Think salt is the main cause of high blood pressure? Think again. While limiting sodium intake has been the cornerstone of hypertension advice for decades, recent research reveals this approach addresses just one piece of a much larger puzzle. In fact, studies show that for many people, factors like insulin resistance and chronic inflammation may play a far more significant role in elevating blood pressure than salt consumption alone. Understanding the true causes of high blood pressure requires looking beyond the salt shaker and examining the complex interplay of metabolic, genetic, and lifestyle factors.
Hypertension affects nearly 1.3 billion people worldwide and contributes to over 10 million deaths annually, yet misconceptions about its causes persist. Many patients diligently cut salt only to find their blood pressure remains stubbornly high. Others believe hypertension is simply “genetic” and therefore unmanageable, missing crucial opportunities for prevention. Today at IFitCenter, we’re cutting through the myths to explore what truly drives this silent epidemic and how understanding these factors can empower you to take control of your cardiovascular health.
Primary vs. Secondary Hypertension: Understanding the Difference
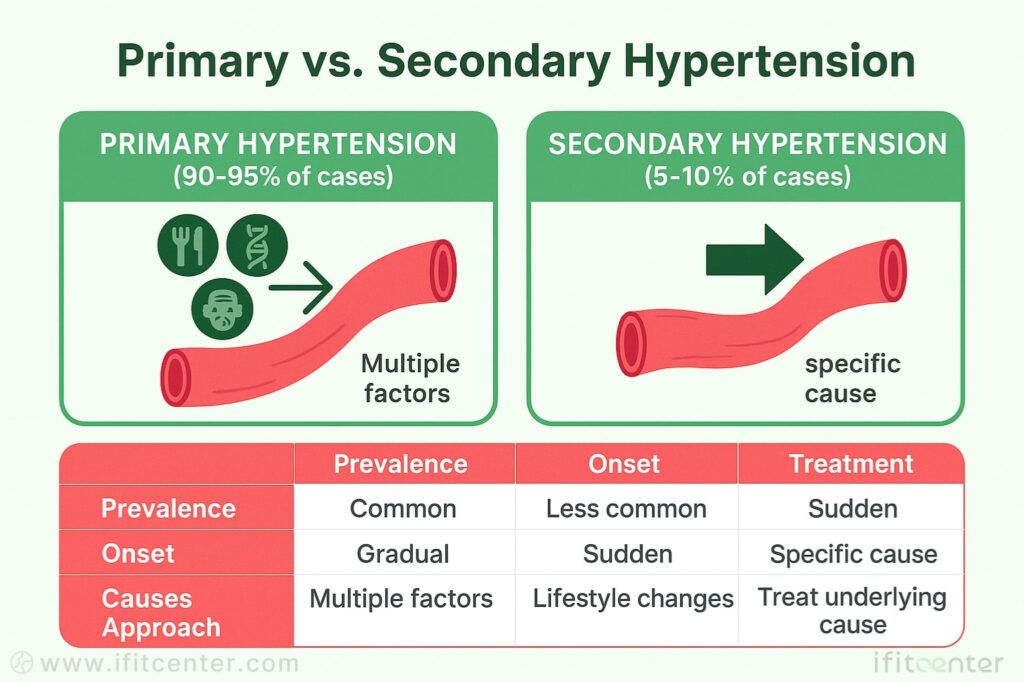
When doctors diagnose high blood pressure, they categorize it into two fundamental types: primary and secondary hypertension. Understanding this distinction is crucial because it directly affects how your condition should be approached and treated.
Primary (Essential) Hypertension: The Common Culprit
Primary hypertension, also called essential hypertension, accounts for 90-95% of all high blood pressure cases. Think of it as a puzzle with multiple pieces – there’s no single identifiable cause, but rather a combination of factors working together.
Primary hypertension typically develops gradually over many years. It’s like a slow-boiling pot that eventually overflows – your blood vessels progressively stiffen, your kidney function subtly changes, and various metabolic shifts occur until one day, your blood pressure reading crosses into the high range.
Secondary Hypertension: When There’s a Clear Cause
Secondary hypertension accounts for just 5-10% of cases but demands special attention. Unlike primary hypertension, secondary hypertension has a specific, identifiable cause – a medical condition or medication that’s driving your blood pressure up. It’s like having a tack in your tire – no matter how much air you add, the pressure won’t stabilize until you address the puncture.
This type often appears suddenly and causes higher blood pressure readings than primary hypertension. According to research, up to 20% of people with resistant hypertension (high blood pressure that doesn’t respond well to multiple medications) actually have an undiagnosed secondary cause.
| Characteristic | Primary Hypertension | Secondary Hypertension |
|---|---|---|
| Prevalence | 90-95% of cases | 5-10% of cases |
| Onset | Gradual, over years | Often sudden |
| Cause | Multiple factors combined | Specific identifiable cause |
| Blood pressure levels | Usually moderate elevation | Often more severe elevation |
| Age pattern | More common with increasing age | Can affect any age but more common in specific groups |
Why This Distinction Matters
The approach to treating these two types differs significantly. For primary hypertension, treatment typically involves addressing multiple contributing factors simultaneously – similar to fixing various leaks in a water system. For secondary hypertension, the focus is on treating the underlying cause – more like repairing the main valve.
