Do you worry about what might happen if diabetes isn’t properly managed? Are you concerned about how diabetes might affect your eyes, kidneys, or heart over time? Have you wondered why healthcare providers emphasize controlling blood sugar so emphatically? The answer lies in understanding the complications of diabetes—the wide-ranging effects this condition can have throughout the body when glucose levels remain elevated for extended periods.
For many people with diabetes, the fear of complications can be more distressing than managing the condition itself. And with good reason—complications of diabetes can affect virtually every system in the body, from your vision and kidney function to your heart health and nerve sensation. What makes these complications particularly concerning is that they often develop silently, without obvious symptoms, until significant damage has already occurred.
At IFitCenter, we recognize that knowledge is power when it comes to diabetes management. That’s why we’ve developed this comprehensive guide to diabetes complications—not to cause alarm, but to provide the essential information that empowers you to recognize potential warning signs and take proactive steps. Whether you’re recently diagnosed or have been managing diabetes for years, understanding possible complications is a crucial part of your health journey.
Microvascular Complications of Diabetes
Microvascular complications affect the body’s smallest blood vessels. High blood glucose damages these tiny vessels over time, particularly in three vulnerable areas: the eyes (retinopathy), kidneys (nephropathy), and nerves (neuropathy).
These complications typically develop silently over years, often without symptoms until significant damage has occurred. Let’s examine each complication in detail.
Diabetic Retinopathy
Diabetic retinopathy damages the retina—the light-sensitive tissue at the back of your eye. Elevated glucose weakens tiny blood vessels in the retina, causing them to leak fluid or blood, swell, or develop abnormal branches.
Diabetic retinopathy progresses through these stages:
- Mild Non-proliferative Retinopathy: Small balloon-like swellings appear in retinal blood vessels. Most people have no symptoms at this stage.
- Moderate Non-proliferative Retinopathy: More blood vessels become blocked, reducing nourishment to the retina.
- Severe Non-proliferative Retinopathy: Many blood vessels are blocked, depriving retinal areas of blood supply.
- Proliferative Retinopathy: New, fragile blood vessels grow along the retina and into the eye’s vitreous gel. These easily leak and bleed, causing severe vision loss.
Diabetic macular edema—fluid leakage into the macula—can occur at any stage and cause significant vision problems.
Common vision effects include:
- Blurred or fluctuating vision
- Impaired color vision
- Empty areas in your vision
- Floating spots or dark strings
- Vision loss
Diabetic Nephropathy
Diabetic nephropathy is kidney damage caused by diabetes. Your kidneys contain millions of tiny blood vessel clusters (glomeruli) that filter waste. High blood sugar damages this filtering system, creating larger holes that allow proteins to leak through.
Kidney disease typically progresses through these stages:
- Hyperfiltration: Kidneys work harder than normal. Function tests may appear normal despite early kidney stress.
- Microalbuminuria: Small amounts of albumin protein leak into urine—the first detectable sign of damage.
- Macroalbuminuria: Larger amounts of proteins leak as kidney filtering function declines.
- End-Stage Renal Disease: Kidneys may fail completely, requiring dialysis or transplantation.
Kidney disease often progresses without symptoms until significant damage occurs. Later symptoms may include swelling, fatigue, nausea, poor appetite, itching, and changes in urination.
“One of the most concerning aspects of diabetic kidney disease is its silent progression. By the time symptoms appear, significant damage has often occurred. What many patients don’t realize is that specialized kidney assessments can detect changes in kidney function up to 5-7 years before standard tests show abnormalities. These early structural changes, particularly in the glomerular basement membrane and mesangial matrix, provide a critical window for intervention when treatments are most effective.”
Dr. Babak Jamalian, Family Physician.
Diabetic Neuropathy
Diabetic neuropathy is nerve damage resulting from diabetes. High blood glucose damages nerves directly and affects the small blood vessels that supply them with nutrients.
