“Can I ever stop taking diabetes medications?” “Will I need insulin eventually?” “Is there anything I can do to reverse my diabetes?” If you’re living with type 2 diabetes, these questions might keep you up at night. The good news? Medical science now has encouraging answers.
Imagine your body’s insulin system like a key card entry system. In type 2 diabetes, the key cards (insulin) stop working properly, and glucose can’t enter your cells. But recent research shows that losing weight can effectively “reset” this system. The DiRECT trial demonstrated that weight loss of 15kg or more led to diabetes remission in 86% of participants – meaning normal blood sugar levels without medication.
At IFitCenter, we believe in empowering you with evidence-based solutions. This comprehensive guide will explain how weight loss can improve – and potentially reverse – type 2 diabetes, based on the latest medical research and clinical evidence.
Understanding the Weight-Diabetes Connection
Why does excess weight often lead to type 2 diabetes? The answer lies in a chain reaction that occurs in your body when you carry extra pounds, particularly around your midsection. Let’s break down this connection step by step.
How Extra Weight Disrupts Blood Sugar Control
Think of your body’s blood sugar control like a perfectly synchronized delivery system. When you eat, your food is broken down into glucose (sugar), which needs to be delivered to your cells for energy. In a healthy body, this process works smoothly: glucose enters your bloodstream, and a hormone called insulin helps transport it into your cells.
However, excess body weight, especially around your abdomen, disrupts this system. It’s like adding obstacles to the delivery route – making it increasingly difficult for insulin to do its job effectively.
The Weight-Blood Sugar Cycle
Here’s what happens when you carry extra weight:
- Your fat cells release substances that interfere with blood sugar control
- This interference makes it harder for insulin to move glucose into your cells
- Your body produces more insulin to compensate
- Over time, your cells become less responsive to insulin
- Blood sugar levels begin to rise
Breaking the Cycle Through Weight Loss
The encouraging news is that losing weight can reverse this process. When you lose significant weight, especially from around your abdomen, several positive changes occur:
- Your body becomes more sensitive to insulin again
- Blood sugar levels start to normalize
- Your body needs less insulin to maintain healthy blood sugar
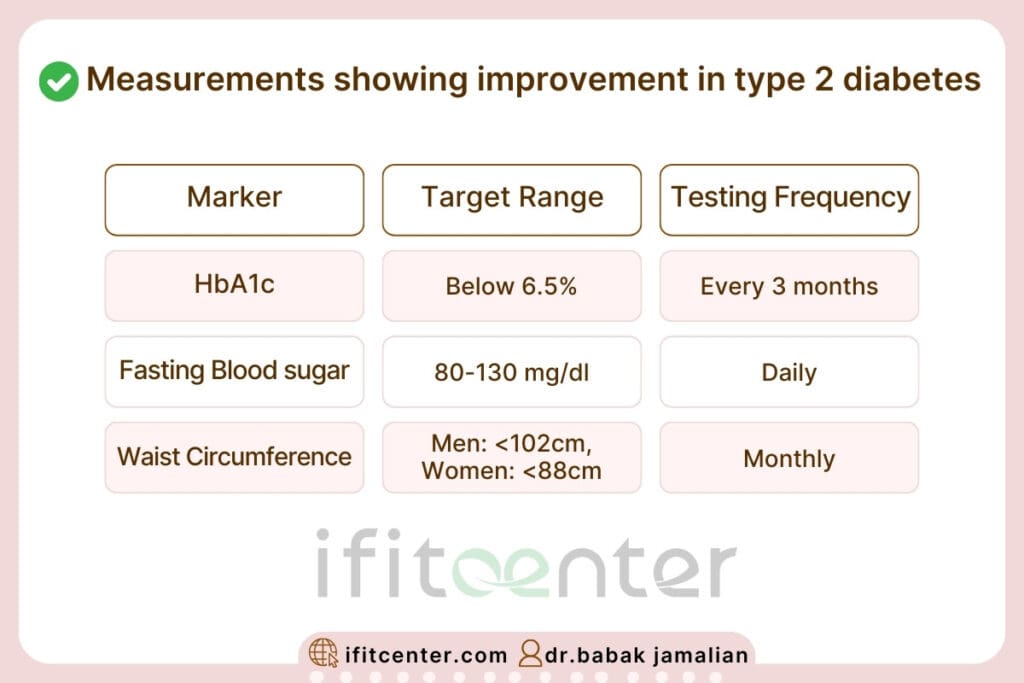
Measuring Progress: Key Health Markers
Doctors track several important markers to understand how weight affects your diabetes:
- Blood Sugar Levels: Both immediate (finger prick) and long-term (HbA1c) measurements show how well your body manages glucose
- Body Composition: Not just weight, but where you carry fat matters
- Medication Needs: As weight drops, many people need less diabetes medication
Research shows that losing 10-15% of your body weight can dramatically improve these markers, and in many cases, lead to diabetes remission – meaning your blood sugar returns to normal levels without medication.
