Only heavy drinkers get fatty liver disease! You can’t reverse liver damage! If you don’t feel sick, your liver is fine! These common beliefs about fatty liver disease aren’t just wrong – they’re potentially dangerous. The truth? Modern science reveals a very different story.
In fact, the most common type of fatty liver disease has nothing to do with alcohol. Medical science now recognizes it as “metabolic dysfunction-associated steatotic liver disease” (MASLD) – a condition that can affect anyone, regardless of their drinking habits. Even more surprising? You can have a perfectly healthy weight and still develop fatty liver disease.
Today at IFitCenter, we’re tackling these misconceptions head-on, providing you with evidence-based facts about fatty liver disease. Understanding this condition is your first step toward better liver health – and we’re here to make that understanding crystal clear.
What is Fatty Liver Disease?
Imagine your liver as your body’s filtration plant. Just like a water filter that gets clogged with debris over time, your liver can become “clogged” with excess fat. When fat makes up more than 5% of your liver’s total weight, doctors diagnose this condition as fatty liver disease.
In recent years, medical understanding of this condition has evolved significantly. What was once called Non-Alcoholic Fatty Liver Disease (NAFLD) is now known as Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD). This name change reflects our deeper understanding that the condition is closely tied to how our body processes energy.
On the IFitCenter blog, we have published a free content database about fatty liver disease that can have a significant impact for you in controlling and preventing this disease. For access, simply use the links below:
- fatty liver Symptoms
- causes of fatty liver
- fatty liver test results
- is dark chocolate good for fatty liver?
- fatty liver disease diagnosis
- egg for fatty liver
Types of Fatty Liver Disease
There are two main types of fatty liver disease, each with distinct causes and characteristics:
- Metabolic Dysfunction-Associated Fatty Liver (MASLD): Previously known as NAFLD, this type is related to how your body processes food and energy. It’s closely linked to conditions like type 2 diabetes and obesity.
- Alcoholic Fatty Liver Disease: Caused by excessive alcohol consumption, this type develops when the liver becomes overwhelmed by processing alcohol.
MASLD can further progress into more serious conditions:
- Simple Fatty Liver: Fat accumulation without significant inflammation
- Metabolic Dysfunction-Associated Steatohepatitis (MASH): Fat accumulation with inflammation and liver cell damage
- Cirrhosis: Advanced scarring resulting from long-term liver damage
“The shift from NAFLD to MASLD represents a fundamental change in how we understand fatty liver disease. This isn’t just a liver problem – it’s a metabolic condition affecting the entire body.”The Lancet Gastroenterology & Hepatology, 2024
“The shift from NAFLD to MASLD represents a fundamental change in how we understand fatty liver disease. This isn’t just a liver problem – it’s a metabolic condition affecting the entire body.”The Lancet Gastroenterology & Hepatology, 2024
How Does a Liver Become Fatty?
Your liver can become fatty through several interconnected pathways. Think of it like a busy kitchen that’s suddenly overwhelmed with too many orders. When this happens, three main problems can occur:
The Role of Insulin Resistance
At the heart of fatty liver development is often a condition called insulin resistance. Insulin is like your body’s traffic controller, directing nutrients where they need to go. When cells become resistant to insulin’s signals, it’s like having a traffic jam in your metabolism. This leads to high blood sugar levels and increased fat storage in the liver.
