Type 2 diabetes is often surrounded by misconceptions: “Only overweight people get diabetes,” or “You’ll definitely develop diabetes if you eat too many sweets.” While obesity and diet do play roles, the reality of type 2 diabetes is far more complex. Understanding the true causes, recognizing subtle symptoms early, and implementing practical management strategies can dramatically improve your health.
In this comprehensive guide from Weight loss clinic, we’ll explore the true causes of type 2 diabetes, identify symptoms that often go unnoticed, and present effective strategies you can immediately apply to manage—and potentially reverse—the condition. Gaining clarity on diabetes empowers you to take control of your health and live better.
Understanding Type 2 Diabetes: What Is Type 2 Diabetes?
Type 2 diabetes is a chronic health condition in which your body either doesn’t produce enough insulin or doesn’t effectively use the insulin it produces—known as insulin resistance. Think of insulin as a key that unlocks your cells, allowing sugar (glucose) to enter and provide energy. With type 2 diabetes, your cells don’t respond properly to insulin, causing sugar to accumulate in your blood instead of fueling your body. This excess sugar buildup can eventually lead to serious health complications like heart disease, kidney damage, or nerve damage.
Who’s at risk for type 2 diabetes?
While it can affect anyone, certain factors significantly raise your risk, including being overweight, leading a sedentary lifestyle, and having a family history of diabetes. According to a comprehensive systematic review published in the World Journal of Diabetes, factors such as obesity, physical inactivity, poor sleep quality, smoking, and certain ethnic backgrounds significantly increase the risk of developing type 2 diabetes. For instance, diabetes prevalence is notably higher among Pacific Islanders, Blacks, Native Americans, Hispanics, and those with a family history of diabetes.
Recognizing these risk factors early is vital because type 2 diabetes often progresses silently, showing minimal or no symptoms for years. Awareness and timely action can make a substantial difference in prevention or effective management of this condition.
Insulin Resistance: The Core Cause of Type 2 Diabetes
The primary driver behind type 2 diabetes is insulin resistance, a condition where the body’s cells no longer respond properly to insulin. Imagine insulin as a courier delivering essential fuel (glucose) to your body’s cells. Insulin resistance is like having faulty locks on your cell doors, causing insulin’s keys to fail, leaving glucose trapped in your bloodstream instead of entering cells. Over time, your pancreas tries to compensate by producing more insulin, but eventually, it becomes overwhelmed, leading to persistently elevated blood sugar levels and ultimately, type 2 diabetes.
Overcome Insulin Resistance by Achieving a Healthy Weight
Type 2 diabetes develops when your body becomes resistant to insulin, often due to excess weight and lifestyle factors. The good news is that weight loss can significantly improve insulin sensitivity, helping your body regulate blood sugar levels naturally.
At iFitCenter, we offer medically supervised weight management programs specifically designed to address insulin resistance and support sustainable, healthy weight loss. Through personalized nutritional plans and comprehensive metabolic evaluations, we help you regain control of your glucose metabolism and protect your long-term health.
Take your first step towards overcoming insulin resistance today.
What Increases Your Risk for Insulin Resistance?
Several key factors contribute to insulin resistance. Obesity is among the most influential. Excess body fat, particularly visceral fat (the deep belly fat surrounding organs), interferes with insulin’s effectiveness. However, genetics also play a significant role. Even individuals with a healthy weight can develop type 2 diabetes if there’s a strong family history or genetic predisposition.
How Lifestyle Choices Increase Diabetes Risk
Environmental and lifestyle factors heavily influence your risk. Lack of regular physical activity reduces your muscles’ sensitivity to insulin, making it harder for glucose to enter cells effectively. Poor dietary habits, particularly frequent consumption of processed carbohydrates and sugary foods, consistently spike insulin, further driving resistance. insulin resistance emerges primarily from chronic carbohydrate overload, making dietary adjustments crucial for prevention and treatment.
The Surprising Role of Sleep and Stress
Poor sleep—both insufficient sleep and disrupted sleep patterns—is increasingly linked to higher diabetes risk. A comprehensive systematic review published in the World Journal of Diabetes found that sleeping fewer than six or more than nine hours daily significantly increases diabetes risk due to its negative impacts on insulin sensitivity and hormone regulation. Likewise, chronic stress raises cortisol levels, further contributing to insulin resistance and obesity.
