Every five seconds, someone in the world develops diabetes. By 2045, an estimated 783 million adults will be living with this condition—a staggering 10.5% increase from today’s already concerning numbers. Behind each of these statistics lies a fundamental question: what exactly causes diabetes to develop in the human body?
Recent scientific research has revealed that the causes of elevated blood sugar are far more nuanced than previously thought. According to a 2023 systematic review published in Communications Medicine, diabetes—particularly Type 2—can be subclassified into distinct subtypes with different causal pathways, challenging the one-size-fits-all understanding of what causes high glucose levels.
For Type 1 diabetes, groundbreaking immunological research has identified specific viral triggers and genetic markers that contribute to the autoimmune destruction of insulin-producing cells. These discoveries are transforming our understanding of the causes of Type 1 diabetes and opening new avenues for prevention.
At IFitCenter, we’re exploring this fascinating and complex topic in its entirety. This comprehensive guide brings together cutting-edge research on the biological, genetic, and environmental factors that cause blood sugar to rise, providing you with a deeper understanding of how diabetes truly develops.
Understanding Blood Sugar Regulation
To truly understand what causes diabetes, we first need to explore how your body normally manages blood sugar. Think of blood sugar regulation as a sophisticated thermostat system in your home—constantly monitoring and adjusting to maintain the perfect temperature. In your body, this “temperature” is your blood glucose level.
Normal Glucose Metabolism: Your Body’s Energy System
Every cell in your body needs glucose (sugar) for energy—similar to how your car needs fuel to run. When you eat carbohydrates, whether from an apple, a slice of bread, or a sugary dessert, your digestive system breaks them down into glucose molecules that enter your bloodstream.
Unlike your car, which can hold extra fuel in its tank, your body wants to keep blood glucose within a very narrow range—typically 70-100 mg/dL when fasting. This amount is surprisingly small—approximately one teaspoon of sugar dissolved in your entire bloodstream (about 1.5 gallons of blood).
When blood glucose rises after a meal, your pancreas—a leaf-shaped organ nestled behind your stomach—detects this increase and responds by releasing insulin from specialized cells called beta cells. This critical hormone then circulates throughout your body, acting as a “key” that unlocks cell membranes so glucose can enter.
How Insulin Works: The Master Key for Glucose
Insulin performs several essential functions to manage your blood sugar:
- Cellular uptake: Insulin attaches to receptors on cell surfaces (particularly muscle and fat cells), triggering glucose transporters to move to the cell membrane and allow glucose inside—like opening doors to let visitors in.
- Glycogen storage: Excess glucose gets converted to glycogen (a storage form of glucose) in the liver and muscles—similar to filling up your pantry with extra food for later use.
- Fat storage: When glycogen stores are full, additional glucose gets converted to fat—like putting overflow items in long-term storage.
- Suppressing glucose production: Insulin tells the liver to stop producing and releasing additional glucose—like turning off the faucet when the bathtub is full.
Your body also produces other hormones that work in concert with insulin. Glucagon—insulin’s counterpart—is released when blood sugar drops too low, instructing the liver to convert stored glycogen back into glucose and release it into the bloodstream. This balanced system ensures your blood sugar stays within the optimal range, whether you’ve just eaten a meal or haven’t eaten for hours.
When the System Malfunctions
Diabetes develops when this finely tuned blood sugar regulation system breaks down. This can happen in two primary ways:
Insufficient insulin production: In this scenario, the pancreas cannot produce enough insulin to manage blood glucose levels. This is like having a thermostat that can’t send enough signals to your heating system—the temperature (or in this case, blood sugar) rises uncontrollably.
Insulin resistance: Here, the body produces insulin, but cells don’t respond properly to its signals. Imagine having a thermostat that works correctly, but the heating system ignores its commands—again resulting in improper regulation.
Over time, both scenarios lead to chronically elevated blood glucose levels—the hallmark of diabetes. This excess glucose circulating in the bloodstream can damage blood vessels and nerves throughout the body, leading to the various complications associated with diabetes.