Factors That Contribute to Fatty Liver
Several factors can contribute to developing fatty liver disease:
- Dietary choices (especially high intake of processed sugars and carbohydrates)
- Sedentary lifestyle
- Genetic predisposition
- Environmental toxins
- Certain medications
Signs and Symptoms of Fatty Liver Disease
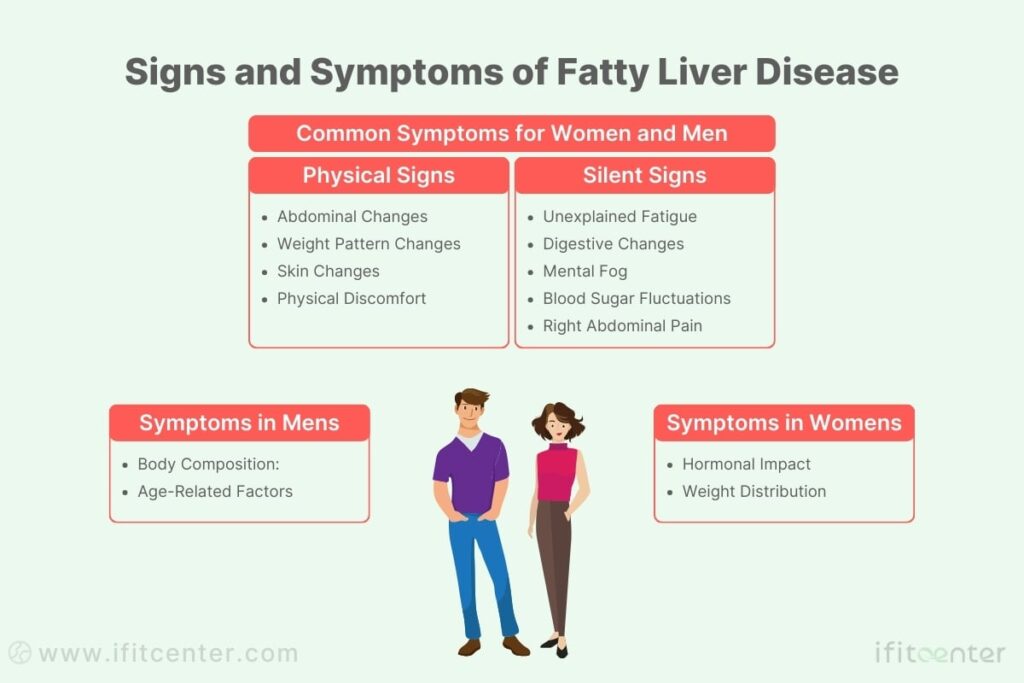
Fatty liver disease is often called a “silent condition” because it can develop and progress without obvious symptoms. Understanding the subtle signs can make a crucial difference in early detection and treatment success.
Silent Signs of Fatty Liver Disease
The early stages of fatty liver disease often go unnoticed, but there are subtle signals your body may be sending:
- Unexplained Fatigue: Feeling tired despite adequate sleep
- Digestive Changes: Occasional nausea or loss of appetite
- Mental Fog: Difficulty concentrating or memory issues
- Blood Sugar Fluctuations: Difficulty maintaining stable energy levels
- Significant Pain: Especially in the right abdominal area below the rib cage.
Physical Signs of Fatty Liver Disease
As the condition progresses, more noticeable physical symptoms may develop:
- Abdominal Changes: Discomfort or pain in the upper right abdomen
- Weight Pattern Changes: Difficulty losing weight despite effort
- Skin Changes: Spider-like blood vessels or reddened palms
- Physical Discomfort: Swelling in ankles and legs
“Recent research shows that up to 30-40% of people with fatty liver disease experience no symptoms until the condition has significantly progressed.”
The Lancet Gastroenterology & Hepatology, 2024
Gender-Specific Symptoms in Women
Women may experience unique manifestations of fatty liver disease, often influenced by hormonal factors:
- Hormonal Impact: Irregular menstrual cycles or worsening PMS symptoms
- Weight Distribution: Changes in body fat patterns
Gender-Specific Symptoms in Men
Men often show different patterns of fatty liver disease manifestation:
- Body Composition: Increased abdominal fat distribution
- Age-Related Factors: Higher risk after age 50
When to Seek Medical Attention
It’s crucial to consult a healthcare provider if you experience:
- Persistent fatigue that doesn’t improve with rest
- Unexplained weight loss or gain
- Yellowing of skin or eyes
- Severe abdominal pain or swelling
- Dark-colored urine or pale stools
Early detection through regular health screenings remains the most effective way to identify and address fatty liver disease before it progresses to more serious stages.
