What if your immune system—designed to protect you from harmful invaders—suddenly turned against your own body? How would your life change if you needed to calculate and monitor every bite of food, every minute of exercise, and administer life-saving medication multiple times daily? For millions living with Type 1 diabetes worldwide, these aren’t hypothetical questions but daily realities.
Have you ever wondered why some people with diabetes need insulin injections from diagnosis, while others manage with pills or lifestyle changes? Or perhaps you’re newly diagnosed with Type 1 diabetes and feel overwhelmed by the sudden need to monitor blood glucose, count carbohydrates, and administer insulin precisely?
Type 1 diabetes is fundamentally different from other forms of diabetes. It’s an autoimmune condition where the body attacks and destroys insulin-producing beta cells in the pancreas, leading to a lifelong dependency on external insulin. Unlike Type 2 diabetes, Type 1 cannot be prevented or reversed through lifestyle changes alone.
At IFitCenter Clinic in Dubai, we’re dedicated to providing comprehensive education about Type 1 diabetes management. While we don’t conduct research ourselves, we bring together the latest evidence-based approaches to help our patients navigate this complex condition with confidence.
What Is Type 1 Diabetes?
Type 1 diabetes is an autoimmune condition where the body’s immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. This destruction leads to an inability to produce sufficient insulin, a hormone essential for survival.
Insulin serves as a key that allows glucose (sugar) from the bloodstream to enter cells where it’s used for energy. Without insulin, glucose remains trapped in the bloodstream while cells essentially starve. This explains why untreated Type 1 diabetes causes high blood sugar levels alongside weight loss and fatigue—the body can’t use the glucose and must break down fat and muscle for energy instead.
Type 1 vs. Type 2 Diabetes: Key Differences
| Characteristic | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Cause | Autoimmune destruction of beta cells | Insulin resistance with declining production |
| Onset | Usually sudden; develops over weeks | Gradual; may be asymptomatic for years |
| Age | Any age, often in youth but 50% in adults | Typically adults, increasing in younger people |
| Body Type | Any body type; not linked to weight | Often associated with overweight/obesity |
| Treatment | Requires insulin from diagnosis | Often begins with lifestyle changes, oral medications |
| Prevention | Cannot be prevented | Often preventable through lifestyle changes |
Unlike Type 2 diabetes, Type 1 is not caused by diet or lifestyle factors. No actions or choices cause the immune system to attack beta cells, and with current medical knowledge, the condition cannot be prevented.
Who Develops Type 1 Diabetes?
Type 1 diabetes can develop at any age but typically appears during childhood, adolescence, or young adulthood. Several factors influence susceptibility:
- Genetics: Specific gene variations, particularly in the HLA complex, increase risk
- Family history: Having a first-degree relative with Type 1 increases risk, though most diagnosed don’t have a family history
- Geography: Higher rates occur in northern countries further from the equator
- Environmental triggers: Researchers are investigating certain viral infections and environmental factors
Type 1 diabetes is a lifelong condition with no cure, but with proper insulin therapy, blood glucose monitoring, and lifestyle management, people with Type 1 diabetes can lead full, active lives with minimal limitations. Modern technology continues to improve quality of life and health outcomes for those with the condition.
Type 1 Diabetes Symptoms and Diagnosis
Type 1 diabetes symptoms typically develop rapidly over days to weeks, unlike Type 2 diabetes which progresses more gradually. Recognizing these signs early is crucial for prompt diagnosis and treatment.
On the IFitCenter blog, we have provided a comprehensive guide for diabetes, completely free of charge and based on the latest research. By viewing these articles, in addition to increasing your general knowledge in this field, you can easily manage this disease in a principled manner. To access the first part of the articles, simply use the links below:
- What is Diabetes?
- Symptoms and Signs of Diabetes
- Difference Between Type 1 and Type 2 Diabetes
- What Are the Complications of Diabetes?
- Diabetes Diagnosis Method
- How to prevent diabetes with family history?
- White vinegar and blood sugar
Common Symptoms of Type 1 Diabetes

- Polydipsia (excessive thirst) – Your body tries to dilute high blood glucose by increasing thirst
- Polyuria (frequent urination) – Kidneys work overtime to filter excess glucose, increasing urination
- Polyphagia (increased hunger) – Despite high blood glucose, cells can’t access energy, triggering hunger
- Unexplained weight loss – When glucose can’t be used, the body breaks down fat and muscle
- Fatigue – Without glucose uptake into cells, energy levels drop significantly
- Blurred vision – High blood glucose affects the fluid balance in the eye lenses
Warning Signs Requiring Immediate Medical Attention
These symptoms may indicate diabetic ketoacidosis (DKA), a life-threatening emergency:
- Fruity-smelling breath
- Deep, rapid breathing
- Nausea and vomiting
- Confusion or altered mental state
- Extreme fatigue or drowsiness
Diagnostic Tests for Type 1 Diabetes
- Blood glucose tests – Random, fasting, or oral glucose tolerance tests to check blood sugar levels
- Glycated hemoglobin (A1C) – Measures average blood glucose over the past 2-3 months
- Autoantibody testing – Detects antibodies that attack insulin-producing cells
- C-peptide test – Measures how much insulin the body produces
- Ketone testing – Checks for ketones in urine or blood
Age Differences in Presentation
In Children: Symptoms often develop rapidly with prominent thirst, urination, and weight loss. Bedwetting in previously toilet-trained children can be a sign.