The four main types of diabetic neuropathy include:
Peripheral Neuropathy
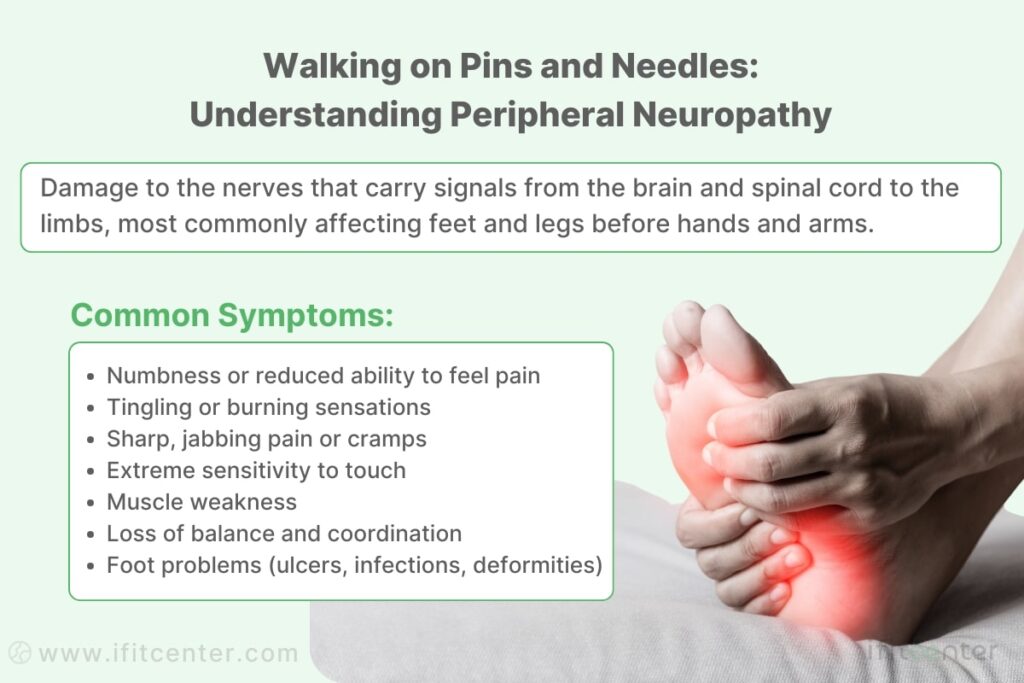
Peripheral neuropathy affects nerves in feet and legs first, later potentially spreading to hands and arms. Symptoms include:
- Numbness or reduced ability to feel pain or temperature
- Tingling or burning sensations
- Sharp pains or cramps
- Increased sensitivity to touch
- Foot problems including ulcers and infections
Autonomic Neuropathy
Autonomic neuropathy affects nerves controlling internal organs, causing problems in:
- Digestive system: Nausea, vomiting, diarrhea, constipation
- Cardiovascular system: Rapid heart rate, dizziness when standing
- Urinary and sexual function: Infections, incontinence, erectile dysfunction
- Sweat glands: Abnormal sweating and heat intolerance
On the IFitCenter blog, we have provided a comprehensive guide for diabetes, completely free of charge and based on the latest research. By viewing these articles, in addition to increasing your general knowledge in this field, you can easily manage this disease in a principled manner. To access the first part of the articles, simply use the links below:
- What is Diabetes?
- Symptoms and Signs of Diabetes
- Difference Between Type 1 and Type 2 Diabetes
- Diabetes Diagnosis Method
- Is Diabetes Curable?
- How Does Diabetes Develop?
Proximal Neuropathy
Proximal neuropathy affects nerves in thighs, hips, and buttocks, causing sudden pain, muscle weakness, and difficulty rising from a sitting position. Symptoms often improve over time.
Focal Neuropathy
Focal neuropathy affects a single nerve, causing symptoms like double vision, facial paralysis, or localized pain. It typically resolves within months without lasting damage.
Macrovascular Complications of Diabetes
While microvascular complications affect small blood vessels, macrovascular complications impact the body’s larger blood vessels. These complications are mainly driven by atherosclerosis—the buildup of fats, cholesterol, and other substances in and on artery walls. People with diabetes develop atherosclerosis at an accelerated rate, leading to serious cardiovascular problems.
Your Weight, Your Heart, Your Health: Take Control with IFitCenter
While diabetes complications can be daunting, the good news is that many can be prevented or significantly delayed through targeted lifestyle adjustments—especially weight management. At iFitCenter, we go beyond basic advice, offering medically supervised programs designed specifically to reduce your cardiovascular and metabolic risks.
Here’s how we help you:
- Comprehensive Metabolic Evaluations: Understand your unique risk profile with advanced assessments.
- Customized Weight Loss Plans: Achieve safe, sustainable fat loss, particularly targeting visceral fat around the abdomen to reduce cardiovascular risk.
- Personalized Nutritional Counseling: Gain practical dietary guidance tailored to improving blood sugar control and protecting your heart.
- Continuous Medical Supervision: Receive regular monitoring to ensure your metabolic health steadily improves.
Your health matters, and your journey towards a healthier heart begins with the right support.