The Fundamental Difference Between Type 1 and Type 2 Diabetes
While both Type 1 and Type 2 diabetes result in high blood sugar, their underlying causes are dramatically different:
| Type 1 Diabetes | Type 2 Diabetes |
|---|---|
| The body’s immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. | The body produces insulin, but cells become resistant to its effects, and eventually, insulin production may decline. |
| Causes an absolute insulin deficiency. | Causes relative insulin insufficiency due to resistance and eventual production decline. |
| Typically appears suddenly, often in childhood or adolescence. | Develops gradually over years, typically in adults (though increasingly in younger people). |
| Not preventable with current knowledge. | Often preventable through lifestyle modifications. |
| Always requires insulin therapy. | May be managed with lifestyle changes, oral medications, and sometimes insulin. |
Think of Type 1 diabetes as a factory shutdown—the insulin production facility (beta cells) has been destroyed. In contrast, Type 2 diabetes begins as a distribution problem—the factory produces insulin, but the recipients (cells) aren’t accepting the deliveries properly. Eventually, the factory may also begin to fail as it struggles to meet the increased demand.
Understanding these fundamental differences explains why the causes, progression, and management approaches differ significantly between the two types. It also highlights why personalized approaches to diabetes prevention and management are essential—the underlying mechanisms are distinct, even though the end result (high blood glucose) appears similar.
What Causes Type 1 Diabetes?
Unlike Type 2 diabetes, which develops gradually over time, Type 1 diabetes often appears suddenly. But what actually causes this autoimmune form of diabetes? Let’s explore the key factors behind Type 1 diabetes development.
On the IFitCenter blog, we have provided a comprehensive guide for diabetes, completely free of charge and based on the latest research. By viewing these articles, in addition to increasing your general knowledge in this field, you can easily manage this disease in a principled manner. To access the first part of the articles, simply use the links below:
- What is Diabetes?
- Symptoms and Signs of Diabetes
- Types of Diabetes
- What Are the Complications of Diabetes?
- Diabetes Diagnosis Method
- Worst fruits for diabetes
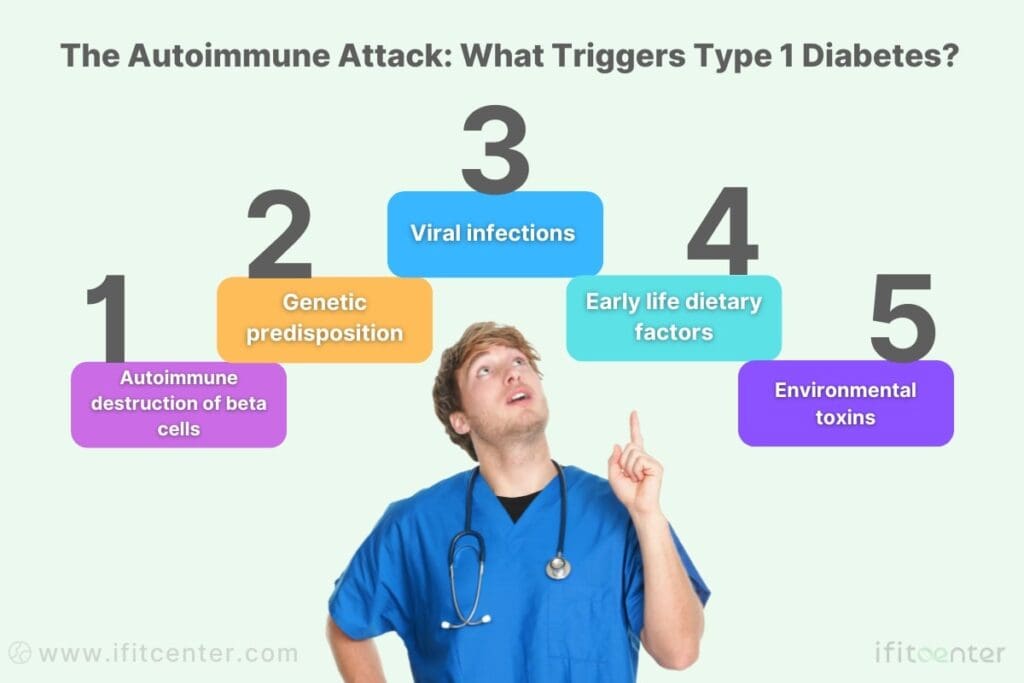
The Autoimmune Attack on Beta Cells
At its core, Type 1 diabetes is an autoimmune condition where the body’s defense system mistakenly identifies insulin-producing beta cells as foreign invaders. This case of “mistaken identity” leads to the immune system attacking and destroying these essential cells in the pancreas.