On the IFitCenter blog, we have provided a comprehensive guide for diabetes, completely free of charge and based on the latest research. By viewing these articles, in addition to increasing your general knowledge in this field, you can easily manage this disease in a principled manner. To access the first part of the articles, simply use the links below:
- What is Diabetes?
- Symptoms and Signs of Diabetes
- Difference Between Type 1 and Type 2 Diabetes
- What Are the Complications of Diabetes?
- Diabetes Diagnosis Method
- Worst fruits for diabetes
- How to take apple cider vinegar to lower blood glucose
Gut Health and Diabetes: A Crucial Connection
Emerging research highlights that a disrupted gut microbiome significantly contributes to insulin resistance and type 2 diabetes. A healthy gut microbiome, rich in beneficial bacteria such as Akkermansia muciniphila and Faecalibacterium prausnitzii, helps maintain insulin sensitivity and reduce inflammation. A 2022 comprehensive review published in the International Journal of Molecular Sciences highlights that individuals with type 2 diabetes often show reduced levels of these beneficial bacteria, contributing to disease progression and complications.
Identifying Symptoms for Type 2 Diabetes: Recognizing Early Warning Signs

Recognizing early symptoms of type 2 diabetes can help you intervene before complications arise. Many early signs are subtle, making them easy to overlook. Common initial symptoms include frequent urination, excessive thirst, unexplained tiredness, blurred vision, and slow-healing wounds. These occur as elevated blood sugar begins affecting different parts of your body, signaling the early stages of diabetes development.
“Many people mistakenly believe that type 2 diabetes always presents clear and obvious symptoms, such as excessive thirst or frequent urination. However, subtle indicators—like skin tags or dark patches on the skin—often emerge much earlier and could indicate underlying insulin resistance. Recognizing these hidden symptoms early can significantly change your management strategies and reduce long-term health risks.”
Dr. Babak Jamalian, Family Physician.
Skin Signs You Shouldn’t Ignore
your skin can provide important clues about diabetes. For instance, if you notice dark, velvety patches on areas such as your neck, armpits, or groin, you might have a condition called acanthosis nigricans. These patches are typically a sign of insulin resistance. Likewise, skin tags—small, benign skin growths appearing around skin folds—can also indicate elevated insulin levels. Another skin-related sign, known as diabetic dermopathy, appears as darkened, bruise-like patches typically found on the lower legs. These skin symptoms, although not painful, signal insulin resistance and should prompt you to seek medical advice.
How to Conduct a Practical Self-Assessment
If you’re concerned you might have type 2 diabetes, you can start by asking yourself a few key questions:
- Am I frequently thirsty, even after drinking sufficient water?
- Do I feel unusually tired or lethargic throughout the day?
- Have I experienced sudden changes in my vision?
- Do wounds or cuts heal noticeably slower than before?
- Have new skin conditions appeared, such as darkened patches or numerous skin tags?
If you answered “yes” to several of these questions, it may be beneficial to undergo a diabetes screening. Early detection can significantly improve your health outcomes and prevent further complications.