How to Diagnose Fatty Liver Disease
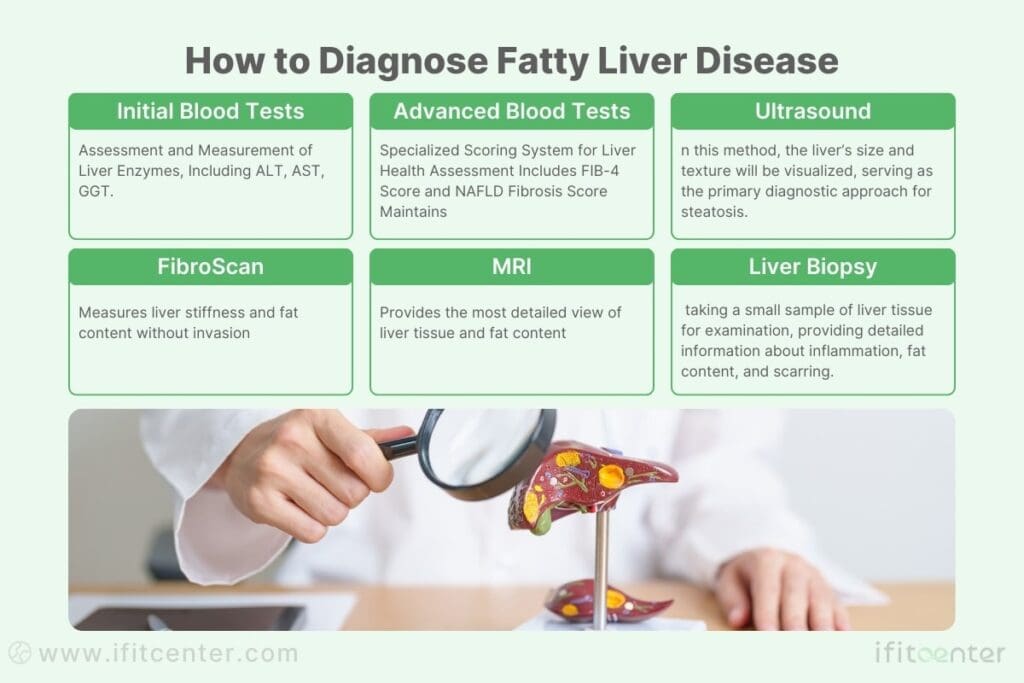
Diagnosing fatty liver disease requires a systematic approach, starting from basic blood tests to advanced imaging techniques. Understanding these tests can help you better engage with your healthcare journey.
Initial Blood Tests and Screening
The journey to diagnosing fatty liver disease typically begins with blood tests that measure liver enzyme levels:
- ALT (Alanine Aminotransferase): Normal range: For women 8-41 U/L | For men 9-59 U/L
- AST (Aspartate Aminotransferase): Normal range: 10-40 units/liter
- GGT (Gamma-Glutamyl Transferase): Normal range: For women 6-40 U/L | For men 12-68 U/L
It’s important to note that normal ranges can vary slightly between laboratories, and results should always be interpreted by a healthcare professional.
Advanced Blood Tests and Scoring Systems
Beyond basic liver function tests, doctors use specialized scoring systems to assess liver health:
- FIB-4 Score: Combines age, platelet count, and liver enzymes to predict fibrosis risk
- NAFLD Fibrosis Score: Evaluates the likelihood of severe liver scarring
Imaging Studies for Fatty Liver
Modern imaging techniques provide detailed views of liver health:
- Ultrasound: The first-line imaging test, showing liver size and texture (first-line for detecting steatosis)
- FibroScan: Measures liver stiffness and fat content without invasion
- MRI: Provides the most detailed view of liver tissue and fat content
“Recent advances in imaging technology allow us to detect fatty liver disease earlier than ever before, often before symptoms appear.”
The Lancet Gastroenterology & Hepatology, 2024
Understanding FibroScan Results
FibroScan provides two key measurements:
- Liver Stiffness: Measured in kilopascals (kPa)
– Normal: Below 7 kPa
– Mild fibrosis: 7-10 kPa
– Advanced fibrosis: Above 10 kPa - CAP Score: Measures liver fat content
– Normal: Below 250 dB/m
– Mild fatty liver: 250-300 dB/m
– Severe fatty liver: Above 300 dB/m
Liver Biopsy: The Gold Standard
While less commonly needed today, liver biopsy remains the most definitive test for fatty liver disease. It’s typically recommended when:
- Other test results are unclear or conflicting
- There’s suspicion of other liver conditions
- Advanced disease needs to be confirmed
- Treatment decisions depend on precise staging
The biopsy procedure involves taking a small sample of liver tissue for microscopic examination, providing detailed information about inflammation, fat content, and scarring.
To access the second part of the fatty liver content, I invite you to use the links below:
- Which vitamin is best for fatty liver?
- is fish oil good for your liver
- what foods help cure a fatty liver
- foods to avoid with fatty liver
- best fruit for fatty liver
- low fat milk is good for fatty liver
What Are the Risks of Fatty Liver Disease?