To access other scientific articles on the blog, you can use the following links:
- Can diabetes be treated?
- How to Stop Insulin Resistance Weight Gain
- Best Diet For Fatty Liver
- Best and Worst Drinks for Fatty Liver
- Is Milk Good for Fatty Liver?
- what fruits must diabetics avoid?
Setting Evidence-Based Type 2 Diabetes Weight Loss
When it comes to losing weight to improve type 2 diabetes, not all weight loss is equal. Research shows that specific targets can make the difference between modest improvement and potential remission. Let’s explore what the latest science tells us about effective weight loss goals.
Weight Loss Goals That Make a Difference
Research from multiple clinical trials has identified key weight loss thresholds that lead to significant improvements in diabetes:
- 5-7% weight loss: Begins to improve insulin sensitivity
- 10% weight loss: Often leads to significant reduction in diabetes medications
- 15% weight loss: Provides the best chance of diabetes remission
“Among patients who maintained at least 10-15kg of weight loss, 86% achieved diabetes remission at two years.”
DiRECT Trial, Lancet Diabetes & Endocrinology
Understanding Your Timeline
Sustainable weight loss follows a predictable pattern. Here’s what you can typically expect:
- First Month: Initial weight loss of 2-4kg with proper dietary changes
- Months 2-3: Continued steady loss of 0.5-1kg per week
- Months 4-6: Stabilization period where weight loss might slow
- Beyond 6 Months: Focus on maintenance and preventing regain
Essential Health Markers to Track
While the scale is important, other measurements provide crucial insights into your progress:
The Critical Role of Body Composition
Your body composition—the ratio of fat to muscle—plays a crucial role in diabetes management. Research shows that losing fat while preserving muscle mass provides the best outcomes for blood sugar control. Focus on these key areas:
- Visceral Fat: Reduction in abdominal fat has the greatest impact on diabetes improvement
- Muscle Mass: Maintaining muscle helps maintain metabolic health and insulin sensitivity
- Body Fat Percentage: Aim for gradual reduction while preserving lean tissue
Remember, these targets aren’t just arbitrary numbers—they’re based on extensive research showing what works for long-term diabetes improvement. The key is to approach them systematically and with proper medical supervision.
Medical Safety: Managing Weight Loss for Type 2 Diabetes
While losing weight can help reverse type 2 diabetes, doing so safely requires careful attention to your body’s signals and proper medical supervision. Understanding the medical aspects of weight loss with diabetes helps ensure your journey to better health is both effective and safe.
To access the second part of the articles related to diabetes, you can use the following links:
- What is Diabetes?
- Symptoms and Signs of Diabetes
- Difference Between Type 1 and Type 2 Diabetes
- What Are the Complications of Diabetes?
- Diabetes Diagnosis Method
- can apple cider vinegar lower blood sugar immediately?
Safe Weight Loss Rates for Diabetes Management
Research indicates that sustainable weight loss for people with type 2 diabetes typically follows these patterns:
- Initial phase: 0.5-1 kg per week (common during the first month)
- Sustainable pace: 2-4 kg per month
- Long-term goal: 10-15% of starting weight within 6 months
Losing weight too quickly can destabilize blood sugar levels and increase health risks. A steady, measured approach allows your body to adapt while maintaining stable blood sugar control.
Medication Changes During Weight Loss
As you lose weight, your body’s response to medications often changes. This is particularly important for:
- Diabetes Medications: Dosages may need adjustment as insulin sensitivity improves
- Blood Pressure Medications: Requirements often decrease with weight loss
- Other Medications: Absorption rates may change as body composition shifts
“Regular medication review during weight loss is essential as insulin requirements often decrease significantly as body weight reduces.”