Type 2 Diabetes Complications: Why Early Screening Matters
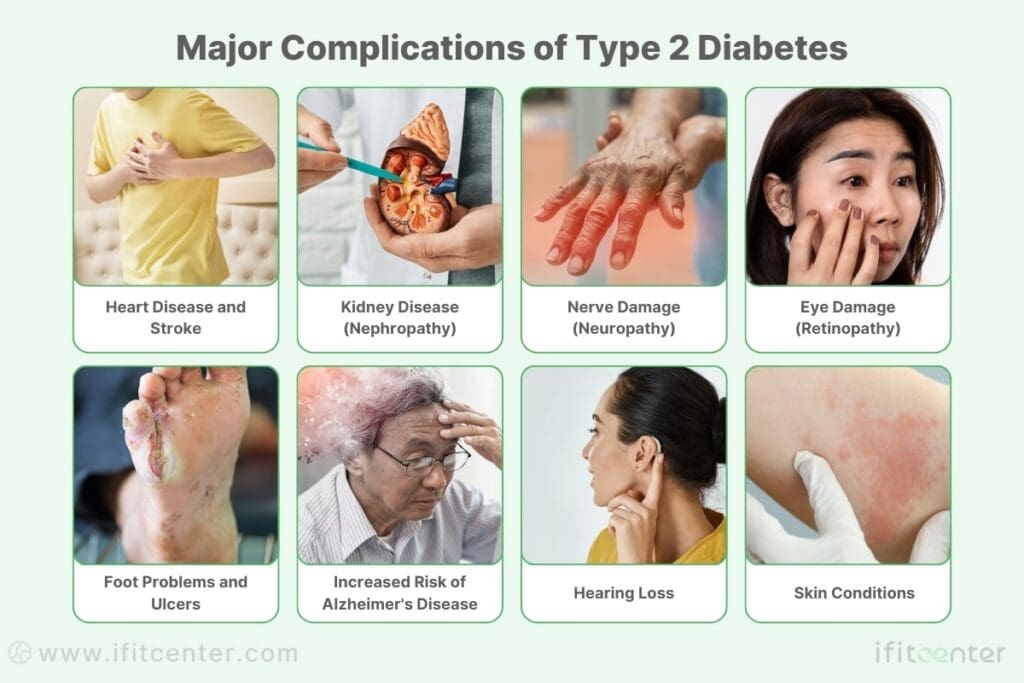
Type 2 diabetes, if left unmanaged, can quietly cause severe complications, including kidney disease, nerve damage, and cardiovascular problems. Diabetic nephropathy, a form of kidney damage caused by diabetes, initially shows no noticeable symptoms. Over time, persistent high blood sugar damages delicate structures within the kidneys, reducing their filtering capacity. Similarly, diabetes-induced nerve damage, or diabetic neuropathy, can lead to numbness, tingling, or burning sensations, particularly in hands and feet. Cardiovascular complications, such as increased risks of heart disease and stroke, arise due to prolonged high glucose and insulin resistance damaging blood vessels.
Advanced Biomarkers for Early Detection
Early detection of these complications significantly improves management and prevention strategies. Recent scientific research, specifically a detailed review published in Frontiers in Physiology, emphasizes innovative biomarkers like SMAD1, Podocalyxin, NGAL (Neutrophil gelatinase-associated lipocalin), Netrin-1, and L-FABP (liver-type fatty acid-binding protein). These biomarkers can identify kidney damage even before conventional tests detect abnormalities. For instance, elevated levels of Neutrophil gelatinase-associated lipocalin (NGAL) or Netrin-1 in urine indicate early kidney injury, long before traditional markers like albumin reveal a problem (DOI: 10.3389/fphys.2022.1020443).
Incorporating advanced biomarker testing into routine diabetes care allows healthcare providers to proactively intervene, preventing progression to severe kidney disease and associated cardiovascular risks.
Tests to Diagnose Type 2 Diabetes
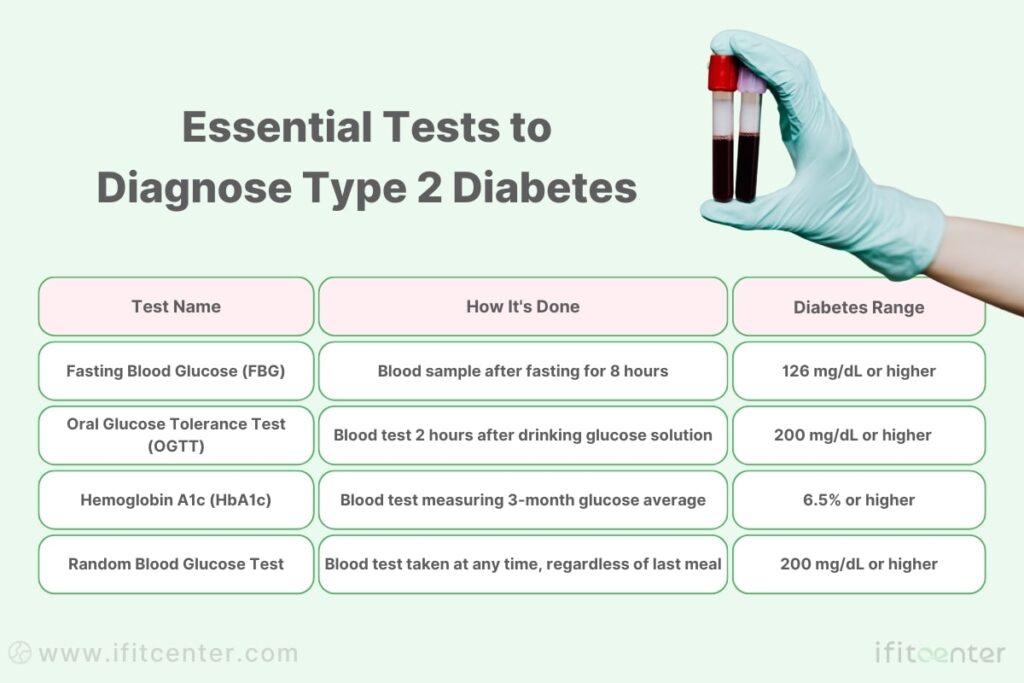
Diagnosing type 2 diabetes typically involves a combination of specific laboratory tests designed to measure blood sugar levels and how effectively your body manages glucose. The most common tests include fasting blood glucose (FBG), Oral Glucose Tolerance Test (OGTT), and the Hemoglobin A1c (HbA1c) test.