Think of it as your body’s security system malfunctioning—rather than protecting your pancreas, it attacks the very cells needed to regulate blood sugar. Once a significant portion of beta cells are destroyed, the pancreas can no longer produce sufficient insulin, resulting in Type 1 diabetes.
Genetic Factors That Increase Type 1 Diabetes Risk
Your genetic makeup plays a significant role in determining whether you might develop Type 1 diabetes. Certain gene variants, particularly those related to the immune system, can increase susceptibility to this condition.
The strongest genetic association involves the human leukocyte antigen (HLA) system—specifically, the HLA-DR3 and HLA-DR4 genes. These genes help regulate immune responses, and certain variants can make the immune system more likely to attack beta cells.
While having these gene variants increases risk, it doesn’t guarantee disease development. Many people with these genetic markers never develop Type 1 diabetes, indicating that additional factors must trigger the disease process.
Family History and Inheritance Patterns
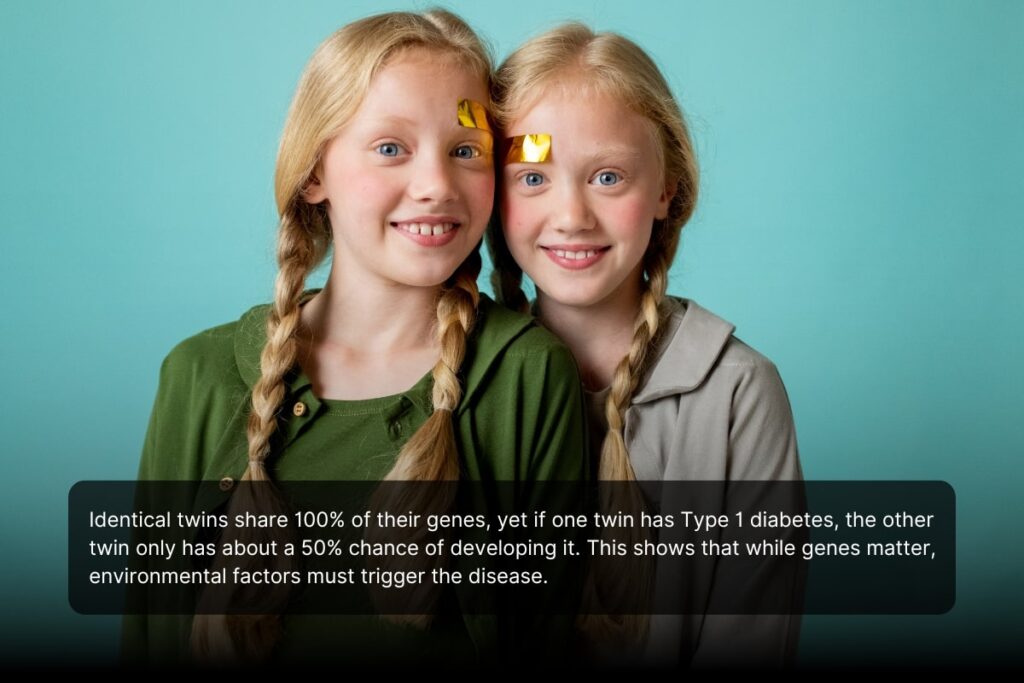
Having a family member with Type 1 diabetes increases your risk, though not as dramatically as you might expect:
- If a parent has Type 1 diabetes, their child has approximately a 5-10% chance of developing it
- If a sibling has Type 1 diabetes, the risk is similar at 5-10%
- If an identical twin has Type 1 diabetes, the other twin has about a 50% chance of developing it
The fact that identical twins don’t always both develop Type 1 diabetes (despite sharing identical genes) provides strong evidence that environmental factors must also play a crucial role in triggering the disease.