According to a study published in the European Journal of Epidemiology, identifying and correcting the underlying cause of secondary hypertension can sometimes completely resolve high blood pressure, eliminating the need for lifelong medication. This is why proper diagnosis is crucial.
“In secondary hypertension, treating the underlying cause is often the most effective approach. Unfortunately, this cause is frequently missed because many healthcare providers don’t look beyond the primary diagnosis.”
Throughout this article, we’ll explore the main causes of high blood pressure in both categories, beginning with the factors that contribute to primary hypertension, followed by the specific conditions that can trigger secondary hypertension. Understanding these causes is the first step toward effective management and potential reversal of high blood pressure.
Insulin Resistance: A Hidden Driver of High Blood Pressure
When discussing what causes high blood pressure, insulin resistance rarely gets the attention it deserves. While insulin resistance is not the sole driver of hypertension, research indicates it plays a significant role in 31-50% of primary hypertension cases, particularly when combined with obesity
On the IFitCenter blog, we have prepared a free information database about various diseases, including high blood pressure, for you, our dear readers. By reviewing these resources, you will gain valuable information for controlling and preventing these conditions. To access the first part of the information, you can use the links below:
- What Is Normal Blood Pressure?
- Blood Pressure Chart
- How to Measure Blood Pressure
- Hypertension symptoms
- How to Lower Blood Pressure Immediately
What Is Insulin Resistance?
Insulin resistance occurs when your cells don’t respond properly to insulin, the hormone that regulates blood sugar. Think of insulin as a key that unlocks your cells to let glucose inside. With insulin resistance, the locks on your cells change, making the key less effective. Your pancreas then produces more insulin to compensate, leading to higher insulin levels in your bloodstream.
While most people associate insulin resistance with diabetes, its effects extend far beyond blood sugar regulation – it directly impacts your blood vessels and kidneys, both critical for blood pressure control.
How Insulin Resistance Raises Blood Pressure
Insulin resistance affects blood pressure through several key mechanisms:
- Sodium Retention: Insulin promotes sodium retention in the kidneys. When you’re insulin resistant, the compensatory high insulin levels cause your body to hold onto more sodium and water, increasing blood volume and pressure.
- Sympathetic Nervous System Activation: Insulin resistance activates your sympathetic nervous system – your body’s “fight or flight” response. This increases heart rate and constricts blood vessels, both of which raise blood pressure.
- Blood Vessel Damage: The inflammatory environment created by insulin resistance damages blood vessel walls, reducing their elasticity and making them stiffer. Stiff vessels require more pressure to pump blood through them.
- Disrupted Nitric Oxide Production: Insulin normally helps produce nitric oxide, which relaxes blood vessels. In insulin resistance, this pathway is selectively impaired, leading to increased vasoconstriction.
The Evolutionary Perspective
Interestingly, the link between insulin resistance and hypertension may have evolutionary roots. Research suggests this connection might have been beneficial for our ancestors during times of starvation or infection. Higher blood pressure from insulin resistance would ensure adequate blood flow to the brain during food scarcity or to fight infections.
In our modern environment of abundant food and sedentary lifestyles, however, this once-adaptive mechanism has become harmful, contributing to chronic hypertension.
Identifying Insulin Resistance
Common signs of insulin resistance include:
- Waist circumference over 40 inches (men) or 35 inches (women)
- Skin tags or darkened skin patches (acanthosis nigricans)
- Elevated triglycerides and low HDL cholesterol
- High blood pressure despite low sodium intake
If you have hypertension that doesn’t respond well to standard treatments, insulin resistance could be an underlying factor worth investigating with your healthcare provider.
“In my clinical experience, insulin resistance is the hidden driver behind many cases of resistant hypertension. While most patients focus exclusively on salt intake, I’ve observed that addressing metabolic health often normalizes blood pressure more effectively than sodium restriction alone. Many patients are surprised to learn that improving insulin sensitivity through dietary changes can reduce their need for blood pressure medications, sometimes eliminating them altogether. This connection between metabolism and blood pressure remains one of the most underutilized insights in hypertension management.”
Dr. Babak Jamalian, Family Physician
Obesity and Body Composition: Key Causes for High Blood Pressure
Among the significant causes for high blood pressure, excess weight stands out as one of the most modifiable risk factors. Research consistently shows a direct relationship between body weight and blood pressure levels.
To access the second section of blood pressure articles, I invite you to use the links below:
- dash diet for hypertension
- complications of hypertension
- Best foods for hypertension
- Foods to Avoid with hypertension
- is green tea good for hypertension?