In Adults: May develop more gradually and be mistaken for Type 2 diabetes. Weight loss is often the most noticeable symptom.
Type 1 diabetes can develop at any age, with adults accounting for nearly half of all new diagnoses, contrary to its former name “juvenile diabetes.”
Type 1 Diabetes Causes and Risk Factors
Unlike Type 2 diabetes, Type 1 diabetes cannot be prevented through lifestyle changes. Understanding its causes helps clarify why this condition develops and dispels common misconceptions.
The Autoimmune Process
Type 1 diabetes occurs when the immune system mistakenly identifies beta cells in the pancreas as foreign invaders. In this autoimmune response, the body produces antibodies that target and destroy these insulin-producing cells. The most common antibodies involved include islet cell antibodies, insulin autoantibodies, glutamic acid decarboxylase (GAD65) antibodies, and tyrosine phosphatase autoantibodies.
This destruction process isn’t immediate. It typically progresses over months or years before enough beta cells are damaged to cause symptoms. By the time Type 1 diabetes is diagnosed, most of the insulin-producing capacity has already been lost.
Genetic Factors in Type 1 Diabetes
Genetics plays a significant role in Type 1 diabetes susceptibility. The condition involves multiple genes, with the human leukocyte antigen (HLA) complex on chromosome 6 being particularly important. People with specific HLA gene variants (HLA-DR3 and HLA-DR4) have a higher risk of developing Type 1 diabetes.
However, genetics alone doesn’t determine who develops Type 1 diabetes. Many people with high-risk genes never develop the condition, while others without these genes do. This suggests that additional factors must trigger the autoimmune response in genetically susceptible individuals.
Environmental Triggers Under Investigation
Researchers are studying various environmental factors that might trigger Type 1 diabetes in genetically predisposed individuals:
- Viral infections – Certain viruses, particularly enteroviruses, have been linked to Type 1 diabetes development. These viruses might trigger autoimmunity through molecular mimicry, where viral proteins resemble beta cell proteins.
- Early dietary factors – Research has explored whether early exposure to cow’s milk proteins, gluten, or the timing of introducing certain foods to infants might influence Type 1 diabetes risk.
- Vitamin D deficiency – Some studies suggest a connection between vitamin D levels and Type 1 diabetes risk, which might explain the higher incidence in northern countries with less sunlight.
- Gut microbiome – Differences in gut bacteria composition may influence immune system development and autoimmunity risk.
It’s important to note that none of these factors has been definitively proven to cause Type 1 diabetes, and research continues to explore these potential triggers.
Common Misconceptions About Type 1 Diabetes Causes
Several misconceptions about Type 1 diabetes causes persist:
- Sugar consumption myth – Type 1 diabetes is not caused by eating too much sugar. The autoimmune process has nothing to do with dietary choices.
- Preventability misconception – Currently, there is no known way to prevent Type 1 diabetes. It is not caused by lifestyle factors that can be modified.
- “Stress causes diabetes” myth – While stress can affect blood glucose levels in people who already have diabetes, it does not cause the autoimmune destruction of beta cells.
- Contagion myth – Type 1 diabetes is not contagious. You cannot “catch” it from someone who has it.
Understanding that Type 1 diabetes results from a complex interaction of genetic and environmental factors helps dispel blame and misconceptions while focusing attention on proper management rather than prevention.
Type 1 Diabetes Treatment and Management
Managing Type 1 diabetes requires three essential components: insulin therapy, blood glucose monitoring, and nutritional management.
To access the second part of the articles related to diabetes, you can use the following links:
- Is Diabetes Curable?
- Type 2 Diabetes Explained
- Relationship Between Diabetes and Obesity
- Causes of Diabetes
- Insulin Resistance and Diabetes
- Fruits to Avoid with Diabetes
- Can you drink alcohol with type 1 diabetes?
Insulin Therapy for Type 1 Diabetes: Types and Administration
Since the pancreas no longer produces insulin in Type 1 diabetes, replacement insulin therapy is essential for survival.
