs may indicate developing diabetes:
- Skin changes: Various skin conditions can signal diabetes, including:
- Vision fluctuations: Rapidly changing vision clarity throughout the day
- Gum disease and dental problems: Higher blood glucose levels increase risk for oral health issues
- Hearing difficulties: Diabetes can affect the small blood vessels and nerves in the ears
- Changes in sexual function: Men may experience erectile dysfunction; women may notice vaginal dryness or recurrent yeast infections
The Diagnostic Process: How Diabetes is Identified
Accurate diabetes diagnosis is crucial for proper management. Several testing methods can identify diabetes, each measuring blood glucose levels in different ways.
Standard Diagnostic Criteria for Diabetes
According to guidelines cited in the medical literature, diabetes is diagnosed when one or more of these criteria are met:
- Fasting blood glucose ≥ 126 mg/dL
- Two-hour blood glucose ≥ 200 mg/dL during an oral glucose tolerance test
- HbA1c ≥ 6.5%
- Random blood glucose ≥ 200 mg/dL with symptoms of hyperglycemia
Fasting Plasma Glucose Test: The Baseline Measurement
The fasting glucose test measures blood sugar after an overnight fast (at least 8 hours without food). This test requires proper preparation for accurate results.
- Procedure: A blood sample is taken after fasting
- Interpretation:
- Normal: Below 100 mg/dL
- Prediabetes: 100-125 mg/dL
- Diabetes: 126 mg/dL or higher (confirmed with a second test)
Oral Glucose Tolerance Test: Measuring Response to Sugar
The OGTT evaluates how your body processes glucose after consuming a sweet solution containing 75 grams of glucose.
- Procedure: Blood is drawn before drinking the solution and again 2 hours later
- Best used for: Gestational diabetes screening and when fasting tests appear normal but diabetes is suspected
- Interpretation:
- Normal: Below 140 mg/dL at 2 hours
- Prediabetes: 140-199 mg/dL at 2 hours
- Diabetes: 200 mg/dL or higher at 2 hours
HbA1c Test: The Three-Month Blood Sugar Average
The HbA1c test measures the percentage of hemoglobin with attached glucose, providing a longer-term view of blood glucose levels.
- Advantage: Doesn’t require fasting and reflects glucose control over approximately 3 months
- Interpretation:
- Normal: Below 5.7%
- Prediabetes: 5.7% to 6.4%
- Diabetes: 6.5% or higher
According to the Diabetes UK educational materials, “HbA1c provides a better indication of long-term glucose control and has been shown to correlate with the risk of diabetes complications.”
Random Blood Glucose Test: Testing Without Preparation
A random blood glucose test can be performed at any time, regardless of when you last ate.
- When it’s appropriate: When symptoms of diabetes are present and immediate testing is needed
- Interpretation: 200 mg/dL or higher, along with symptoms like excessive thirst and urination, suggests diabetes
Additional Diagnostic Tests for Specific Diabetes Types
Further testing may be needed to determine the specific type of diabetes:
- Autoantibody tests: Help distinguish Type 1 diabetes by detecting immune system antibodies against insulin-producing cells
- C-peptide test: Measures how much insulin your body produces naturally, helping differentiate between diabetes types
- Genetic testing: May identify specific forms of diabetes like MODY (Maturity-Onset Diabetes of the Young)
Beyond Blood Sugar: Understanding Your Test Results
Receiving diabetes test results can be confusing. Understanding what these numbers mean is crucial for making informed decisions about your health.
“Conventional diabetes screening often misses early metabolic dysfunction. I’ve seen many patients with ‘normal’ fasting glucose but significant insulin resistance already developing. Testing for fasting insulin levels and post-meal glucose responses can reveal problems years before standard tests show abnormalities, giving us a much wider window for effective intervention.”
Dr. Babak Jamalian, Family Physician.
Interpreting Glucose Test Numbers
When looking at blood glucose test results, the key thresholds to remember are:
| Test Type | Normal | Prediabetes | Diabetes |
|---|---|---|---|
| Fasting Glucose | <100 mg/dL | 100-125 mg/dL | ≥126 mg/dL |
| 2-hour OGTT | <140 mg/dL | 140-199 mg/dL | ≥200 mg/dL |
| HbA1c | <5.7% | 5.7-6.4% | ≥6.5% |
As explained in the resources from Diabetes UK, these numbers reflect different aspects of glucose metabolism. A fasting glucose of 100 mg/dL represents about one teaspoon of sugar in your entire blood volume—a surprisingly small amount that highlights how precisely the body normally regulates blood sugar.
Understanding Prediabetes: The Critical Warning Stage
Prediabetes test results indicate that your glucose regulation system is already compromised, though not yet to the level of full diabetes. This stage represents a crucial opportunity for intervention.