Fasting Blood Glucose Test
This test measures blood sugar after fasting for at least 8 hours. Normally, your body maintains glucose within a certain range, but consistently high fasting glucose levels may indicate diabetes. An FBG reading equal to or greater than 126 mg/dL on two separate occasions confirms diabetes. A reading between 100 and 125 mg/dL indicates prediabetes or insulin resistance, which signifies an increased risk of progressing to type 2 diabetes.
Oral Glucose Tolerance Test (OGTT)
The OGTT involves drinking a glucose-rich beverage after an overnight fast. Blood sugar is then measured at intervals, typically two hours after consumption. A two-hour glucose level of 200 mg/dL or higher confirms diabetes, while readings between 140 and 199 mg/dL suggest impaired glucose tolerance, another sign of prediabetes.
Hemoglobin A1c (HbA1c) Test
The HbA1c test measures your average blood sugar levels over approximately three months, offering a broader picture of your glucose management. An HbA1c result of 6.5% or higher indicates diabetes. Levels between 5.7% and 6.4% are indicative of prediabetes, highlighting the need for preventive action through lifestyle changes.
To access the second part of the articles related to diabetes, you can use the following links:
- Is Diabetes Curable?
- Type 1 Diabetes Explained
- Relationship Between Diabetes and Obesity
- Causes of Diabetes
- Weight Loss for Type 2 Diabetes
- can diabetics drink whiskey?
Distinguishing Type 2 Diabetes from Type 1 Diabetes
Sometimes, healthcare providers must differentiate between type 2 diabetes and type 1 diabetes. A useful test in these cases is the C-peptide test, which measures the level of a byproduct released when insulin is produced. In type 2 diabetes, your body typically continues to produce insulin initially, resulting in normal or elevated C-peptide levels. Conversely, individuals with type 1 diabetes show significantly reduced or absent C-peptide levels due to the autoimmune destruction of insulin-producing beta cells in the pancreas.
If you have concerns about your blood sugar levels or believe you might be at risk, consult your healthcare provider for these tests to obtain an accurate assessment of your glucose metabolism.
Practical Lifestyle Management Strategies for Type 2 Diabetes
Managing type 2 diabetes effectively involves more than medication—it requires practical lifestyle strategies that directly address insulin resistance. Among these strategies, nutritional management and diet therapy have emerged as particularly effective solutions. Adopting evidence-based dietary approaches can significantly improve insulin sensitivity, enhance energy levels, and reduce diabetes-related complications, enabling individuals to lead healthier, more active lives.
Nutritional Management and Diet Therapy: The Ketogenic Diet and Intermittent Fasting
The ketogenic diet and intermittent fasting have gained popularity for their effectiveness in addressing type 2 diabetes at its root cause—insulin resistance. ketogenic diet, which involves reducing carbohydrate intake and increasing healthy fats, directly lowers insulin levels, allowing your body to use fat as its primary energy source instead of glucose. This approach helps your body regain sensitivity to insulin, effectively improving blood sugar control.