- is coffee good for hypertension?
- Sudden high blood pressure with headache
Does being obese cause high blood pressure? - fasting benefits for high blood pressure
How Excess Weight Raises Blood Pressure
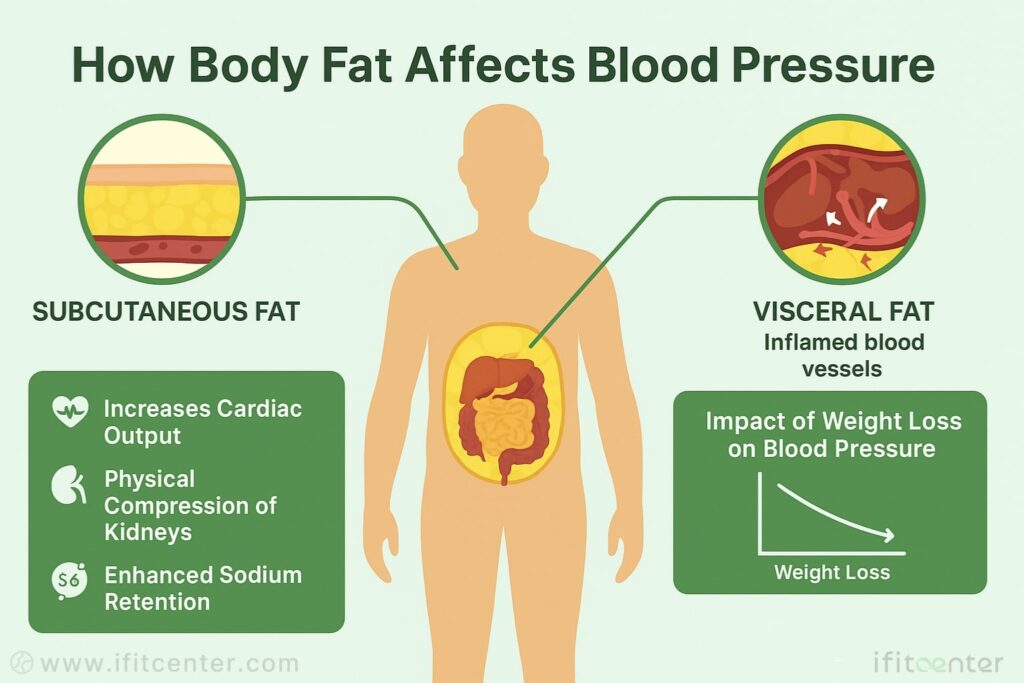
The relationship between obesity and hypertension involves several mechanisms:
- Increased Cardiac Output: Excess weight requires your heart to pump more blood to supply the additional tissue, increasing pressure within your blood vessels.
- Physical Compression: Extra weight physically compresses your kidneys, affecting their ability to regulate blood pressure.
- Enhanced Sodium Retention: Obesity changes how your kidneys handle sodium, causing your body to retain more fluid.
Not All Fat Is Created Equal: Visceral vs. Subcutaneous
The location of excess fat matters significantly. Visceral fat (deep abdominal fat surrounding your organs) poses a much greater risk for hypertension than subcutaneous fat (the fat just under your skin).
Think of visceral fat as an active organ rather than just stored energy. Unlike subcutaneous fat (which you can pinch), visceral fat wraps around your internal organs and actively produces compounds that raise blood pressure.
Adipose Tissue: More Than Just Fat Storage
Modern research reveals that adipose tissue functions as an endocrine organ, producing hormones and other biologically active substances:
- Inflammatory Cytokines: Visceral fat releases inflammatory compounds that damage blood vessels and reduce their elasticity.
- Angiotensinogen: Fat cells produce this compound, which converts to angiotensin II, a powerful blood vessel constrictor.
- Altered Adiponectin Levels: Obesity reduces levels of adiponectin, a protective hormone that helps maintain blood vessel health.
The Impact of Weight Loss on Blood Pressure
The good news is that even modest weight loss can significantly reduce blood pressure. Research shows that losing just 5-10% of your body weight can lower systolic blood pressure by 5-20 mmHg. For someone with a blood pressure of 150/90 mmHg, this reduction could bring readings into a much healthier range.
Weight loss has a dose-dependent effect on blood pressure – the more weight lost, the greater the improvement in blood pressure readings, particularly when the weight loss comes from the abdominal area.
Lower Blood Pressure Naturally at IFitCenter
Understanding what causes high blood pressure is the first step—addressing it starts with your lifestyle. At IFitCenter, Dr. Babak Jamalian leads evidence-based weight-loss and metabolic health programs proven to help reverse some of the root causes of hypertension:
✔ Personalized nutrition plans targeting insulin resistance
✔ Safe, sustainable weight-loss strategies that reduce vascular strain
✔ Medical oversight to track progress and adjust as needed
Begin your personalized journey to lower blood pressure today.