Environmental Triggers of Type 1 Diabetes
Research suggests several environmental factors may trigger Type 1 diabetes in genetically susceptible individuals:
Viral Infections as Diabetes Triggers
Certain viruses, particularly enteroviruses, have been linked to Type 1 diabetes development. These viral infections may either:
- Directly damage beta cells
- Create inflammation that harms beta cells
- Cause the immune system to mistakenly attack beta cells due to similarities between viral proteins and proteins on beta cells (called molecular mimicry)
Coxsackievirus B, a type of enterovirus, has shown the strongest association with Type 1 diabetes onset. Some research suggests that enterovirus infections during pregnancy or early childhood may increase risk.
To access the second part of the articles related to diabetes, you can use the following links:
- Is Diabetes Curable?
- Type 2 Diabetes Explained
- Type 1 Diabetes Explained
- Relationship Between Diabetes and Obesity
- The Real Difference Between Prediabetes and Diabetes
- can diabetics drink alcohol?
Early Dietary Factors
Some research suggests that early nutrition choices might influence Type 1 diabetes risk:
- Early introduction of cow’s milk proteins (before 3-4 months of age)
- Early exposure to gluten or cereal proteins
- Vitamin D deficiency in early life
- Breastfeeding duration (with longer periods potentially offering some protection)
However, it’s important to note that the evidence for dietary influences remains inconsistent, and no single food has been definitively proven to cause or prevent Type 1 diabetes.
Environmental Toxins
Some environmental chemicals and toxins have been suggested as potential contributors to Type 1 diabetes risk:
- Nitrates in drinking water
- Certain pesticides and air pollutants
- Some food additives and preservatives
The evidence for toxin-related causes remains preliminary, and more research is needed to establish definitive connections.
The Process of Beta Cell Destruction
The development of Type 1 diabetes follows a progressive pattern:
- Genetic predisposition: Individuals inherit genes that make them susceptible.
- Environmental trigger: An environmental factor (like a viral infection) initiates the process.
- Autoimmunity begins: The immune system starts producing antibodies against beta cells.
- Silent phase: Beta cells are gradually destroyed over months or years without symptoms.
- Diminished insulin reserve: When approximately 80-90% of beta cells are destroyed, insulin production becomes insufficient.
- Clinical onset: Blood glucose levels rise significantly, and symptoms of diabetes appear.
This process explains why Type 1 diabetes often appears suddenly despite developing silently over a longer period.
“Many patients are surprised to learn that Type 1 diabetes develops long before symptoms appear. The immune system can be attacking beta cells for months or even years while the pancreas compensates by working harder. By the time glucose levels rise and symptoms develop, approximately 80-90% of insulin-producing cells have already been destroyed. This silent progression is why we’re exploring immune markers for earlier detection in high-risk individuals.”
Dr. Babak Jamalian, Family Physician.
Debunking Common Myths About Type 1 Diabetes Causes
Several misconceptions about what causes Type 1 diabetes persist:
| Myth | Fact |
|---|---|
| Type 1 diabetes is caused by eating too much sugar | Type 1 diabetes is an autoimmune condition and is not caused by diet or sugar consumption |
| Type 1 diabetes only affects children | While often diagnosed in childhood, Type 1 diabetes can develop at any age |
| Type 1 diabetes is caused by obesity | Unlike Type 2 diabetes, Type 1 has no connection to weight or obesity |
| Stress causes Type 1 diabetes | While stress may affect blood glucose levels, it does not cause Type 1 diabetes |
| Type 1 diabetes can be prevented or reversed with lifestyle changes | Currently, there is no known way to prevent or reverse Type 1 diabetes |
Understanding the true causes of Type 1 diabetes—a complex interplay of genetic susceptibility and environmental triggers—helps clarify why this condition develops and dispels harmful misconceptions that often lead to stigma or blame.
What Causes Type 2 Diabetes?