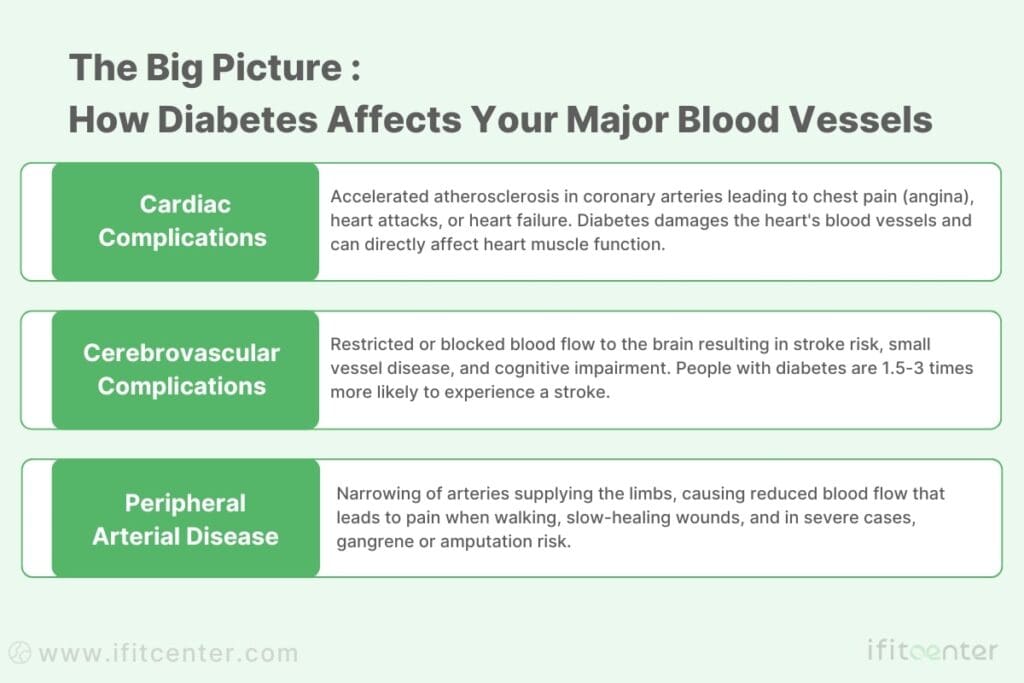
Cardiovascular Disease in Diabetes
Diabetes dramatically increases the risk of various cardiovascular problems. High blood glucose damages the blood vessels and the nerves that control the heart, while the prolonged high insulin levels often seen in type 2 diabetes accelerate the development of atherosclerosis.
Atherosclerosis in diabetes progresses faster for several reasons:
- Glucose-damaged endothelium (the inner lining of blood vessels) more readily traps cholesterol particles
- Inflammation is heightened, promoting plaque formation
- Blood clotting factors are increased, making blockages more likely
- Oxidative stress damages vessels and accelerates plaque buildup
The major types of heart disease common in diabetes include:
- Coronary Artery Disease (CAD): Narrowing of the arteries supplying blood to the heart muscle. This can lead to chest pain (angina), shortness of breath, or heart attack.
- Myocardial Infarction (Heart Attack): People with diabetes are more likely to have silent heart attacks (without obvious symptoms) or atypical symptoms like fatigue or shortness of breath instead of chest pain.
- Heart Failure: Diabetes increases the risk of heart failure—where the heart can’t pump blood effectively—even in the absence of coronary artery disease. This condition, sometimes called “diabetic cardiomyopathy,” results from direct damage to the heart muscle.
The heart-diabetes connection is so significant that heart disease is the leading cause of death among people with diabetes, with cardiovascular mortality rates two to four times higher than in people without diabetes.
“A common misconception I encounter is that once blood sugar, blood pressure, and cholesterol are controlled, cardiovascular risk returns to normal. The research clearly shows this isn’t the case. Even with perfect control of all traditional risk factors, people with diabetes maintain an elevated cardiovascular risk. This is because diabetes affects blood vessels in multiple ways beyond blood sugar alone—through inflammation, oxidative stress, and direct damage to the endothelium. This is why comprehensive cardiovascular assessment is essential even for those with well-controlled diabetes.”
Dr. Babak Jamalian, Family Physician.
Cerebrovascular Disease and Stroke
Cerebrovascular disease affects blood vessels in the brain. Diabetes increases stroke risk through the same mechanisms that damage heart vessels: accelerated atherosclerosis, increased inflammation, and enhanced blood clotting.
People with diabetes face a 1.5 to 3 times higher risk of stroke compared to those without diabetes. Additionally, when strokes occur in people with diabetes, they often have worse outcomes, including higher mortality rates and more significant disability.
Several types of stroke are particularly associated with diabetes:
- Ischemic Stroke: The most common type, caused by a blood clot blocking blood flow to part of the brain. Diabetes significantly increases the risk of this type.
- Lacunar Stroke: Small, deep brain infarcts caused by blockage of small penetrating arteries. These are particularly common in people with diabetes and hypertension.
- Cerebral Small Vessel Disease: Widespread damage to small blood vessels in the brain, which can lead to cognitive impairment and vascular dementia over time.
Beyond acute strokes, diabetes contributes to more gradual forms of brain damage. Chronic small vessel disease in the brain leads to what’s sometimes called “vascular cognitive impairment”—problems with thinking, reasoning, and memory. Over time, these changes can progress to vascular dementia, the second most common form of dementia after Alzheimer’s disease.
Peripheral Arterial Disease
Peripheral arterial disease (PAD) involves narrowing of the arteries that supply blood to the limbs, most commonly the legs. In diabetes, PAD develops earlier, progresses more rapidly, and is often more severe than in people without diabetes.