Dietary Factors: Beyond the Number One Food That Causes High Blood Pressure
When discussing the number one food that causes high blood pressure, most people immediately think of salt. While sodium intake is important, the dietary picture is far more complex.
The Sodium-Potassium Balance: More Important Than Sodium Alone
Modern research suggests the ratio between sodium and potassium may be more crucial than sodium intake alone. Our ancestors consumed a diet with 10 times more potassium than sodium, but today’s typical diet contains 10 times more sodium than potassium – a complete reversal with significant consequences for blood pressure.
Potassium helps your body excrete sodium and relaxes blood vessel walls. When potassium levels are insufficient, even moderate sodium intake can raise blood pressure significantly.
“The sodium-potassium balance is far more crucial for blood pressure regulation than sodium alone. Many patients meticulously avoid salt while consuming diets severely deficient in potassium-rich foods. This imbalance is particularly problematic because potassium actively helps excrete excess sodium and relaxes blood vessel walls. I’ve found that patients who focus on increasing vegetables, fruits, and other potassium sources often achieve better blood pressure control than those who only restrict salt. It’s about creating balance rather than simply eliminating one mineral.”
Dr. Babak Jamalian, Family Physician
Processed Foods: The Hidden Sodium Source
Most dietary sodium (over 70%) comes from processed and restaurant foods, not from salt added during home cooking or at the table. Manufacturers add significant amounts of sodium to foods for flavor, texture, and preservation.
Common high-sodium processed foods include:
- Bread and rolls
- Pizza
- Sandwiches
- Cold cuts and cured meats
- Soups
- Burritos and tacos
- Savory snacks (chips, crackers, pretzels)
- Cheese
- Boxed pasta meals
Beyond Sodium: Other Dietary Factors
Several other dietary components significantly impact blood pressure:
- Added Sugars and Refined Carbohydrates: High consumption increases insulin levels, promoting sodium retention and blood vessel constriction. Research suggests sugar may impact blood pressure more than salt for many people.
- Alcohol: Regular consumption of more than 1-2 drinks daily raises blood pressure by multiple mechanisms, including nervous system activation and hormone disruption.
- Insufficient Minerals: Low intake of magnesium, calcium, and potassium all contribute to hypertension. These minerals help regulate blood vessel function and fluid balance.
- Excessive Caffeine: Can cause temporary spikes in blood pressure, though tolerance develops in regular consumers. Individual sensitivity varies significantly.
The DASH Diet Approach
The Dietary Approaches to Stop Hypertension (DASH) diet emphasizes fruits, vegetables, whole grains, lean proteins, and low-fat dairy while limiting sodium, sweets, and red meats. Research shows this approach can lower systolic blood pressure by 8-14 mmHg, comparable to some medications.
What makes the DASH diet effective isn’t just sodium reduction but the combined effect of multiple nutrients working together to optimize blood pressure.
In the second part of our blog content introduction, we have prepared valuable articles in the field of healthy nutrition and weight loss for you. To access them, simply use the links below:
- how to make healthy food tasty
- recognizing food craving patterns
- preserve muscle during medical weight loss
- why diets fail
Chronic Inflammation: One of the Hidden Causes of High Blood Pressure Hypertension
Among the less recognized causes of high blood pressure hypertension, chronic inflammation stands out as a significant yet often overlooked factor. Modern research increasingly points to inflammation as a key driver in the development and progression of hypertension.
How Inflammation Damages Blood Vessels
Inflammation affects blood pressure through several mechanisms:
- Endothelial Dysfunction: Inflammation damages the endothelium, the thin layer of cells lining your blood vessels. This impairs their ability to dilate properly, resulting in increased resistance and higher pressure.
- Arterial Stiffening: Inflammatory processes promote arterial wall thickening and loss of elasticity, reducing the vessels’ ability to accommodate pressure changes.
- Sodium Retention: Certain inflammatory pathways can increase sodium retention in the kidneys, expanding blood volume and raising pressure.
Oxidative Stress: The Silent Blood Vessel Damager
Closely related to inflammation is oxidative stress, which occurs when free radicals (reactive oxygen species) overwhelm your body’s antioxidant defenses. This imbalance plays a critical role in hypertension by:
- Reducing Nitric Oxide: Oxidative stress depletes nitric oxide, a molecule that relaxes blood vessels. With less nitric oxide, vessels remain constricted and pressure rises.
- Promoting Vascular Remodeling: Oxidative damage triggers structural changes in blood vessels, making them narrower and less flexible.
- Enhancing Inflammation: Oxidative stress and inflammation form a vicious cycle, each worsening the other.
Lifestyle Factors Promoting Inflammation
Several aspects of modern living contribute to chronic inflammation and oxidative stress:
- Poor Diet: Processed foods, refined carbohydrates, and unhealthy fats promote inflammation.