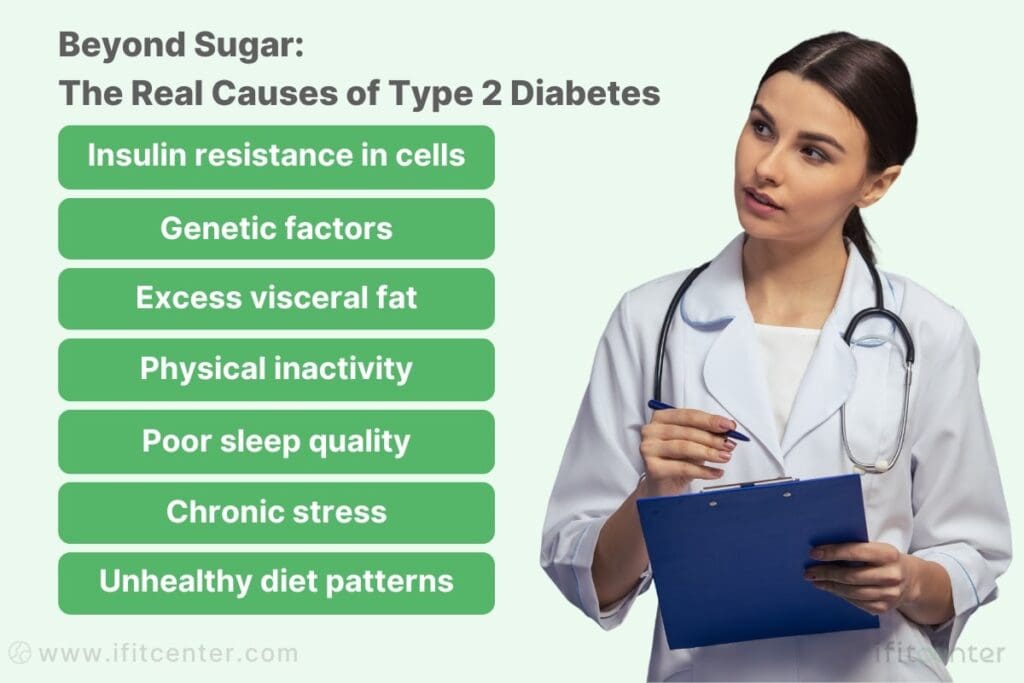
Type 2 diabetes, which accounts for over 90% of all diabetes cases worldwide, develops through a different pathway than Type 1. Understanding what causes high blood sugar in Type 2 diabetes requires examining several interconnected factors that contribute to this increasingly common condition.
Insulin Resistance: The Root Cause of Type 2 Diabetes
At the heart of Type 2 diabetes lies insulin resistance—a condition where your cells don’t respond properly to insulin signals. Think of insulin as a key that unlocks cells to allow glucose entry. With insulin resistance, the locks on your cells change, making the keys (insulin) less effective.
When cells resist insulin’s effects, glucose remains in the bloodstream instead of entering cells. In response, your pancreas produces more insulin to overcome this resistance—like making more keys when the locks become difficult. This compensatory mechanism can work for years, keeping blood glucose levels near normal despite increasing insulin resistance.
Eventually, however, the pancreas cannot keep up with the increased demand. The insulin-producing beta cells become exhausted and begin to fail, leading to rising blood glucose levels and the development of Type 2 diabetes.
How Insulin Resistance Develops Over Time
Insulin resistance doesn’t appear overnight—it develops gradually over years through several mechanisms:
- Fat accumulation: Excess fat, particularly in the liver and around abdominal organs (visceral fat), releases inflammatory compounds that interfere with insulin signaling
- Mitochondrial dysfunction: The energy-producing components of cells become less efficient, affecting glucose metabolism
- Chronic inflammation: Low-grade, persistent inflammation disrupts normal cell function and insulin response
- Lipid overflow: When fat cells become overloaded, fatty acids spill into the bloodstream and accumulate in muscles and the liver, impairing insulin action
This progression explains why Type 2 diabetes typically develops over decades rather than suddenly appearing like Type 1 diabetes.
Genetic Factors That Increase Type 2 Diabetes Risk
Your genetic makeup significantly influences your susceptibility to Type 2 diabetes. Unlike Type 1 diabetes, which involves a few specific genes, Type 2 diabetes has been linked to numerous gene variants, each contributing a small amount to overall risk.