This reduced blood flow to the limbs can cause varying symptoms depending on severity:
- Intermittent Claudication: Pain, cramping, or fatigue in legs during walking or exercise that goes away with rest. This happens because active muscles aren’t getting enough oxygen-rich blood.
- Rest Pain: As PAD worsens, pain may occur even at rest, especially at night when lying down. This pain often improves when hanging the leg over the edge of the bed (because gravity helps blood flow).
- Critical Limb Ischemia: Severe blockage that leads to persistent pain, non-healing sores or ulcers, and tissue death (gangrene). Without treatment, this can lead to amputation.
What makes PAD particularly dangerous in diabetes is its relationship with neuropathy. Due to nerve damage, many people with diabetes don’t feel the warning pain that would normally signal poor circulation. This “pain-free PAD” often means the condition isn’t discovered until tissue damage is advanced.
PAD creates the perfect conditions for foot complications by reducing blood flow necessary for healing. Even minor injuries can become serious when combined with poor circulation. Modern vascular assessment techniques can detect PAD early, before symptoms develop, allowing for timely intervention to improve blood flow and prevent complications.
Diabetic Foot Complications
Foot problems are among the most serious complications of diabetes. They occur when two main issues combine: nerve damage and poor blood flow to the feet.
This dangerous combination creates several problems:
- No pain warnings: Nerve damage means you may not feel injuries
- Poor healing: Reduced blood flow means wounds heal slowly
- Foot deformities: Nerve damage can change foot shape, creating pressure points
- Dry, cracked skin: Creates openings for infection
Diabetic foot ulcers are open sores that typically form on the bottom of the foot. They start with minor injuries that go unnoticed and worsen due to continued pressure and poor healing.
Charcot foot is a condition where the bones weaken and deform. Because of nerve damage, a person may walk on broken bones without feeling pain, causing severe deformity over time.
Infections develop easily in diabetic feet and spread quickly. Poor circulation means fewer infection-fighting cells reach the area, while high blood sugar provides fuel for bacteria to grow.
In severe cases, tissue death (gangrene) can occur when blood supply is completely cut off. This may lead to amputation if the infection cannot be controlled with antibiotics.
Acute Complications of Diabetes
Unlike long-term complications, acute complications develop quickly—sometimes within hours. They can be life-threatening if not treated promptly.
To access the second part of the articles related to diabetes, you can use the following links:
- The Difference Between Prediabetes and Diabetes
- Insulin Resistance and Diabetes
- Understanding Blood Sugar Numbers
- Weight Loss for Type 2 Diabetes
- Best Fruits for Diabetic Patients
Diabetic Ketoacidosis (DKA)
Diabetic ketoacidosis occurs when the body has too little insulin. Without insulin, cells cannot use glucose for energy, so the body burns fat rapidly instead, producing acidic substances called ketones.
DKA mainly affects people with type 1 diabetes. Common triggers include:
- Missing insulin doses
- Illness or infection
- Newly diagnosed diabetes
- Severe stress
Warning signs of DKA include:
- Extreme thirst and frequent urination
- Nausea and vomiting
- Stomach pain
- Fruity-smelling breath
- Confusion
- High blood sugar levels
DKA is dangerous because it makes the blood too acidic, causing severe dehydration and disrupting essential body functions. Without treatment, it can lead to coma or death.
Hyperosmolar Hyperglycemic State (HHS)
Hyperosmolar hyperglycemic state is characterized by extremely high blood sugar and severe dehydration. Unlike DKA, it doesn’t produce many ketones because some insulin is still present.
HHS primarily affects older adults with type 2 diabetes. Main differences from DKA include:
- Much higher blood sugar levels
- More severe dehydration
- Few or no ketones
- Slower development (days rather than hours)
Common triggers include infections, inadequate fluid intake, and certain medications. Symptoms include extreme thirst, confusion, and weakness.
The extreme dehydration in HHS is particularly dangerous. It concentrates the blood, which can cause brain cells to shrink and lead to seizures or coma.
Hypoglycemia
Hypoglycemia means low blood sugar. It’s common in people who take insulin or certain diabetes medications. Blood sugar below 70 mg/dL is generally considered low.
Common causes of hypoglycemia include:
- Too much diabetes medication
- Not eating enough or skipping meals
- Unexpected exercise
- Alcohol consumption
Hypoglycemia produces three levels of symptoms:
- Early signs: Hunger, shakiness, sweating, anxiety
- Worsening signs: Difficulty thinking, confusion, weakness
- Severe signs: Seizures, unconsciousness
A dangerous aspect of hypoglycemia is that repeated episodes can cause “hypoglycemia unawareness.” This means the body stops giving warning signals when blood sugar drops, increasing the risk of severe episodes.
Other Complications of Diabetes
Diabetes affects many parts of the body beyond the well-known complications. The skin, mouth, and digestive system can all develop problems that affect daily life and comfort.