- Sedentary Behavior: Regular physical activity has anti-inflammatory effects; lack of movement increases inflammation.
- Environmental Toxins: Pollution, chemicals, and particulate matter increase oxidative stress and inflammation.
- Chronic Stress: Persistent stress triggers inflammatory pathways throughout the body.
The Gut-Inflammation-Hypertension Connection
Emerging research highlights the connection between gut health and blood pressure. The gut microbiome (the community of microorganisms in your digestive tract) influences inflammation throughout the body. Dysbiosis—an unhealthy imbalance in gut bacteria—can increase inflammation and oxidative stress, contributing to hypertension.
Certain gut bacteria help produce short-chain fatty acids that have anti-inflammatory and blood pressure-lowering effects. When these beneficial bacteria decrease, blood pressure regulation can be compromised.
Stress and Sleep Quality: Significant Factors That Can Cause High Blood Pressure
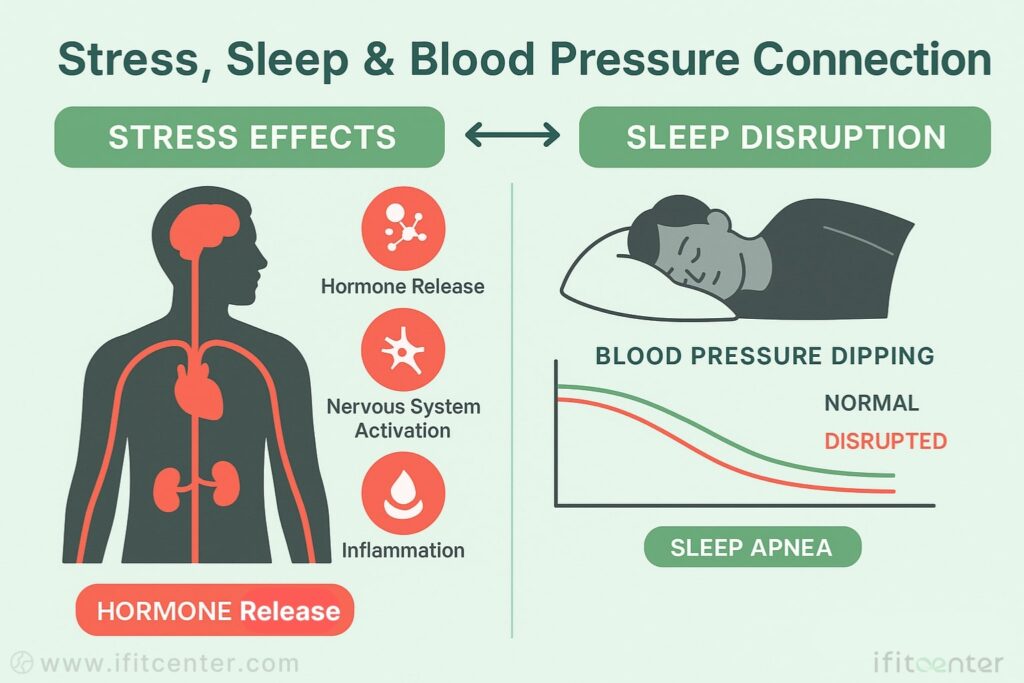
The question “can stress cause high blood pressure” is common among patients, and the answer from research is clear: chronic stress is a significant contributor to hypertension. Similarly, many wonder “can lack of sleep cause high blood pressure,” and studies confirm this connection as well.
The Physiology of Stress and Blood Pressure
When you experience stress, your body activates its “fight-or-flight” response, triggering several changes that directly impact blood pressure:
- Hormone Release: Stress prompts the release of cortisol and adrenaline, both of which raise heart rate and constrict blood vessels.
- Nervous System Activation: The sympathetic nervous system becomes dominant during stress, increasing blood pressure and heart rate.
- Sodium Retention: Chronic stress can alter kidney function, causing increased sodium retention and fluid volume.
- Inflammation: Persistent stress triggers inflammatory pathways that damage blood vessels over time.
While temporary stress-induced blood pressure elevations are normal, chronic stress keeps these mechanisms constantly activated, eventually leading to sustained hypertension.
Sleep Disruption and Hypertension
Quality sleep is essential for proper blood pressure regulation. Poor sleep affects blood pressure through multiple pathways:
- Disrupted Circadian Rhythm: Blood pressure normally decreases during sleep (called “dipping”). Sleep disruption prevents this natural dipping pattern.
- Sympathetic Activation: Sleep deprivation increases sympathetic nervous system activity, raising blood pressure.
- Hormonal Imbalance: Poor sleep alters stress hormone levels and disrupts metabolic regulation.
- Inflammation: Sleep deficit increases inflammation and oxidative stress throughout the body.