Some of these genes affect:
- Beta cell function and insulin production
- Insulin receptor sensitivity
- Glucose transport and metabolism
- Fat distribution patterns
- Appetite regulation
Having a family history of Type 2 diabetes significantly increases your risk. If one parent has Type 2 diabetes, your risk increases by 40%. If both parents have the condition, your risk can be as high as 70%.
Ethnic Variations in Type 2 Diabetes Risk
Type 2 diabetes risk varies significantly across ethnic groups, with some populations showing much higher susceptibility:
- Pacific Islanders, Native Americans, and Hispanic populations have higher rates than white populations
- South Asians develop Type 2 diabetes at younger ages and lower body weights than Europeans
- African Americans have increased risk compared to white Americans
These variations reflect both genetic differences and cultural/lifestyle factors that influence diet, physical activity, and body composition.
Lifestyle Factors That Cause High Blood Sugar
While genetics loads the gun, lifestyle factors often pull the trigger in Type 2 diabetes development:
Diet Composition and Insulin Sensitivity
What you eat significantly impacts your Type 2 diabetes risk through several mechanisms:
- Refined carbohydrates and added sugars: These cause rapid blood glucose spikes, placing stress on insulin-producing cells
- Excessive calories: Regardless of source, overconsumption leads to weight gain and increased insulin resistance
- Processed foods: Often high in unhealthy fats, refined carbs, and low in fiber—a combination that promotes insulin resistance
- Low fiber intake: Fiber slows glucose absorption and supports a healthy gut microbiome
Contrary to popular belief, Type 2 diabetes is not simply caused by eating too much sugar—it’s the overall dietary pattern and caloric balance that matter most.
“One of the most significant misconceptions I encounter is that Type 2 diabetes is simply caused by consuming too much sugar. While diet certainly plays a role, the underlying mechanisms are far more complex. Insulin resistance often begins in the liver and muscle tissue due to metabolic dysfunction at the cellular level. This explains why seemingly minor improvements in physical activity can have profound effects on insulin sensitivity, even before significant weight loss occurs.”
Dr. Babak Jamalian, Family Physician.
Physical Inactivity and Metabolic Effects
Regular physical activity is crucial for maintaining insulin sensitivity. When you’re inactive:
- Muscles use less glucose, leaving more in the bloodstream
- Insulin receptors become less responsive
- Fat accumulates in and around organs
- Mitochondria (cellular energy producers) become less efficient
Even modest increases in activity can improve insulin sensitivity. Research shows that walking briskly for 30 minutes daily can reduce Type 2 diabetes risk by approximately 30%.
Sleep Deprivation’s Impact on Blood Sugar
Poor sleep is an often overlooked cause of elevated blood sugar. When you don’t get enough quality sleep:
- Insulin sensitivity decreases (even one night of poor sleep can reduce insulin sensitivity by 25%)
- Stress hormones increase, raising blood glucose levels
- Appetite-regulating hormones are disrupted, leading to increased hunger and cravings
- The body’s circadian rhythm is disrupted, affecting glucose metabolism
Studies show that people who regularly sleep less than 6 hours per night have significantly higher rates of insulin resistance and Type 2 diabetes.
Understanding these multiple causes of Type 2 diabetes explains why prevention and management approaches need to address various aspects of lifestyle and health, from nutrition and physical activity to sleep quality and stress management.
Manage Your Weight, Master Your Blood Sugar
Lifestyle factors like excess weight and physical inactivity can significantly elevate your risk of developing Type 2 diabetes. But the good news is: these are factors you can control. At iFitCenter, we offer personalized, medically supervised weight-loss and lifestyle programs specifically designed to improve insulin sensitivity, stabilize blood sugar, and reduce your diabetes risk.
Our comprehensive metabolic assessments and tailored nutritional plans are designed to address your unique health profile, helping you regain control of your weight—and your blood glucose levels—for the long term.
Take action today and start your personalized journey toward better metabolic health.
Comparing Type 1 and Type 2 Diabetes Causes: What is the Reason for Diabetes?