Understanding the risks associated with fatty liver disease is crucial for recognizing the importance of early intervention and treatment. While the condition is often reversible in its early stages, untreated fatty liver disease can lead to serious health complications.
Immediate Health Risks
When fatty liver disease first develops, it can affect your health in several ways:
- Liver Inflammation: Fat accumulation triggers inflammatory responses, affecting liver function
- Metabolic Disruption: Impaired blood sugar control and energy metabolism
- Increased Cardiovascular Risk: Higher risk of heart-related complications
- Reduced Energy Levels: Compromised liver function affecting daily activities
“Recent research shows that individuals with fatty liver disease have a 2.22 times higher risk of developing type 2 diabetes compared to those without the condition.”
The Lancet Gastroenterology & Hepatology, 2024
Long-term Health Complications
Without proper management, fatty liver disease can progress to more serious conditions:
- Liver Scarring (Fibrosis): Approximately 5-12% of people with fatty liver disease develop liver scarring within a decade if left untreated
- Cirrhosis: Advanced scarring that can severely impact liver function
- Liver Cancer Risk: Studies show a 3.5-fold increased risk of liver cancer in advanced cases
- System-Wide Effects: Impact on kidney function, cardiovascular health, and metabolic balance
Impact on Overall Health
Fatty liver disease affects more than just your liver. Research shows connections to:
- Increased risk of heart disease
- Higher likelihood of developing type 2 diabetes
- Greater chance of kidney problems
Prevention and Risk Reduction
The good news is that many risks can be significantly reduced through early intervention:
- Early Detection: Regular health screenings can catch problems before they progress
- Lifestyle Changes: Proper diet and exercise can reverse early-stage fatty liver
- Medical Monitoring: Regular check-ups to track liver health
- Risk Factor Management: Controlling diabetes, weight, and cardiovascular health
Understanding these risks emphasizes the importance of taking action early. With proper management and lifestyle changes, many of these complications can be prevented or minimized.
Fatty Liver Disease Treatments
Treatment for fatty liver disease focuses on addressing the root causes through scientifically proven lifestyle modifications. Research shows that with the right approach, fatty liver disease can be reversed in many cases.
The most effective approach to treating fatty liver disease is a combination of targeted lifestyle modifications and emerging medical therapies. Research has shown that a structured diet, particularly the Mediterranean diet, coupled with regular exercise, can significantly reduce liver fat content. Additionally, bioactive compounds such as curcumin and resveratrol, as well as pharmaceutical interventions like GLP-1 receptor agonists, have demonstrated promising results in clinical trials.”
Dr. Babak Jamalian, Family Physician Specialist.
Evidence-Based Nutritional Strategies
Studies indicate that dietary changes play a crucial role in treating fatty liver disease. Research published in The Lancet shows up to 30% reduction in liver fat within 6 weeks with appropriate dietary modifications.
Foods to Reduce or Avoid
- Refined Carbohydrates: Processed foods, white bread, pastries
- Added Sugars: Especially fructose-containing products
- Industrial Seed Oils: High in inflammatory omega-6 fatty acids
- Alcohol: Even moderate consumption can impact liver health
Beneficial Foods for Liver Health
- Protein-Rich Foods: Support liver repair and maintenance
- Fiber-Rich Vegetables: Aid in toxin removal and gut health
- Healthy Fats: Omega-3 sources like fatty fish
- Antioxidant-Rich Foods: Berries, leafy greens, cruciferous vegetables
“Recent research shows that metabolic health improvements can begin within days of adopting appropriate dietary changes.”Journal of Hepatology, 2024
The Role of Weight Management
Weight loss significantly impacts liver health, but it must be approached safely and sustainably:
- Target Rate: 0.5-1 kg per week (evidence shows this is optimal for liver health)
- Initial Goal: 5-10% body weight reduction can show significant improvements
- Long-term Strategy: Focus on sustainable habits rather than rapid weight loss
Exercise Guidelines for Fatty Liver
Physical activity plays a crucial role in treatment success:
- Aerobic Exercise: 150 minutes per week of moderate activity
- Resistance Training: 2-3 sessions per week for muscle health
- Daily Movement: Reducing sedentary time through regular activity
Lifestyle Optimization
Comprehensive treatment includes important lifestyle modifications:
- Sleep Quality: 7-9 hours of quality sleep supports liver recovery
- Stress Management: Chronic stress can impact liver health
- Regular Timing: Consistent meal and activity schedules
- Habit Formation: Building sustainable healthy routines
Success in treating fatty liver disease requires a comprehensive approach combining these elements into a sustainable lifestyle plan.