Diabetes Care Journal, 2024
When to Contact Your Healthcare Provider
Immediate medical attention is needed if you experience:
- Blood sugar readings below 70 mg/dL or above 250 mg/dL
- Persistent dizziness or unusual fatigue
- Rapid weight loss exceeding 2 kg per week
- Difficulty maintaining hydration
Essential Health Monitoring
Regular monitoring helps ensure safe progress:
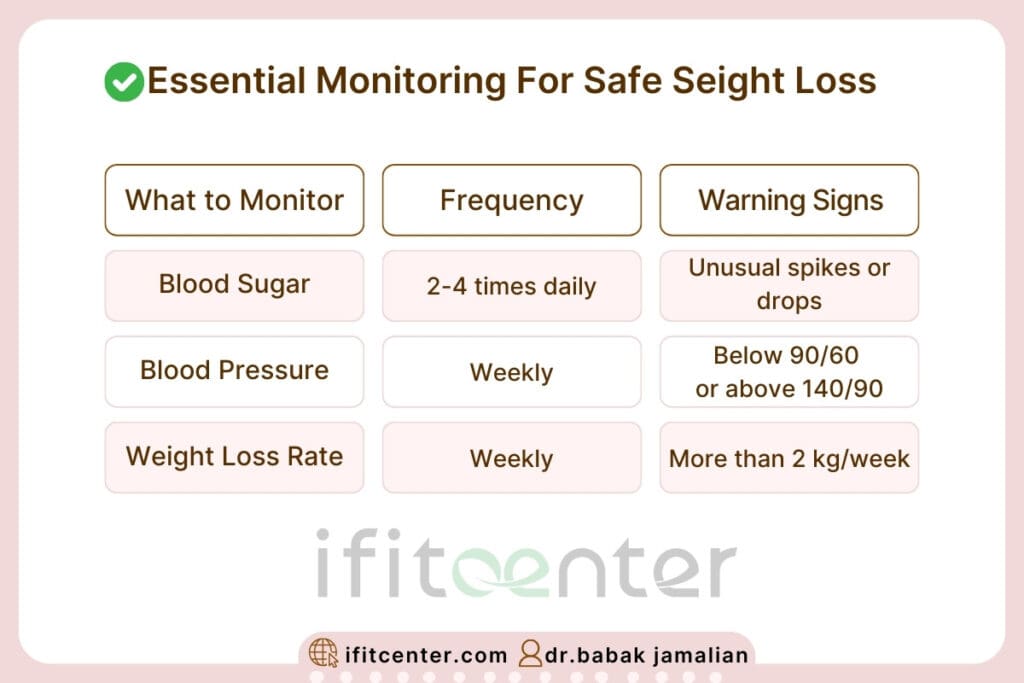
Regular check-ups with your healthcare provider become especially important during weight loss. These visits allow for timely medication adjustments and early detection of any potential issues.
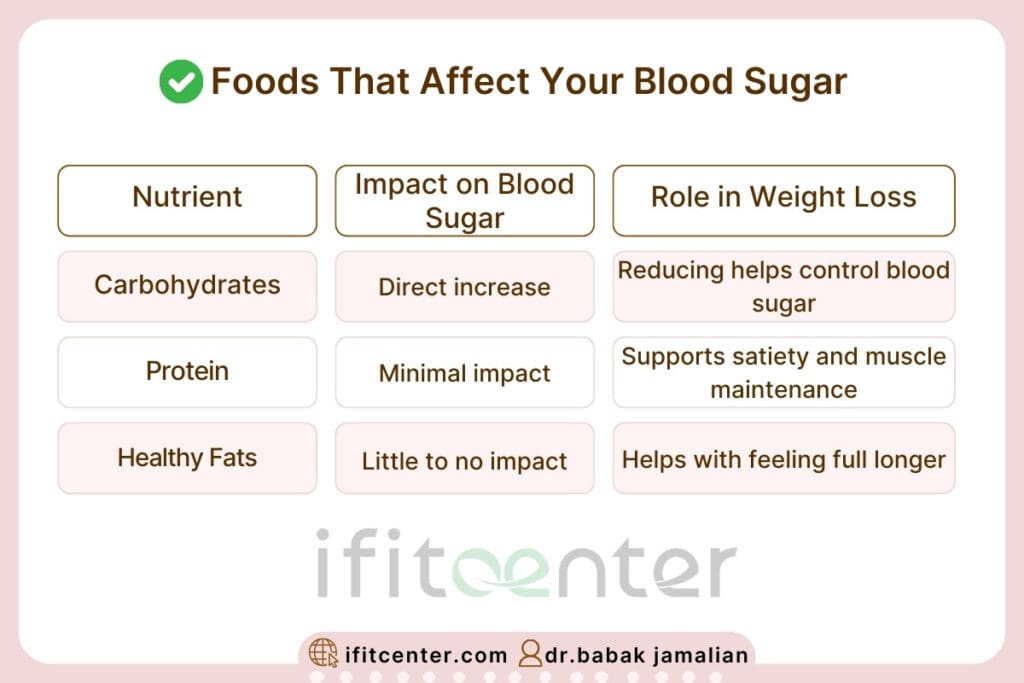
Nutrition Science: Eating to Improve Type 2 Diabetes
Understanding how different foods affect your blood sugar is key to achieving diabetes remission through weight loss. Recent research has revealed clear patterns about which dietary approaches work best for improving type 2 diabetes.