While both Type 1 and Type 2 diabetes result in elevated blood glucose levels, they stem from fundamentally different causes. Understanding these differences is crucial for proper prevention, diagnosis, and management approaches.
Key Differences Between Type One Diabetes Causes and Type 2 Diabetes Causes
| Factor | Type 1 Diabetes Causes | Type 2 Diabetes Causes |
|---|---|---|
| Primary Mechanism | Autoimmune destruction of beta cells | Insulin resistance followed by relative insulin deficiency |
| Insulin Production | Severe lack or complete absence of insulin | Initially increased insulin production, which declines over time |
| Genetic Component | Primarily HLA genes (DR3/DR4); fewer genes with stronger influence | Multiple genes with small individual effects; stronger overall heritability |
| Family Risk | 5-10% risk if parent or sibling has it; 50% for identical twins | 40% risk with one parent; up to 70% with both parents |
| Environmental Triggers | Viral infections (especially enteroviruses), early dietary exposures | Excess caloric intake, sedentary lifestyle, poor sleep, chronic stress |
| Age of Onset | Usually childhood or adolescence, but can occur at any age | Typically adulthood, but increasingly appearing in younger populations |
| Speed of Development | Often appears suddenly after years of silent autoimmune activity | Develops gradually over many years with insulin resistance preceding diagnosis |
| Obesity Relation | No causal relationship with obesity | Strong causal relationship, though can develop in non-obese individuals |
| Reversibility | Currently not reversible | Often reversible in early stages through lifestyle changes and weight loss |
| Prevention | No proven prevention strategies yet | Largely preventable through lifestyle modifications |
Similarities in Diabetes Causes
Despite their differences, Type 1 and Type 2 diabetes share some common elements in their causal pathways:
- Genetic predisposition: Both types have genetic components, though the specific genes and inheritance patterns differ
- Environmental influence: External factors play crucial roles in triggering both diabetes types
- Beta cell stress: Both types eventually involve beta cell dysfunction, though through different mechanisms
- Inflammation: Inflammatory processes contribute to both types, though in different ways
Why Understanding Causes Matters for Prevention and Management
Knowing what causes high blood sugar in each diabetes type has profound implications:
For Type 1 Diabetes:
- Understanding the autoimmune nature explains why immunosuppressive therapies are being researched
- Knowing beta cells are destroyed explains the absolute requirement for insulin therapy
- Recognizing genetic markers helps identify high-risk individuals for clinical trials
- Research into environmental triggers may eventually lead to prevention strategies
For Type 2 Diabetes:
- Understanding insulin resistance guides effective lifestyle interventions
- Recognizing the progressive nature emphasizes the importance of early intervention
- Knowing the reversible nature in early stages provides hope and motivation
- Understanding ethnic variations helps target screening and prevention efforts
The distinction between what causes Type 1 and Type 2 diabetes is not merely academic—it fundamentally shapes treatment approaches. Type 1 requires insulin replacement therapy due to the absence of insulin production. Type 2 initially focuses on reducing insulin resistance through lifestyle changes and medications that improve insulin sensitivity or enhance the body’s insulin response.
Moreover, understanding these distinct causes helps combat the stigma that often surrounds diabetes. Type 1 is not caused by lifestyle choices, and while lifestyle factors strongly influence Type 2 risk, genetic predisposition plays a significant role that is beyond individual control.
By understanding what causes blood sugar to rise in each type of diabetes, patients, healthcare providers, and researchers can work together more effectively to manage existing cases and potentially prevent new ones.
Understanding What Really Causes Diabetes: Moving Forward
Throughout this article, we’ve explored the complex web of factors that cause diabetes. Rather than a single culprit, we’ve seen that both Type 1 and Type 2 diabetes develop through multiple interlinking pathways.
Key Insights About Diabetes Causes
- Type 1 diabetes stems from an autoimmune attack on pancreatic beta cells, triggered by a combination of genetic susceptibility and environmental factors
- Type 2 diabetes develops primarily through insulin resistance, influenced by genetics, lifestyle choices, and metabolic factors
- Both diabetes types involve a complex interplay between what we can’t control (genetics) and what we can (many environmental and lifestyle factors)
- Understanding these causes helps dispel harmful myths and stigma surrounding diabetes
The causes of high blood sugar differ significantly between diabetes types, which explains why prevention and management approaches must be tailored accordingly. What works for preventing Type 2 diabetes may have little relevance for Type 1, and understanding this distinction is crucial.