Sleep Apnea: A Critical Connection
Sleep apnea—a condition where breathing repeatedly stops and starts during sleep—deserves special attention in any discussion of sleep and blood pressure. When breathing pauses, blood oxygen levels drop, triggering.
Genetic and Environmental Factors: Understanding What Is the Main Cause of High Blood Pressure
When investigating what is the main cause of high blood pressure, genetics emerges as a significant factor that interacts with environmental influences to determine individual risk.
The Genetic Component of Hypertension
Hypertension runs in families, with genetics accounting for approximately 30-50% of blood pressure variability between individuals. This genetic influence operates through several mechanisms:
- Multiple Gene Involvement: Unlike some conditions caused by a single gene, hypertension typically involves numerous genes, each contributing a small effect.
- Sodium Sensitivity: Genetic variations affect how your kidneys process sodium, with some people experiencing greater blood pressure increases from sodium intake than others.
- Renin-Angiotensin System: Genetic differences in this hormone system can predispose some individuals to higher blood pressure.
- Sympathetic Nervous System: Genetic factors influence how reactive your sympathetic nervous system is to various stimuli.
Ethnic and Racial Variations
Hypertension risk and causes vary significantly across different ethnic groups:
- African Heritage: People with African ancestry tend to develop hypertension earlier, experience more severe hypertension, and face higher risks of complications.
- Salt Sensitivity: Different ethnic groups show varying degrees of blood pressure response to sodium intake, with greater sensitivity often observed in those of African and Asian descent.
- Treatment Response: Genetic differences influence how effectively different medications work across ethnic groups, highlighting the importance of personalized treatment approaches.
Gene-Environment Interactions
Perhaps most important is understanding that genes rarely act alone in causing hypertension. Instead, they create susceptibilities that environmental factors can trigger:
- Diet-Gene Interactions: Genetic variations determine how your blood pressure responds to dietary factors like sodium, potassium, and caffeine.
- Stress Response: Your genetic makeup influences how your cardiovascular system reacts to stress.
- Epigenetic Changes: Environmental factors can modify how genes are expressed without changing the underlying DNA sequence, affecting blood pressure regulation.
Environmental Toxins and Blood Pressure
Beyond lifestyle factors, certain environmental exposures can contribute to hypertension:
- Air Pollution: Particulate matter and other pollutants increase oxidative stress and inflammation, damaging blood vessels.
- Heavy Metals: Lead, mercury, and cadmium exposure can contribute to hypertension through vascular damage and kidney effects.
- Endocrine Disruptors: Certain chemicals interfere with hormone systems involved in blood pressure regulation.
- Noise Pollution: Chronic exposure to high noise levels activates stress pathways that can raise blood pressure over time.
Understanding your genetic predisposition doesn’t mean hypertension is inevitable. Even with a strong family history, environmental and lifestyle factors remain powerful influencers of your blood pressure—and these are factors you can control.
Medical Conditions: Common Causes of Secondary Hypertension
While primary hypertension accounts for most cases, identifying the specific causes of secondary hypertension is crucial for effective treatment. Unlike primary hypertension, secondary hypertension has an identifiable underlying cause that, when treated, can sometimes completely resolve high blood pressure.
Kidney Disorders
The kidneys play a central role in blood pressure regulation, making kidney disorders the most common cause of secondary hypertension:
- Chronic Kidney Disease: Damaged kidneys can’t filter fluid and sodium properly, leading to fluid retention and increased pressure. The relationship is bidirectional—kidney disease causes hypertension, and hypertension worsens kidney damage.
- Renal Artery Stenosis: Narrowing of the arteries supplying the kidneys causes reduced blood flow. The kidneys respond by releasing hormones that raise blood pressure, mistakenly “thinking” the body’s overall blood pressure is low.
- Glomerulonephritis: Inflammation of the kidney’s filtering units impairs sodium excretion and activates pressure-raising hormonal systems.
- Polycystic Kidney Disease: This inherited condition causes cysts to develop in the kidneys, leading to hypertension in about 60% of affected individuals before significant kidney function loss occurs.
Hormonal Disorders
Several hormonal conditions can significantly raise blood pressure:
- Primary Aldosteronism: Overproduction of the hormone aldosterone causes the kidneys to retain sodium and water while excreting potassium. It’s present in about 5-10% of hypertensive patients but is often missed.
- Pheochromocytoma: These rare tumors of the adrenal gland release excessive amounts of adrenaline and noradrenaline, causing sudden, dramatic spikes in blood pressure along with sweating, headaches, and rapid heartbeat.
- Cushing’s Syndrome: Excessive cortisol production affects multiple systems that regulate blood pressure, leading to hypertension in about 80% of cases.
- Thyroid Disorders: Both hyperthyroidism and hypothyroidism can cause hypertension through different mechanisms—affecting heart rate, blood vessel elasticity, and blood volume.