Evidence-Based Dietary Approaches
Research shows that several dietary patterns can effectively improve blood sugar control and support weight loss:
- Low Carbohydrate Approach: Can lead to significant improvements in blood sugar control within weeks
- Mediterranean Style: Emphasizes healthy fats and vegetables, showing excellent long-term results
- Time-Restricted Eating: May enhance insulin sensitivity when combined with proper food choices
“Low-carbohydrate diets achieved higher rates of diabetes remission at 6 months compared with other diets commonly recommended for management of type 2 diabetes.”
BMJ 2021
Understanding Food’s Impact on Blood Sugar
Timing Matters: When to Eat
Research has revealed that when you eat can be almost as important as what you eat:
- Morning: Your body typically handles carbohydrates better earlier in the day
- Meal Spacing: Allowing 4-5 hours between meals helps stabilize blood sugar
- Evening Cutoff: Limiting late-night eating can improve morning blood sugar readings
Common Nutrition Myths Debunked
| Myth | Reality | Scientific Evidence |
|---|---|---|
| “All carbs are bad” | Quality and quantity matter | Different carbs have varying effects on blood sugar |
| “Fruit is off-limits” | Whole fruits can be included | Fiber in fruit slows sugar absorption |
| “Eating fat makes you fat” | Healthy fats support weight loss | Helps with satiety and blood sugar control |
Building Your Meal Plan
A balanced approach includes:
- Non-starchy Vegetables: Fill half your plate
- Quality Protein: Quarter of your plate
- Complex Carbohydrates: Quarter of your plate, portion controlled
- Healthy Fats: Added in moderation
Remember, sustainable dietary changes work better than strict, unsustainable restrictions. The goal is to find an eating pattern that helps control blood sugar while being enjoyable enough to maintain long-term.
Exercise and Type 2 Diabetes: Your Guide to Safe and Effective Activity
Physical activity plays a crucial role in diabetes management and weight loss, but it’s essential to approach exercise systematically and safely. Understanding how different types of activity affect your blood sugar helps you create an effective routine that supports your weight loss goals.
Starting Safely: Your Exercise Progression Plan
Begin with these research-backed activity levels and progress gradually:
| Week | Activity Level | Duration | Frequency |
|---|---|---|---|
| 1-2 | Light walking | 10-15 minutes | 3-4 times/week |
| 3-4 | Brisk walking | 15-20 minutes | 4-5 times/week |
| 5-6 | Combined activities | 20-30 minutes | 5-6 times/week |
Types of Exercise and Their Benefits
Different forms of exercise affect your body and blood sugar in unique ways:
- Aerobic Exercise
- Improves insulin sensitivity for up to 24 hours
- Helps burn fat stores
- Examples: walking, swimming, cycling
- Resistance Training
- Builds muscle mass which improves glucose metabolism
- Enhances long-term insulin sensitivity
- Examples: bodyweight exercises, resistance bands, light weights
- Flexibility Work
- Reduces risk of injury
- Improves circulation
- Examples: gentle stretching, yoga
“Combined aerobic and resistance training shows the most significant improvements in blood sugar control and weight loss outcomes for type 2 diabetes patients.”