Why Personal Risk Assessment Matters
Each person’s risk profile for diabetes is unique, based on their specific combination of:
- Genetic background
- Family history
- Ethnicity
- Body composition
- Lifestyle patterns
- Environmental exposures
This individual variation means that understanding your personal risk factors is essential for effective prevention. What causes high glucose levels in one person might have less impact on another due to genetic differences and other protective factors.
Prevention: Focus on What You Can Control
While we can’t change our genetic makeup, research clearly shows that many diabetes risk factors are modifiable:
- Maintain a healthy body weight through balanced nutrition
- Stay physically active, even with moderate activities like regular walking
- Prioritize quality sleep (7-8 hours for most adults)
- Manage stress through various relaxation techniques
- Be aware of early warning signs and risk factors
For Type 2 diabetes particularly, these lifestyle approaches can dramatically reduce risk and even reverse early stage disease progression in many cases.
To access other content on the IFitCenter’s blog, you can use the following links:
References for Causes of Diabetes
- Madurapperumage Anuradha Erandathi, William Yu Chung Wang, Michael Mayo, Ching-Chi Lee. Comprehensive Factors for Predicting the Complications of Diabetes Mellitus: A Systematic Review. Curr Diabetes Rev. 2024;20(9):e040124225240. DOI: 10.2174/0115733998271863231116062601
- Matti Uusitupa, Tauseef A Khan, Effie Viguiliouk, Hana Kahleova, Angela A Rivellese, Kjeld Hermansen, Andreas Pfeiffer, Anastasia Thanopoulou, Jordi Salas-Salvadó, Ursula Schwab, John L Sievenpiper. Prevention of Type 2 Diabetes by Lifestyle Changes: A Systematic Review and Meta-Analysis. Nutrients. 2019;11(11):2611. DOI: 10.3390/nu11112611
- Karla Ivette Galaviz, Mary Beth Weber, Audrey Straus, Jeehea Sonya Haw, KM Venkat Narayan, Mohammed Kumail Ali. Global Diabetes Prevention Interventions: A Systematic Review and Network Meta-analysis of the Real-World Impact on Incidence, Weight, and Glucose. Diabetes Care. 2018;41(7):1526–1534. DOI: 10.2337/dc17-2222
- Lu, X., Xie, Q., Pan, X. et al. Type 2 diabetes mellitus in adults: pathogenesis, prevention and therapy. Sig Transduct Target Ther 9, 262 (2024).
DOI: 10.1038/s41392-024-01951-9 - Ismail, L., Materwala, H., & Al Kaabi, J. (2021). Association of risk factors with type 2 diabetes: A systematic review. Computational and Structural Biotechnology Journal, 19, 1759-1785.
DOI: 10.1016/j.csbj.2021.03.003 - Ali, S., Hussain, R., Malik, R. A., Amin, R., & Tariq, M. N. (2024). Association of Obesity With Type 2 Diabetes Mellitus: A Hospital-Based Unmatched Case-Control Study. Cureus, 16(1), e52728. DOI: 10.7759/cureus.52728
- Harding, J. L., Wander, P. L., Zhang, X., Li, X., Karuranga, S., Chen, H., Sun, H., Xie, Y., Oram, R. A., Magliano, D. J., Zhou, Z., Jenkins, A. J., & Ma, R. C. W. (2022). The incidence of adult-onset type 1 diabetes: A systematic review from 32 countries and regions. Diabetes Care, 45(4), 994–1006.
DOI: 10.2337/dc21-1752 - Mobasseri, M., Shirmohammadi, M., Amiri, T., Vahed, N., Hosseini Fard, H., & Ghojazadeh, M. (2020). Prevalence and incidence of type 1 diabetes in the world: A systematic review and meta-analysis. Health Promotion Perspectives, 10(2), 98–115.
DOI: 10.34172/hpp.2020.18