Intermittent fasting complements this dietary approach by restricting your eating to specific time windows, providing periods when insulin production is minimal. This practice can be as simple as skipping breakfast and limiting meals to an eight-hour period during the day. According to Dr. Sarah Hallberg, reducing carbohydrate intake not only stabilizes blood sugar but also helps decrease hunger and cravings, making dietary changes sustainable long-term.
Effective Physical Activity for Type 2 Diabetes: Practical Exercise Guidelines
Regular physical activity is an essential part of managing type 2 diabetes effectively, especially due to its proven ability to improve insulin sensitivity. Structured exercises like resistance training and walking offer significant benefits, helping your muscles better absorb glucose and reducing the demand on your pancreas.
Resistance Training: Building Muscle for Better Blood Sugar Control
A systematic review published in Frontiers in Endocrinology highlights the substantial benefits of resistance training for managing type 2 diabetes. Engaging in strength training exercises, such as lifting weights or using resistance bands, helps muscles use glucose more efficiently, thereby directly reducing insulin resistance (DOI: 10.3389/fendo.2023.1224161).
To gain maximum benefits, the following guidelines are recommended:
- Duration: Follow a structured program for 12 to 16 weeks.
- Frequency: Aim for 2-3 resistance training sessions per week.
- Intensity and Repetitions: Perform each exercise at 70-80% of your maximum ability, completing 8-10 repetitions per set.
Effective Walking Guidelines for Diabetes Management
Walking is a practical, accessible exercise that significantly supports diabetes management. A recent study published in the British Journal of Sports Medicine (BJSM) emphasizes that regular moderate-paced walking can improve insulin sensitivity and metabolic health. Walking at a comfortable yet brisk pace (around 4 to 6 km/hour) ensures an optimal balance, benefiting glucose regulation without overexertion.
By consistently incorporating these exercises into your weekly routine, you can effectively improve your diabetes control and overall health. Before starting any new exercise program, it’s beneficial to consult your healthcare provider or an exercise specialist to personalize your regimen.
Comprehensive Management of Diabetes Complications: Protect Your Long-Term Health
Effectively managing type 2 diabetes goes beyond blood sugar control—it also involves addressing associated complications such as cardiovascular disease, diabetic nephropathy (kidney damage), and neuropathy. Consistently maintaining optimal glucose levels, cholesterol, and blood pressure is essential to reducing these serious risks, as prolonged high blood sugar can damage blood vessels, nerves, and organs.
According to a detailed systematic review on diabetes complications (DOI: 10.3389/fphys.2022.1020443), early detection of kidney damage through advanced biomarkers and routine assessments significantly improves outcomes. Similarly, specialists like Dr. Tom Biernacki emphasize the critical role of early intervention to prevent foot ulcers and neuropathy, highlighting the importance of regular screenings and proactive care.
A comprehensive diabetes management plan involves regular medical check-ups with healthcare professionals from various specialties, including podiatrists, cardiologists, and nephrologists. Regular eye exams, diabetic retinopathy screening and foot assessments help identify complications like diabetic retinopathy and diabetic neuropathy at their earliest stages, enabling timely treatment and preventing further damage.
“A common misconception about diabetes complications is that they only appear when blood sugar reaches very high levels. In reality, conditions like kidney damage and neuropathy can start silently, even before conventional blood tests show elevated sugar levels. Early detection through regular screenings and monitoring can provide patients with a substantial advantage in preventive care.”
Dr. Babak Jamalian, Family Physician.
Is Type 2 Diabetes Curable? Exploring the Truth About Diabetes Type 2 Cure
The question of whether type 2 diabetes can be permanently cured is often debated. While there’s currently no guaranteed permanent cure, type 2 diabetes can certainly be reversed or placed into remission with effective management. Remission means achieving normal blood sugar levels without relying on diabetes medication, often maintained through consistent lifestyle adjustments such as diet changes and increased physical activity.
reversing type 2 diabetes involves addressing insulin resistance, primarily by significantly reducing carbohydrate intake and adopting intermittent fasting practices. However, it’s important to understand that remission is maintained as long as these lifestyle modifications continue. Returning to previous dietary or lifestyle habits can bring diabetes back.