Diabetes Care Journal, 2024
Understanding Blood Sugar Response to Exercise
Different activities can affect your blood sugar in various ways:
| Activity Type | Typical Blood Sugar Response | Monitoring Needs |
|---|---|---|
| Moderate Walking | Gradual decrease | Check before and after |
| Strength Training | May temporarily increase | Check before, during, after |
| High-Intensity Exercise | Can vary significantly | Frequent monitoring needed |
Building a Sustainable Exercise Routine
Follow these principles to create a lasting exercise habit:
- Start Small: Begin with activities you enjoy and can maintain
- Progress Gradually: Increase duration or intensity by no more than 10% weekly
- Mix Activities: Combine different types of exercise for optimal results
- Listen to Your Body: Adjust based on energy levels and blood sugar readings
Tracking Your Progress: Beyond the Scale
Successfully managing type 2 diabetes through weight loss requires tracking more than just the number on your scale. Understanding and monitoring the right health markers helps you make informed decisions about your journey and ensures you’re moving toward diabetes remission.
Key Health Markers to Monitor
| Health Marker | What It Tells You | How Often to Check |
|---|---|---|
| Morning Blood Sugar | Baseline glucose control | Daily |
| Post-meal Blood Sugar | Food response | 1-2 times daily |
| HbA1c | 3-month blood sugar average | Every 3 months |
| Body Composition | Fat vs. muscle changes | Monthly |
| Waist Circumference | Abdominal fat changes | Bi-weekly |
Understanding Your Progress Patterns
Progress in managing diabetes through weight loss typically follows specific patterns:
- Early Phase (1-4 weeks)
- Rapid improvements in blood sugar
- Initial weight loss
- Increased energy levels
- Adaptation Phase (1-3 months)
- Steadier weight loss
- Stabilizing blood sugar patterns
- Possible medication adjustments
- Long-term Phase (3+ months)
- Sustained improvements
- More consistent patterns
- Focus on maintenance
Making Sense of Your Numbers
Look for these positive indicators in your tracking:
- Blood Sugar Patterns
- More stable daily readings
- Lower morning numbers
- Better post-meal recovery
- Physical Changes
- Looser waistbands
- Increased energy
- Better sleep quality
Navigating Plateaus
Progress plateaus are normal and often occur in predictable patterns:
| Plateau Type | Common Timing | Adjustment Strategy |
|---|---|---|
| Early Plateau | 4-6 weeks | Review food portions |
| Metabolic Plateau | 3-4 months | Adjust activity levels |
| Long-term Plateau | 6+ months | Reassess overall plan |
When to Adjust Your Approach
Consider making changes when you notice:
- No change in blood sugar patterns for two weeks
- Weight stable for more than three weeks
- Energy levels consistently low
- Hunger increasing significantly
“Regular monitoring and timely adjustments are key factors in achieving diabetes remission through weight loss.”
Diabetes Care Journal, 2024
Remember, progress isn’t always linear. Focus on the overall trend of your health markers rather than daily fluctuations.
Maintaining Type 2 Diabetes Remission: Your Long-Term Success Guide
While achieving diabetes remission through weight loss is a significant accomplishment, maintaining these improvements requires understanding the factors that contribute to long-term success. Research has identified key strategies that help people sustain their progress and prevent diabetes relapse.
What Research Shows About Long-Term Success
Studies of successful long-term diabetes remission reveal common patterns:
- Consistent Monitoring: Regular blood sugar checking even after achieving target levels
- Weight Maintenance: Keeping weight within 5% of target
- Ongoing Support: Regular check-ins with healthcare providers
- Active Lifestyle: Maintaining regular physical activity
“Among patients who maintained their weight loss, 86% remained in diabetes remission at two years.”
DiRECT Trial Follow-up Study
Key Behavioral Patterns for Success
| Behavior | Impact on Success | Implementation Strategy |
|---|---|---|
| Regular Self-Monitoring | 3x higher success rate | Daily tracking routine |
| Meal Planning | 2x better maintenance | Weekly preparation |
| Social Support | 70% higher success | Regular group activities |
Building Sustainable Habits
Research identifies these core habits as essential for maintaining diabetes remission:
- Consistent Meal Timing
- Regular eating schedule
- Planned portions
- Mindful eating practices
- Active Lifestyle Integration
- Daily movement goals
- Variety in activities
- Social exercise opportunities
- Stress Management
- Regular relaxation practices
- Adequate sleep routine
- Work-life balance
Managing Common Challenges
| Challenge | Warning Signs | Prevention Strategy |
|---|---|---|
| Gradual Weight Regain | Clothes fitting tighter | Weekly weigh-ins, early intervention |
| Rising Blood Sugar | Morning readings increasing | Food and activity log review |
| Motivation Decline | Skipping monitoring routines | Reset small, achievable goals |
Creating Your Support System
Long-term success is significantly improved with:
- Regular medical check-ups
- Connection with others on similar journeys
- Family involvement in lifestyle changes
- Professional guidance for ongoing adjustments
Remember, maintaining diabetes remission is not about perfection but about developing sustainable patterns that you can maintain for life. Small adjustments, made consistently, lead to lasting success.