Skin Complications of Diabetes
Skin problems are among the first visible signs of diabetes. High blood sugar provides an ideal environment for infections and affects blood flow to the skin.
Common skin infections include bacterial infections like styes and boils, and fungal infections such as athlete’s foot and ringworm. These infections often occur repeatedly and heal slowly in people with diabetes.
Diabetic dermopathy appears as light brown, scaly patches, often on the shins. These “shin spots” are harmless but very common in diabetes. They result from minor injury to the skin combined with changes in small blood vessels.
Necrobiosis lipoidica diabeticorum causes raised, reddish-yellow patches with a shiny porcelain-like appearance. These patches can be itchy or painful and may eventually open up as sores.
Acanthosis nigricans produces dark, velvety skin patches in body folds, particularly around the neck and armpits. It’s strongly linked to insulin resistance and often appears before diabetes is diagnosed.
Diabetic blisters (bullosis diabeticorum) are painless, fluid-filled blisters that appear suddenly, usually on the feet and legs. They look like burn blisters but occur without injury.
Digital sclerosis causes thickening of the skin on the hands and fingers, making them stiff and waxy. This condition can limit finger movement and dexterity.
Oral and Dental Complications of Diabetes
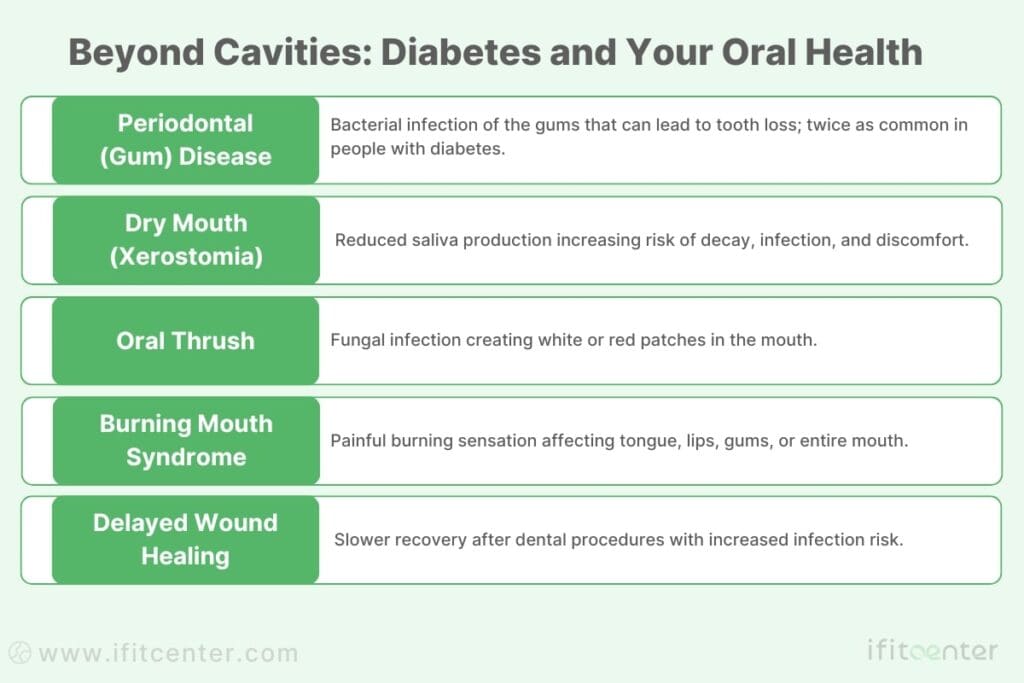
Diabetes affects oral health through reduced saliva flow, increased sugar in saliva, and impaired healing abilities. These changes create an environment where oral problems flourish.
Periodontal (gum) disease is significantly more common in people with diabetes. High blood sugar weakens the body’s ability to fight bacteria, allowing gum infections to develop more easily. These infections then make blood sugar control more difficult, creating a vicious cycle.
Dry mouth (xerostomia) occurs when salivary glands don’t produce enough saliva. This creates discomfort and increases risk for tooth decay and oral infections since saliva helps wash away food particles and neutralize acids.
Oral candidiasis (thrush) is a fungal infection causing white or red patches in the mouth. People with diabetes are more susceptible to this infection, especially when blood sugar is poorly controlled.
Burning mouth syndrome creates a painful burning sensation affecting the tongue, lips, gums, palate, throat or whole mouth. It’s more common in people with diabetes, particularly women.
Dental healing issues are common in diabetes. After dental procedures, healing may take longer and infection risk increases. This is why it’s important to inform your dentist about your diabetes before any procedure.
Digestive Complications of Diabetes
Diabetes can damage the nerves that control the digestive system, leading to various gastrointestinal problems that affect quality of life.
Diabetic gastroparesis occurs when nerve damage affects the stomach muscles, slowing or stopping the movement of food. This delayed emptying causes symptoms like nausea, vomiting, feeling full quickly, and unpredictable blood sugar levels since food is absorbed at irregular times.