Don’t Just Treat Symptoms—Fix the Root Cause of Fatty Liver
Fatty liver isn’t just about the liver—it’s a metabolic condition that affects your whole body. That’s why simply cutting out certain foods isn’t enough. Sustained fat loss, hormonal balance, and medical guidance are essential to prevent progression to liver damage.
At iFitCenter, we offer:
✔ Comprehensive liver function assessments to understand your unique needs
✔ A structured weight loss and metabolic program that prioritizes liver health
✔ Ongoing medical supervision to track improvements and prevent relapses
Fatty liver is reversible—but only if you take action now. Get started with expert care today!
Common Misconceptions About Fatty Liver Disease
When it comes to fatty liver disease, many common beliefs can mislead people about their health. Let’s examine five widespread myths and uncover the scientific truth behind each one.
Myth #1: “Only Alcoholics Get Fatty Liver Disease”
The Truth: Research published in The Lancet shows that metabolic dysfunction-associated fatty liver disease (MASLD) affects up to 30% of the global population, regardless of alcohol consumption. In fact, studies indicate that approximately 75% of fatty liver cases are unrelated to alcohol use.
“Current evidence shows that metabolic factors, rather than alcohol, are now the leading cause of fatty liver disease worldwide.”
Journal of Hepatology, 2024
Myth #2: “Fatty Liver Disease Is Irreversible”
The Truth: Recent research demonstrates that fatty liver disease is often reversible, especially in its early stages. Studies show that appropriate lifestyle changes can reduce liver fat by up to 50% within 14 days. The liver has remarkable regenerative capabilities when given proper support.
Myth #3: “You Need Medication to Treat Fatty Liver Disease”
The Truth: While medications may be helpful in some cases, research shows that lifestyle modifications are the primary and most effective treatment. Clinical studies demonstrate that proper nutrition and exercise alone can reverse fatty liver disease in many cases, without medication.
Myth #4: “You Must Avoid All Fats to Treat Fatty Liver”
The Truth: Scientific evidence indicates that healthy fats are actually crucial for liver health. Research shows that certain fats, particularly omega-3 fatty acids, can help reduce liver inflammation and improve overall liver function. The key is choosing the right types of fats while managing overall caloric intake.
Myth #5: “Fatty Liver Has No Symptoms”
The Truth: While early stages may be asymptomatic, research indicates that up to 75% of people with fatty liver disease experience some symptoms. These can include fatigue, right-sided abdominal discomfort, and various metabolic disturbances.
Understanding these truths about fatty liver disease is crucial for proper management and treatment. While some myths may contain elements of truth, the scientific evidence provides a much more nuanced and hopeful picture of this condition.
| Myth | Scientific Reality |
|---|---|
| Only alcoholics get fatty liver | 75% of cases are non-alcohol related |
| Condition is irreversible | 50% improvement possible within weeks |
| Medication is necessary | Lifestyle changes are primary treatment |
| Avoid all fats | Healthy fats aid liver recovery |
| No symptoms present | 75% experience some symptoms |
Fatty Liver Management and Long-term Success at IFitCenter
Successfully managing fatty liver disease requires a comprehensive, scientifically-grounded approach combined with personalized support. At IFitCenter, we integrate evidence-based protocols with individualized care to help patients achieve lasting results.
Evidence-Based Treatment Approach
Under the guidance of Dr. Babak Jamalian, who brings over 25 years of medical experience to fatty liver management, our approach focuses on three key principles:
- Comprehensive Assessment: Understanding each patient’s unique metabolic profile
- Personalized Protocols: Tailoring interventions based on scientific evidence
- Regular Monitoring: Tracking progress through validated medical markers
“The key to successful fatty liver management lies in understanding each patient’s unique metabolic profile and creating sustainable, personalized interventions.”Dr. Babak Jamalian
Supporting Long-term Success
Research shows that successful long-term management of fatty liver disease requires ongoing support and monitoring. Our program includes:
- Regular Health Assessments: Monitoring liver function and metabolic health markers
- Lifestyle Integration Support: Practical guidance for maintaining healthy habits
- Progress Tracking: Using advanced diagnostic tools to measure improvements
- Ongoing Education: Keeping patients informed about the latest research and recommendations
Measuring Success
Our evidence-based program tracks multiple markers of progress:
- Liver function improvements through regular blood tests
- Body composition changes using advanced analysis
- Metabolic health markers including blood sugar control
- Quality of life improvements
Ongoing Support System
Long-term success requires comprehensive support. Our program provides:
- Regular Check-ins: Scheduled monitoring of progress
- Adjustment Protocols: Fine-tuning treatment based on response
- Educational Resources: Continuous learning opportunities
- Community Support: Connection with others on similar journeys
Through this comprehensive approach, we help patients not only improve their liver health but maintain those improvements for the long term.