Medications and Substances
Various medications and substances can raise blood pressure:
- NSAIDs: Common pain relievers like ibuprofen can cause sodium retention and constrict blood vessels, especially with regular use.
- Oral Contraceptives: Birth control pills, particularly older formulations with higher estrogen levels, can raise blood pressure in some women.
- Decongestants: Over-the-counter cold remedies containing pseudoephedrine constrict blood vessels throughout the body.
- Corticosteroids: Used to treat inflammation, these medications can cause sodium retention and increase blood volume.
- Stimulants: ADHD medications, diet pills, and illicit drugs like cocaine can dramatically increase blood pressure by stimulating the sympathetic nervous system.
- Alcohol: Regular consumption of more than 1-2 drinks daily raises blood pressure through multiple mechanisms.
Structural Cardiovascular Issues
Physical abnormalities in the cardiovascular system can lead to hypertension:
- Coarctation of the Aorta: This congenital narrowing of the body’s main artery forces the heart to pump harder to deliver blood to the lower body. Blood pressure is typically higher in the arms than the legs.
- Obstructive Sleep Apnea: While also contributing to primary hypertension, severe sleep apnea can cause such significant blood pressure elevation that some experts classify it as a cause of secondary hypertension.
- Preeclampsia: This pregnancy complication involves poor placental blood flow, leading to hypertension and protein in the urine. Though temporary, it signals increased future cardiovascular risk.
If you have hypertension that developed suddenly, is severe, or doesn’t respond to standard treatments, discuss the possibility of these secondary causes with your healthcare provider.
Age and Gender Factors: What Causes High Blood Pressure in Young Adults vs. Older People
The causes and characteristics of hypertension vary significantly across age groups. Understanding what causes high blood pressure in young adults versus older individuals can help target prevention and treatment more effectively.
Hypertension in Children and Adolescents
Pediatric hypertension has increased in recent decades, primarily due to:
- Secondary Causes: Unlike adults, children with high blood pressure are more likely to have an identifiable cause, typically kidney disease or congenital heart defects.
- Obesity: The rising prevalence of childhood obesity has led to more cases of primary hypertension in younger populations.
- Premature Birth: Being born preterm, especially before 32 weeks, increases the risk of developing hypertension in childhood and adolescence.
What Causes High Blood Pressure in Young Adults
For those between 18-40 years, several factors contribute to early-onset hypertension:
- Insulin Resistance: Often present before diabetes develops, insulin resistance affects blood pressure regulation and is increasingly common in younger adults.
- Genetic Factors: Young people with hypertension frequently have a strong family history, suggesting inherited susceptibility.
- Lifestyle Choices: Poor diet, sedentary behavior, chronic stress, and insufficient sleep affect younger generations significantly.
- Kidney Issues: Young adults with high blood pressure should be evaluated for kidney disorders, which can manifest with hypertension as an early sign.
Middle-Age Onset Hypertension
In people 40-60 years old, the causes typically shift toward:
- Metabolic Changes: The cumulative effects of poor metabolic health, including insulin resistance and visceral fat accumulation, become more prominent.
- Hormonal Shifts: Menopause in women leads to estrogen decline, which affects blood vessel function and blood pressure regulation.
- Chronic Stress Effects: The cumulative impact of career, family, and financial stressors often peaks during these years.
- Early Vascular Aging: Blood vessels begin to stiffen, increasing systolic pressure in particular.
Elderly Hypertension
In those over 65, hypertension often has unique characteristics:
- Arterial Stiffening: The loss of elasticity in major arteries leads to isolated systolic hypertension (high systolic with normal diastolic pressure).
- Endothelial Dysfunction: Age-related impairment of the blood vessel lining affects blood pressure regulation.
- Medication Effects: Older adults often take multiple medications that may affect blood pressure.
- Baroreceptor Dysfunction: Age-related changes in pressure sensors can lead to greater blood pressure variability.
Gender Differences in Hypertension
Men and women develop hypertension through somewhat different pathways:
- Premenopausal Women: Generally have lower rates of hypertension than age-matched men, partly due to estrogen’s protective effects on blood vessels.
- Postmenopausal Women: Experience a sharp increase in hypertension risk, sometimes surpassing men of the same age.
- Sex Hormones: Testosterone and estrogen affect kidney function, blood vessel reactivity, and sympathetic nervous system activity differently.
- Pregnancy: Approximately 10% of pregnancies are affected by gestational hypertension or preeclampsia, which can indicate future cardiovascular risk.
Understanding these age and gender differences helps explain why hypertension can manifest differently across the lifespan and why treatment approaches often need to be tailored to the individual’s specific circumstances.
Identifying Your Personal Triggers: What Can Cause High Blood Pressure in Your Case
After exploring the many factors that can cause high blood pressure, the crucial question becomes: what can cause high blood pressure in your specific case? Hypertension is rarely the result of just one factor, and the combination of causes varies greatly from person to person.