Fatty liver disease is more common in people with diabetes, particularly those who are overweight. In this condition, fat builds up in liver cells, potentially leading to liver inflammation and scarring. Many people have no symptoms until the disease is advanced.
Other digestive effects include constipation or diarrhea due to nerve damage affecting the intestines. Some people experience alternating bouts of both problems. Trouble swallowing, heartburn, and abdominal pain may also occur due to effects on the esophagus and other digestive organs.
Sexual and Urological Complications of Diabetes
Diabetes can affect sexual health and urinary function through damage to nerves and blood vessels that control these systems. These complications are common but often not discussed due to embarrassment.
Erectile dysfunction (ED) is very common in men with diabetes. It occurs when diabetes damages blood vessels and nerves needed for an erection. The problem may develop gradually, with partial erections before complete ED occurs. Unlike occasional difficulties that all men experience, diabetic ED tends to be persistent and worsen over time if blood sugar remains uncontrolled.
Women with diabetes also experience sexual problems, including reduced sensation, vaginal dryness, painful intercourse, and decreased desire. These issues stem from nerve damage, reduced blood flow, and hormonal changes related to diabetes. Vaginal infections, more common in diabetes, can further complicate sexual health.
Bladder dysfunction occurs when diabetes damages nerves that control the bladder. This condition, called diabetic cystopathy, can cause the bladder to not empty completely or lose the sensation of fullness. People may not feel the urge to urinate until the bladder is very full, or may not be able to tell when it’s empty.
Urinary tract infections and incontinence occur more frequently in people with diabetes. Poor bladder emptying leaves urine in the bladder longer, allowing bacteria to grow. High sugar levels in urine also create an ideal environment for bacterial growth. Nerve damage can cause unexpected leakage or inability to control urination.
Neurological Complications of Diabetes
Diabetes affects the brain and nervous system beyond the peripheral neuropathy discussed earlier. These neurological effects can impact thinking, mood, and overall quality of life.
Cognitive impairment ranges from subtle changes in memory and thinking speed to more serious conditions like dementia. Diabetes impacts the brain through reduced blood flow, inflammation, and direct effects of high blood sugar on brain cells. Some researchers refer to Alzheimer’s disease as “Type 3 diabetes” due to the strong connection between insulin resistance and brain function.
Depression is twice as common in people with diabetes compared to those without the condition. This goes beyond feeling sad about having a chronic condition. Diabetes affects brain chemistry directly, while the stress of managing a complex disease adds psychological burden. Depression makes diabetes self-care more difficult, creating a cycle where each condition worsens the other.
Diabetes distress describes the emotional burden of managing diabetes day after day. It includes feelings of overwhelm, failure, and burnout specifically related to diabetes care. This condition is different from clinical depression but can significantly impact quality of life and diabetes management.
Sleep disorders are more common in diabetes, including insomnia, sleep apnea, and restless legs syndrome. Poor sleep then makes blood sugar control more difficult, creating another harmful cycle. Nerve damage, pain, frequent urination at night, and blood sugar fluctuations all contribute to sleep problems.
Musculoskeletal Complications of Diabetes
Diabetes affects joints, muscles, and connective tissues throughout the body. These musculoskeletal complications can limit movement and cause significant pain.
Limited joint mobility syndrome, also called diabetic hand syndrome or cheiroarthropathy, causes thickening of the skin and tissues around joints. The hands are most commonly affected, with tight, waxy skin that limits finger movement. People may be unable to press their palms flat against each other in a “prayer position” – a simple test for this condition.
Frozen shoulder (adhesive capsulitis) involves pain and stiffness in the shoulder joint, eventually leading to severely restricted movement. While frozen shoulder can occur in anyone, it’s much more common in people with diabetes. It typically develops slowly, with gradually increasing pain and stiffness over months or years.
Dupuytren’s contracture causes thick, tough tissue to form under the skin of the palm. This tissue gradually tightens, pulling one or more fingers into a bent position that cannot be straightened. Though not painful, it can severely limit hand function. Diabetes increases the risk of developing this condition.
Carpal tunnel syndrome occurs when a nerve in the wrist is compressed, causing numbness, tingling, and weakness in the hand and fingers. Diabetes increases the risk by causing swelling of tissues in the wrist or damage to the nerve itself.
Diabetic muscle infarction is a rare but serious complication where blood flow to a muscle (usually in the thigh) is suddenly blocked, causing severe pain and swelling. This painful condition often resolves on its own over weeks or months but may recur in the same or different muscles.
Other Systemic Complications of Diabetes
Beyond the well-known complications, diabetes affects several other body systems in ways that can significantly impact health and quality of life.
Respiratory Complications of Diabetes
Diabetes affects lung function and respiratory health in ways that aren’t widely recognized. These changes can make breathing more difficult and increase vulnerability to respiratory illnesses.