- HbA1c of 5.7-6.4%: Indicates higher average blood sugar over the past 3 months than optimal
- Fasting glucose of 100-125 mg/dL: Shows impaired fasting glucose
- OGTT 2-hour result of 140-199 mg/dL: Reveals impaired glucose tolerance
Many people discover they’re in the early stages of blood sugar imbalance without realizing that this is the perfect time to take control. At this stage, structured weight loss can help relieve pressure on the pancreas, improve insulin sensitivity, and stabilize blood sugar—all without extreme diets or medications.
At iFitCenter, we don’t offer a one-size-fits-all solution. We start with a full metabolic assessment, then create a personalized plan designed to help reduce fat around the liver and pancreas, restore balance to your glucose metabolism, and support sustainable lifestyle changes with close medical supervision.
If your recent test results fall into the prediabetic range—or if you simply want to protect your long-term health—our team is ready to help.
Insulin Testing: Going Deeper Than Glucose
Standard diabetes tests focus on glucose levels, but insulin testing provides additional insights. As Dr. Berg emphasizes in his educational videos, insulin resistance often begins years before blood sugar levels rise.
- Fasting insulin: Elevated levels (above 5 μIU/mL) may indicate insulin resistance even with normal glucose
- HOMA-IR (Homeostatic Model Assessment of Insulin Resistance): Calculated using fasting glucose and insulin measurements to assess insulin resistance
- Insulin response during OGTT: Excessive insulin production after glucose ingestion can indicate early metabolic dysfunction
Additional Biomarkers That Provide Context
Several other laboratory tests help provide a more complete picture of metabolic health:
- Lipid Profile: Diabetes often accompanies dyslipidemia, with elevated triglycerides and low HDL cholesterol being particularly significant
- Liver Function Tests: Non-alcoholic fatty liver disease frequently accompanies insulin resistance
- Inflammatory Markers: Chronic inflammation plays a role in diabetes development
- Kidney Function Tests: Early detection of kidney changes helps prevent diabetic nephropathy
What Do Borderline Results Really Mean?
Borderline results deserve attention rather than dismissal. They often indicate that metabolic changes are underway but haven’t yet progressed to diagnosable diabetes.
- Slightly elevated fasting glucose (100-105 mg/dL): May indicate early insulin resistance
- HbA1c in the lower prediabetic range (5.7-5.9%): Shows that blood sugar control is beginning to slip
- Normal fasting glucose with elevated post-meal levels: Can identify problems that fasting tests miss
According to established research, people with prediabetes have a 74% higher risk of progressing to type 2 diabetes than those with normal glucose levels. The good news is that this progression isn’t inevitable—lifestyle modifications can significantly reduce this risk.
Understanding your test results empowers you to take appropriate action based on your specific metabolic profile. Whether your results indicate normal function, prediabetes, or diabetes, knowing where you stand is the first step toward optimal health.
When Diabetes Goes Undetected: Understanding Complications
Undiagnosed or poorly managed diabetes can lead to serious health complications. Understanding these potential consequences emphasizes the importance of early detection and proper management.
Short-Term Complications: Acute Metabolic Emergencies
Undetected diabetes can lead to acute metabolic emergencies that require immediate medical attention:
- Diabetic Ketoacidosis (DKA): Primarily affects people with Type 1 diabetes. Without insulin, the body breaks down fat too quickly, producing ketones that make the blood acidic. Symptoms include fruity-smelling breath, deep labored breathing, confusion, and even coma.
- Hyperosmolar Hyperglycemic State (HHS): More common in Type 2 diabetes, this condition involves extremely high blood sugar levels (often over 600 mg/dL) causing severe dehydration. It develops more slowly than DKA but can be equally dangerous.
According to the medical resources reviewed, these acute complications can develop within days or weeks of diabetes onset, particularly in Type 1 diabetes, and may be the first indication of the condition.
Long-Term Complications: The Silent Damage
Chronic elevation of blood glucose damages blood vessels and nerves throughout the body, leading to complications that develop gradually over years:
- Cardiovascular Disease: Diabetes significantly increases the risk of heart attack, stroke, and peripheral artery disease. Small and large blood vessels throughout the body are damaged by chronic high blood glucose.
- Nerve Damage (Neuropathy): High blood sugar damages nerves, particularly in the legs and feet, causing numbness, tingling, pain, or complete loss of sensation. As Dr. Berg points out in his videos, this “peripheral neuropathy” is one of the most common complications of long-standing diabetes.
- Kidney Damage (Nephropathy): Diabetes is a leading cause of kidney failure. The kidneys’ filtering system becomes damaged, initially allowing small amounts of protein to leak into urine (microalbuminuria) before progressing to more severe dysfunction.
- Eye Damage (Retinopathy): Diabetes can damage the small blood vessels in the retina, potentially leading to vision impairment or blindness. The condition called “diabetic retinopathy” is a leading cause of blindness in working-age adults.
- Foot Complications: Combined nerve damage and poor circulation can lead to serious foot problems, including ulcers and infections that may ultimately require amputation.