Key Takeaways: How to Lose Weight with Diabetes Type 2?
The science is clear: type 2 diabetes doesn’t have to be a lifelong condition. Through evidence-based weight management, many people can achieve significant improvements in their blood sugar control and potentially even diabetes remission. Here’s what we’ve learned about this journey:
Understanding the Process
- The Weight-Diabetes Connection: Excess weight, particularly around the abdomen, directly impacts how your body processes blood sugar
- Evidence-Based Targets: Weight loss of 10-15% can lead to significant improvements, with some people achieving complete remission
- Medical Safety: Proper monitoring and medication adjustment ensure safe progress toward better health
Taking Action
- Nutrition Science: Understanding how different foods affect your blood sugar enables better dietary choices
- Physical Activity: Safe, progressive exercise supports both weight loss and blood sugar control
- Progress Tracking: Regular monitoring of key health markers guides your journey effectively
Maintaining Success
- Long-Term Habits: Sustainable lifestyle changes support lasting improvements
- Regular Monitoring: Keeping track of progress helps maintain improvements
- Support System: Professional guidance and personal support enhance success
“The journey to better health through weight management isn’t about quick fixes—it’s about sustainable changes that improve your life for years to come.”
Remember that improving type 2 diabetes through weight loss is a journey that requires patience, understanding, and proper support. While the path may have challenges, the potential rewards—better health, reduced medication needs, and possibly even diabetes remission—make it worthwhile.
Whether you’re just starting or already on your way, focus on sustainable changes rather than quick fixes. With proper medical guidance and commitment to healthy lifestyle changes, significant improvements in your diabetes management are possible.
To access other content on the IFitCenter’s blog, you can use the following links:
References for Diabetes Type 2 Weight Loss
This article is based on the following peer-reviewed research and authoritative sources:
- Lean ME, Leslie WS, Barnes AC, et al. (2018). Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. The Lancet, 391(10120):541-551. DOI: 10.1016/S0140-6736(17)33102-1
- Lean MEJ, Leslie WS, Barnes AC, et al. (2019). Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol, 7(5):344-355. DOI: 10.1016/S2213-8587(19)30068-3
- Taylor R, Al-Mrabeh A, Zhyzhneuskaya S, et al. (2018). Remission of Human Type 2 Diabetes Requires Decrease in Liver and Pancreas Fat Content but is Dependent upon Capacity for β Cell Recovery. Cell Metabolism, 28:547-556. DOI: 10.1016/j.cmet.2018.07.003
- Churuangsuk C, Hall J, Reynolds A, et al. (2022). Diets for weight management in adults with type 2 diabetes: an umbrella review of published meta-analyses and systematic review of trials of diets for diabetes remission. Diabetologia, 65:14-36. DOI: 10.1007/s00125-021-05577-2
- McInnes N, Smith A, Otto R, et al. (2017). Piloting a Remission Strategy in Type 2 Diabetes: Results of a Randomized Controlled Trial. The Journal of Clinical Endocrinology & Metabolism, 102(5):1596-1605. DOI: 10.1210/jc.2016-3373
- American Diabetes Association (2024). Standards of Medical Care in Diabetes—2024. Diabetes Care, 47(Supplement 1). DOI: 10.2337/dc24-SINT
- Davies MJ, D’Alessio DA, Fradkin J, et al. (2018). Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care, 41(12):2669-2701. DOI: 10.2337/dci18-0033
- Taylor R. (2022). Your Simple Guide to Reversing Type 2 Diabetes: The 3-step Plan to Transform Your Health. Short Books Ltd. ISBN: 978-1780724096
- Riddle MC, Cefalu WT, Evans PH, et al. (2021). Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes. Diabetes Care, 44:2438-2444. DOI: 10.2337/dci21-0034