Pulmonary function gradually declines in people with diabetes. High blood sugar damages lung tissue and blood vessels similar to how it affects other organs. This can reduce lung capacity and make breathing less efficient, especially during physical activity. Many people notice shortness of breath with exertion before other lung symptoms develop.
Sleep apnea is strongly linked to diabetes. This condition causes breathing to stop briefly during sleep, sometimes hundreds of times per night. The connection works both ways – diabetes increases sleep apnea risk, while sleep apnea makes blood sugar control more difficult. Symptoms include loud snoring, gasping during sleep, morning headaches, and daytime sleepiness.
People with diabetes face higher risks from respiratory infections like pneumonia and bronchitis. High blood sugar impairs immune function, making it harder to fight off infections. When respiratory infections do occur, they often last longer and cause more complications in people with diabetes.
Hematologic Complications of Diabetes
Diabetes affects blood cells and clotting factors, creating changes that impact how the body responds to injury and infection.
Immune function becomes impaired when diabetes is present, especially when blood sugar is poorly controlled. White blood cells, which fight infection, don’t work as effectively in a high-sugar environment. They move more slowly to infection sites and have reduced ability to kill bacteria. This explains why infections are both more common and more severe in people with diabetes.
Wound healing is altered in diabetes through multiple mechanisms. Beyond reduced blood flow to tissues, diabetes affects the activity of growth factors and specialized cells needed for proper healing. The normal sequence of inflammation, tissue formation, and remodeling becomes disrupted. Even minor wounds may heal slowly or incompletely.
Blood clotting changes make both excessive clotting and bleeding more likely in diabetes. Platelets (cells involved in clotting) become more sticky and prone to forming clots, increasing risk for heart attack and stroke. Yet paradoxically, abnormal clotting proteins can also increase bleeding risk in some situations. This complex balance helps explain the diverse circulatory complications seen in diabetes.
Hearing and Balance Complications of Diabetes
The inner ear’s delicate structures depend on good blood flow and nerve function – both affected by diabetes. These changes can impact both hearing and the sense of balance.
Hearing loss occurs more frequently in people with diabetes, developing gradually and affecting both ears equally. The condition typically affects ability to hear higher frequencies first. Many people don’t notice the early changes because the brain adapts to gradually declining hearing. Diabetes damages both the inner ear’s tiny blood vessels and the auditory nerve, creating a double impact on hearing function.
Vertigo and dizziness occur more often in diabetes due to effects on the vestibular system – the part of the inner ear responsible for balance. These symptoms may range from mild unsteadiness to severe spinning sensations that make it difficult to stand or walk. Sudden position changes often trigger symptoms, which may last from seconds to hours.
Inner ear dysfunction in diabetes extends beyond hearing loss and balance problems. Tinnitus (ringing in the ears) and a sense of fullness or pressure in the ears are also more common. These symptoms can be distressing and may interfere with concentration, communication, and overall quality of life.
Type 1 vs Type 2 Diabetes Complications
While both types of diabetes can lead to similar complications, there are important differences in how and when these problems develop. Understanding these patterns helps with appropriate monitoring and care.
Type 1 and Type 2 diabetes share many complication pathways. Both conditions damage blood vessels and nerves through extended periods of high blood sugar. This means the major complications—retinopathy, nephropathy, neuropathy, and cardiovascular disease—can occur in either type.
The time course of complications differs significantly between types. In Type 1 diabetes, complications typically develop after 5-10 years of disease, even with good control. Since Type 1 often begins in childhood or adolescence, serious complications may appear when patients are in their 20s or 30s. In Type 2 diabetes, complications might already be present at diagnosis since many people have had undiagnosed diabetes for years before detection.
Type 1 diabetes brings unique considerations regarding complications. The lifelong exposure to diabetes means that even with excellent control, complications may eventually develop simply due to the duration of the disease. Fluctuating blood sugar levels with insulin therapy can also create distinct challenges, particularly with hypoglycemia risk.
Type 2 diabetes often occurs alongside other conditions like obesity, high blood pressure, and abnormal cholesterol levels. This “metabolic syndrome” cluster accelerates complication development and makes management more complex. Additionally, older age at onset means complications may interact with age-related health issues.
Specialized complication risk assessments can identify early warning signs before obvious symptoms appear. These comprehensive evaluations look for subtle changes in nerve function, kidney performance, and eye health that might otherwise go unnoticed, allowing for earlier intervention.
Serious Long-Term Complications of Diabetes
While all diabetes complications warrant attention, some pose immediate threats to life or can severely impact independence and quality of life. Understanding these serious complications helps emphasize the importance of prevention.