The Individualized Nature of Hypertension
Blood pressure regulation involves multiple body systems, making each person’s hypertension somewhat unique. Consider these patterns:
- Salt Sensitivity: While some people experience significant blood pressure increases with sodium consumption, others show minimal response, largely due to genetic differences.
- Stress Response: The degree to which stress affects blood pressure varies dramatically between individuals.
- Medication Effects: The same medication can lower blood pressure significantly in one person while having minimal effect in another.
- Weight Impact: Some people see dramatic blood pressure reductions with modest weight loss, while others experience smaller changes.
Identifying Your Primary Hypertension Drivers
To determine which factors most affect your blood pressure, consider the following approach:
- Track Your Readings: Monitor your blood pressure regularly, noting date, time, and circumstances (after meals, during stress, etc.).
- Experiment With One Factor: Modify one potential trigger at a time (reduce sodium, improve sleep, etc.) and track the results for 2-4 weeks.
- Notice Patterns: Identify which lifestyle changes produce the most significant improvements in your readings.
- Consider Testing: Based on your response patterns, discuss relevant testing with your healthcare provider (insulin resistance assessment, sleep study, etc.).
Common Hypertension Trigger Combinations
Research suggests certain hypertension causes frequently cluster together:
- Metabolic Pattern: Insulin resistance + abdominal obesity + sleep issues + stress
- Inflammatory Pattern: Chronic inflammation + gut health issues + dietary sensitivities + oxidative stress
- Stress-Sleep Pattern: Chronic stress + poor sleep quality + sympathetic overdrive + inadequate recovery
- Environmental Pattern: Chemical exposures + medication effects + nutritional deficiencies + inadequate physical activity
The Value of Comprehensive Assessment
While self-monitoring provides valuable insights, a comprehensive assessment can identify less obvious causes:
- Blood Biomarkers: Beyond standard lipid panels, advanced testing can reveal inflammation, insulin resistance, and hormonal imbalances affecting blood pressure.
- Body Composition Analysis: Understanding visceral fat levels and muscle mass provides context for metabolic health.
- Functional Assessments: Evaluating stress response, autonomic function, and vascular reactivity can reveal underlying mechanisms.
- Environmental Exposure History: Reviewing potential toxin exposures, medication effects, and other environmental factors can uncover hidden triggers.
Understanding the Multiple Causes of High Blood Pressure: Your Path Forward
As we’ve explored throughout this guide, the causes of high blood pressure extend far beyond simply consuming too much salt. Hypertension emerges from a complex interplay of metabolic, genetic, environmental, and lifestyle factors that affect each person differently.
The key insights from our exploration include:
- Insulin resistance
- Body composition
- Dietary factors
- Chronic inflammation and oxidative stress
- Stress and poor sleep
- Genetic and environmental factors
- Age and gender
- Secondary causes must be considered, especially in cases of sudden onset or treatment-resistant hypertension.
Understanding these diverse causes empowers you to take a more targeted approach to managing your blood pressure. Rather than applying generic recommendations, identifying your personal hypertension triggers allows for precision interventions that address the root causes of your specific case.
This comprehensive approach often leads to more effective blood pressure management, sometimes with reduced need for medication. More importantly, addressing these underlying factors improves overall cardiovascular health and reduces risk beyond what blood pressure numbers alone indicate.
To access other content on the IFitCenter’s blog, you can use the following links:
References
- Cai, Q., Zhao, X., Dong, L., Zhang, X., Wang, C., Wang, S., Zhou, Y., Zhou, X., Li, Y., Wang, S., Liu, L., & Hu, A. (2023). Keeping obesity status is a risk factor of hypertension onset: evidence from a community-based longitudinal cohort study in North China. Frontiers in Public Health, 11, 1170334. DOI: 10.3389/fpubh.2023.1170334
- Wang, B., Yang, Y., & Li, X. (2022). Interaction of Hypertension and Insulin Resistance Exacerbates the Occurrence of Diabetes Mellitus in Healthy Individuals. Journal of Diabetes Research, 2022, 9289812. DOI: 10.1155/2022/9289812
- El Meouchy, P., Wahoud, M., Allam, S., Chedid, R., Karam, W., & Karam, S. (2022). Hypertension Related to Obesity: Pathogenesis, Characteristics and Factors for Control. International Journal of Molecular Sciences, 23(20), 12305. DOI: 10.3390/ijms232012305
- Makarem, N., Alcántara, C., Williams, N., Bello, N. A., & Abdalla, M. (2021). Effect of Sleep Disturbances on Blood Pressure. Hypertension, 77(4). DOI: 10.1161/HYPERTENSIONAHA.120.14479
- Marwaha, K. (2022). Examining the Role of Psychosocial Stressors in Hypertension. Journal of Preventive Medicine and Public Health, 55(6), 499-505. DOI: 10.3961/jpmph.21.266