Treatments and Strategies for Controlling Type 2 Diabetes
Although there’s no guaranteed cure, numerous treatments can effectively manage type 2 diabetes, preventing complications and improving quality of life. Common treatments include:
- Lifestyle Changes: Dietary modifications, weight management, and regular physical activity are foundational strategies.
- Oral Medications: Drugs such as metformin improve insulin sensitivity and help regulate blood sugar.
- Insulin Therapy: Some patients may eventually require insulin injections if their pancreas can no longer produce sufficient insulin.
Adopting personalized treatment strategies, based on professional medical guidance, ensures optimal diabetes management and significantly enhances overall quality of life.
Common Myths and Facts About Type 2 Diabetes
Misunderstandings surrounding type 2 diabetes can often lead to confusion, ineffective management, and unnecessary stress. Let’s clearly distinguish myth from reality to better understand how you can manage or prevent type 2 diabetes effectively.
| Common Myth | Correct Fact |
|---|---|
| Only overweight people develop type 2 diabetes. | While obesity is a significant risk factor, genetics, age, and lifestyle factors also play crucial roles. Even individuals with a healthy weight can develop diabetes due to genetic or other health factors. |
| Eating sugar directly causes diabetes. | Eating sugar alone doesn’t cause diabetes; however, frequent consumption of sugary foods increases insulin resistance, significantly elevating diabetes risk over time. |
| Diabetes medications mean no need for lifestyle changes. | Medication helps manage diabetes, but effective long-term management requires healthy dietary habits and regular physical activity. |
| Type 2 diabetes always shows obvious symptoms. | Many people experience subtle or no symptoms initially. Regular screening is important, especially if you’re at higher risk. |
| Type 2 diabetes isn’t serious. | Unmanaged diabetes can lead to severe complications, including heart disease, kidney failure, nerve damage, and blindness. |
| Sugar consumption alone directly causes diabetes. | It’s the continuous overconsumption of carbohydrates and sugars leading to insulin resistance—not sugar consumption alone—that contributes significantly to type 2 diabetes. |
Understanding these truths can empower you to make informed decisions for your health and prevent common misconceptions from negatively affecting your diabetes management strategies.
Final Thoughts: Taking Control of Type 2 Diabetes
Type 2 diabetes is a chronic condition influenced by genetics, lifestyle, and environmental factors, but the good news is that it’s highly manageable—and in many cases, reversible. By adopting practical lifestyle strategies such as a ketogenic diet, intermittent fasting, structured exercise programs, and regular health screenings, you can significantly reduce insulin resistance and maintain healthy blood sugar levels.
Understanding diabetes clearly and taking early action are essential. If you’re ready to take the next step toward effectively managing your diabetes or exploring the possibility of remission, seek personalized guidance from a healthcare professional. With the right support, you can confidently navigate your journey towards better health and improved quality of life.
To access other content on the IFitCenter’s blog, you can use the following links:
References For Understanding Type 2 Diabetes
- Lu, X., Xie, Q., Pan, X. et al. Type 2 diabetes mellitus in adults: pathogenesis, prevention and therapy. Sig Transduct Target Ther 9, 262 (2024).
DOI: 10.1038/s41392-024-01951-9 - Ismail, L., Materwala, H., & Al Kaabi, J. (2021). Association of risk factors with type 2 diabetes: A systematic review. Computational and Structural Biotechnology Journal, 19, 1759-1785.
DOI: 10.1016/j.csbj.2021.03.003 - Galindo, R. J., Trujillo, J. M., Low Wang, C. C., & McCoy, R. G. (2023). Advances in the management of type 2 diabetes in adults. BMJ Medicine, 2(1), e000372.
DOI: 10.1136/bmjmed-2022-000372 - Su, W., Tao, M., Ma, L., Tang, K., Xiong, F., Dai, X., & Qin, Y. (2023). Dose-response relationships of resistance training in Type 2 diabetes mellitus: A meta-analysis of randomized controlled trials. Frontiers in Endocrinology, 14, Article 1224161.
DOI: 10.3389/fendo.2023.1224161 - Misra, S., Wagner, R., Ozkan, B., et al. (2023). Precision subclassification of type 2 diabetes: a systematic review. Communications Medicine, 3, Article 138.
- DOI: 10.1038/s43856-023-00360-3