Life-threatening complications of diabetes include:
- Heart attack and stroke: Cardiovascular events remain the leading cause of death among diabetic patients
- Kidney failure: Advanced kidney disease requires dialysis or transplantation for survival
- Severe infections: Diabetic foot infections can lead to systemic infection (sepsis)
- Acute metabolic crises: DKA and HHS have significant mortality rates if not treated promptly
Several warning signs require immediate medical attention:
- Chest pain, jaw pain, or shortness of breath
- Sudden weakness, numbness, confusion, or severe headache
- Foot ulcers that show signs of infection (redness, warmth, drainage)
- Persistent vomiting, abdominal pain, or fruity-smelling breath
- Vision changes that develop rapidly
Complications rarely occur in isolation. Instead, they interconnect and worsen each other. For example, kidney disease accelerates heart disease, while neuropathy increases fall risk, which can be catastrophic for someone with osteoporosis. This interconnection means that developing one complication significantly increases the risk for others.
When multiple complications are present, overall health declines more rapidly than with individual problems. Daily activities become increasingly difficult, independence may be threatened, and treatment becomes more complex. For example, a person with vision loss from retinopathy, pain from neuropathy, and reduced mobility from heart disease faces compounded challenges in daily life.
Conclusion
Diabetes complications affect virtually every system in the body, from the smallest blood vessels in the eyes to the largest arteries supplying the heart. These complications develop gradually when blood sugar remains elevated over time, often without obvious symptoms until significant damage has occurred.
The major categories of complications include:
- Microvascular complications: Affecting the eyes (retinopathy), kidneys (nephropathy), and nerves (neuropathy)
- Macrovascular complications: Affecting the heart, brain, and limbs through accelerated atherosclerosis
- Acute complications: Including diabetic ketoacidosis, hyperosmolar hyperglycemic state, and hypoglycemia
- Other systemic complications: Affecting the skin, mouth, digestive system, urinary system, musculoskeletal system, and more
While diabetes complications are serious, understanding them is the first step toward prevention. Early detection through comprehensive complication assessments can identify problems when they’re most treatable. These thorough evaluations check for early signs of complications before they cause symptoms or irreversible damage.
Awareness of potential complications isn’t meant to frighten but to empower. With proper management and regular monitoring, many people with diabetes live long, healthy lives without developing serious complications. Knowledge about these potential problems helps reinforce the importance of blood sugar control, regular medical care, and healthy lifestyle choices in protecting long-term health.
Frequently Asked Questions About Diabetes Complications
What are the most common complications of diabetes?
The most common complications include retinopathy (eye damage), nephropathy (kidney damage), neuropathy (nerve damage), and cardiovascular disease (heart and blood vessel damage).
What’s the difference between microvascular and macrovascular complications?
Microvascular complications affect small blood vessels and include problems with the eyes, kidneys, and nerves. Macrovascular complications affect large blood vessels and include heart disease, stroke, and peripheral artery disease.
Can diabetes complications be reversed?
Some early complications can improve with better blood sugar control. However, many advanced complications cause permanent damage that can’t be reversed, though treatment may prevent further progression.
How quickly do diabetes complications develop?
The timeline varies greatly. Some complications may develop within months of poorly controlled diabetes, while others take many years. Regular screening is important even when you feel fine.
Are complications of diabetes type 1 different from type 2?
Both types can lead to similar complications, but the timeline and risk factors differ. Type 1 complications typically develop after several years of disease, while Type 2 complications may be present at diagnosis due to years of undetected high blood sugar.
To access other content on the IFitCenter’s blog, you can use the following links:
References for Diabetes Complications
- American Diabetes Association. The American Diabetes Association Releases Standards of Care in Diabetes—2025. December 9, 2024, Arlington, VA. DOI: 10.2337/dc25-SOC
- Huh, Ji Hye, Kwon, Serim, Kim, Gui Ok, Kim, Bo Yeon, Ha, Kyoung Hwa, & Kim, Dae Jung. Long-term Effectiveness of the National Diabetes Quality Assessment Program in South Korea. Diabetes Care, 2023; 46(9): 1700–1706. DOI: 10.2337/dc23-0444
- Młynarska, Ewelina, Czarnik, Witold, Dzięża, Natasza, Jędraszak, Weronika, Majchrowicz, Gabriela, Prusinowski, Filip, Stabrawa, Magdalena, Rysz, Jacek, & Franczyk, Beata. Type 2 Diabetes Mellitus: New Pathogenetic Mechanisms, Treatment and the Most Important Complications. International Journal of Molecular Sciences, 2025; 26(3): 1094. DOI: 10.3390/ijms26031094
- Kibirige D, Chamba N, Andia-Biraro I, et al, Indicators of optimal diabetes care and burden of diabetes complications in Africa: a systematic review and meta-analysis, DOI: 10.1136/bmjopen-2022-060786
- Tan, Michelle Hwee Pheng, Ong, Siew Chin, Bujang, Mohamad Adam, Shah, Shamsul Azhar, & Mustafa, Norlaila. Evaluation of the Health-Related Quality of Life of Patients with Type 2 Diabetes in Relation to Macrovascular and Microvascular Complications. Acta Diabetologica, 2023; 60(12): 1735–1747. DOI: 10.1007/s00592-023-02164-2