Ready to start your journey to better liver health? Schedule a consultation to learn more about our comprehensive management program.
Taking Action Against Fatty Liver Disease
Understanding fatty liver disease is the first step toward better health. Research shows that early intervention and consistent lifestyle changes can lead to significant improvements in liver health, often within a matter of weeks.
Key Takeaways
- Early Detection Matters: Fatty liver disease is often reversible when caught early
- Lifestyle Changes Work: Scientific evidence shows up to 50% reduction in liver fat through proper diet and exercise
- Comprehensive Approach: Success comes from addressing multiple factors: nutrition, physical activity, sleep, and stress management
- Professional Support: Working with healthcare providers increases success rates significantly
Your Action Plan
Take these evidence-based steps to start improving your liver health:
- Schedule a comprehensive health assessment to understand your current liver status
- Begin implementing dietary changes, focusing on reducing processed foods and sugars
- Start a regular exercise routine, aiming for 150 minutes of moderate activity weekly
- Establish consistent sleep patterns and stress management practices
- Set up regular monitoring to track your progress
Hope for Recovery
Recent medical research provides substantial hope for those affected by fatty liver disease. Studies show that with proper intervention:
- Most patients see improvements within 3-6 months of consistent lifestyle changes
- Liver function often returns to normal ranges with proper management
- Long-term success is achievable with sustained healthy habits
Additional Resources
To support your journey toward better liver health, consider these valuable resources:
- Latest research from The Journal of Hepatology
- Guidelines from the American Association for the Study of Liver Diseases
- Educational materials from the European Association for the Study of the Liver
- Support groups and community resources
“With current medical knowledge and proper support, fatty liver disease is a condition we can effectively address. The key is taking action early and staying committed to positive changes.”
Remember, your journey to better liver health is a marathon, not a sprint. Each positive step you take brings you closer to your goal of improved health and well-being.
- Cabot, S. (2015). The Liver Cleansing Diet. SCB International.
- Hyman, M. (2012). The Blood Sugar Solution: The UltraHealthy Program for Losing Weight, Preventing Disease, and Feeling Great Now!. Little, Brown and Company.
To access other content on the IFitCenter’s blog, you can use the following links:
References for What Is a Fatty Liver and What Causes It
- Loomba, R., et al. (2024). “Tirzepatide for Metabolic Dysfunction-Associated Steatohepatitis with Liver Fibrosis.” New England Journal of Medicine.
- Sanyal, A. J., et al. (2024). “A Phase 2 Randomized Trial of Survodutide in MASH and Fibrosis.” New England Journal of Medicine.
- lasmari, A., et al. (2023). “Ramadan Fasting Model Exerts Hepatoprotective, Anti-obesity, and Anti-Hyperlipidemic Effects in an Experimentally-induced Nonalcoholic Fatty Liver in Rats.” bioRxiv.
- Eslam, M., Sanyal, A. J., George, J. (2020). MAFLD: A Consensus-Driven Redefinition of NAFLD. Gastroenterology, 158(7), 1999-2014. [DOI:10.1053/j.gastro.2019.11.312]
- Younossi, Z. M., et al. (2018). Global Burden of NAFLD and NASH: Trends, Predictions, Risk Factors, and Prevention. Nature Reviews Gastroenterology & Hepatology, 15(1), 11-20. [DOI:10.1038/nrgastro.2017.109]
- Chalasani, N., et al. (2018). The Diagnosis and Management of NAFLD: Practice Guidance from the American Association for the Study of Liver Diseases. Hepatology, 67(1), 328-357. [DOI:10.1002/hep.29367]
- American Association for the Study of Liver Diseases (AASLD) – Guidance on NAFLD Diagnosis & Treatment
- World Health Organization (WHO) – Global Report on Noncommunicable Diseases
- National Institutes of Health (NIH) – Fatty Liver Disease Overview