The Timeline of Complication Development
Understanding when complications typically develop can help emphasize the importance of early intervention:
- Years 0-5: Subtle changes in blood vessels and nerves may begin but are often not detectable through symptoms
- Years 5-10: Early signs of complications may appear, including minor nerve symptoms and early kidney changes
- Years 10-15: More significant complications become apparent, including moderate retinopathy and neuropathy
- Years 15+: Advanced complications can develop, including severe vision problems, kidney failure, and cardiovascular events
Importantly, this timeline is highly variable and influenced by how well blood glucose is controlled, genetic factors, and other health conditions.
Early Intervention: The Power of Prevention
The good news is that detecting diabetes early and implementing proper management significantly reduces the risk of complications:
- Blood Glucose Control: Managing blood glucose levels within target ranges can reduce the risk of complications by 25-70%, depending on the specific complication
- Regular Screening: Early detection of complications allows for immediate intervention
- Comprehensive Approach: Addressing related risk factors like blood pressure and cholesterol provides additional protection
As explained in the Diabetes UK materials, many complications can be prevented entirely or significantly delayed with proper diabetes management and regular screening for early signs of problems.
Conclusion
Understanding diabetes—from its underlying mechanisms and warning signs to diagnostic procedures and potential complications—provides a foundation for proactive health management. As we’ve explored throughout this article, diabetes develops through distinct metabolic changes that can often be detected early with proper attention to symptoms and appropriate testing.
Key takeaways from our exploration include:
- Diabetes results from impaired glucose regulation due to either insufficient insulin production or ineffective insulin action
- Different types of diabetes (Type 1, Type 2, gestational) have distinct causes and characteristics but share the common feature of elevated blood glucose
- Early warning signs like increased thirst, frequent urination, and unexplained fatigue deserve attention and proper evaluation
- Various diagnostic tests offer complementary information about glucose metabolism and overall metabolic health
- Understanding test results in context allows for appropriate intervention, particularly during the critical prediabetes stage
- Early detection and intervention significantly reduce the risk of serious complications
To access other content on the IFitCenter’s blog, you can use the following links:
References
- Madurapperumage Anuradha Erandathi, William Yu Chung Wang, Michael Mayo, Ching-Chi Lee. Comprehensive Factors for Predicting the Complications of Diabetes Mellitus: A Systematic Review. Curr Diabetes Rev. 2024;20(9):e040124225240. DOI: 10.2174/0115733998271863231116062601
- Matti Uusitupa, Tauseef A Khan, Effie Viguiliouk, Hana Kahleova, Angela A Rivellese, Kjeld Hermansen, Andreas Pfeiffer, Anastasia Thanopoulou, Jordi Salas-Salvadó, Ursula Schwab, John L Sievenpiper. Prevention of Type 2 Diabetes by Lifestyle Changes: A Systematic Review and Meta-Analysis. Nutrients. 2019;11(11):2611. DOI: 10.3390/nu11112611
- Karla Ivette Galaviz, Mary Beth Weber, Audrey Straus, Jeehea Sonya Haw, KM Venkat Narayan, Mohammed Kumail Ali. Global Diabetes Prevention Interventions: A Systematic Review and Network Meta-analysis of the Real-World Impact on Incidence, Weight, and Glucose. Diabetes Care. 2018;41(7):1526–1534. DOI: 10.2337/dc17-2222
- Annika Rosengren, Pigi Dikaiou. Cardiovascular outcomes in type 1 and type 2 diabetes. Diabetologia. 2023;66(3):425–437. DOI: 10.1007/s00125-022-05857-5
- Weronika Bielka, Agnieszka Przezak, Andrzej Pawlik. The Role of the Gut Microbiota in the Pathogenesis of Diabetes. Int. J. Mol. Sci. 2022;23(1):480. DOI: 10.3390/ijms23010480
- Danijela Tatovic, Ashish Marwaha, Peter Taylor, Stephanie J. Hanna, Kym Carter, W. Y. Cheung, Steve Luzio, Gareth Dunseath, Hayley A. Hutchings, Gail Holland, Steve Hiles, Greg Fegan, Evangelia Williams, Jennie H. M. Yang, Clara Domingo-Vila, Emily Pollock, Muntaha Wadud, Kirsten Ward-Hartstonge, Susie Marques-Jones, Jane Bowen-Morris, Rachel Stenson, Megan K. Levings, John W. Gregory, Timothy I. M. Tree; USTEKID Study Group. Ustekinumab for type 1 diabetes in adolescents: a multicenter, double-blind, randomized phase 2 trial. Nature Medicine. 2024;30:2657–2666. DOI: 10.1038/s41591-024-03115-2
- Hao Liu, Jianguo Feng, Liling Tang. Early renal structural changes and potential biomarkers in diabetic nephropathy. Frontiers in Physiology. 2022;13:1020443. DOI: 10.3389/fphys.2022.1020443