- Insulin types: Rapid-acting (for meals, peaks in 1-2 hours), long-acting (background insulin, lasts up to 24 hours), intermediate-acting, and premixed options
- Delivery methods: Syringes, insulin pens, smart pens, insulin pumps, and tubeless pump systems
- Dosing principles: Most people use a combination of basal (long-acting) insulin for background needs and bolus (rapid-acting) insulin for meals and corrections
- Special situations: Travel, exercise, illness, and missed doses require specific adjustments to insulin management
Blood Glucose Monitoring for Type 1 Diabetes
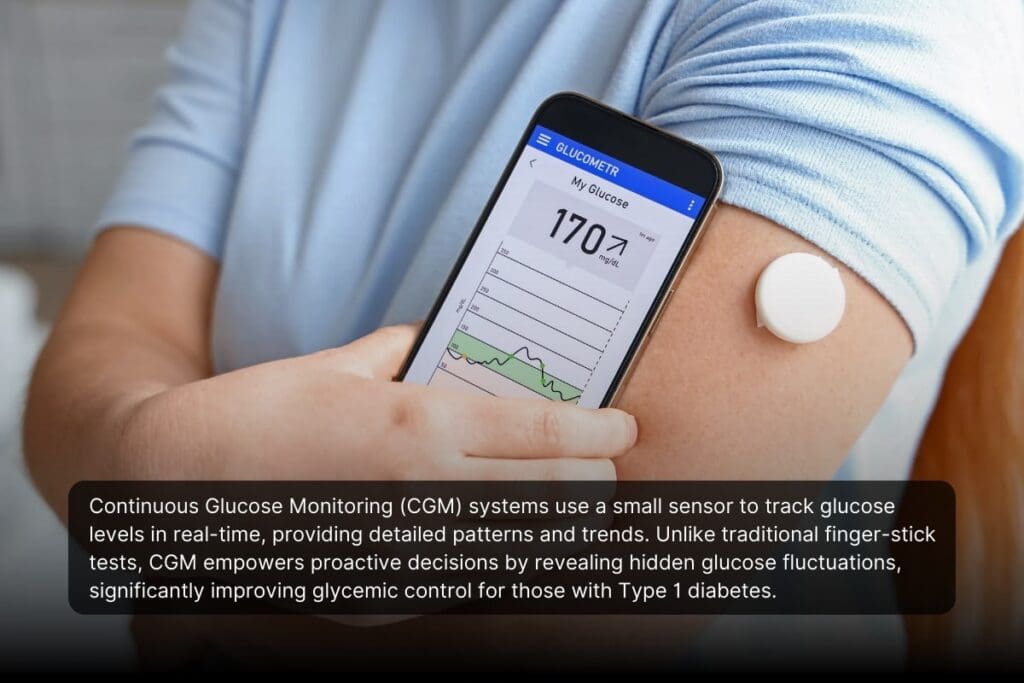
- Monitoring options: Traditional blood glucose meters (finger prick) or continuous glucose monitoring (CGM) systems that provide real-time data
- Target ranges: Typically 80-130 mg/dL before meals and below 180 mg/dL after meals, though individual targets vary
- Key metrics: Time in range (ideally above 70%), glucose variability, and recurring patterns
- Pattern management: Identifying trends and making systematic adjustments to address recurring highs or lows
Research shows CGM technology significantly improves glycemic control compared to traditional monitoring, especially for those with higher baseline HbA1c levels.
“One of the most transformative advances I’ve seen for Type 1 diabetes management is continuous glucose monitoring technology. The data clearly shows that CGM significantly decreases HbA1c levels compared to traditional finger-stick monitoring, with the most substantial benefits seen in patients whose initial control was suboptimal. What many people don’t realize is that CGM isn’t just about convenience—it fundamentally changes management by revealing glucose patterns and trends that would otherwise remain invisible, allowing for more precise and timely interventions.”
Dr. Babak Jamalian, Family Physician.
Type 1 Diabetes Diet and Nutrition: Meal Planning Strategies
- Nutritional approach: Individualized based on preferences and health goals; generally includes balanced intake of carbohydrates (50-55%), protein (15-20%), and fat (25-30%)
- Carbohydrate counting: Tracking carb intake to match insulin doses, shown to improve HbA1c levels compared to standard dietary education
- Glycemic index: Considering how quickly foods raise blood sugar; lower GI foods (beans, most fruits) cause a steadier rise than higher GI options (white bread, potatoes)
- Meal timing and composition: Regular meal times and balanced meals that include protein, fat, and fiber alongside carbohydrates help maintain stable glucose levels
Optimize Your Nutrition, Improve Your Diabetes Management
Although Type 1 diabetes requires insulin therapy, proper nutrition and weight management play a crucial role in optimizing insulin effectiveness and stabilizing blood sugar levels. At iFitCenter, we provide personalized nutritional counseling and medically supervised weight management programs specifically tailored to enhance your overall diabetes management.
Our comprehensive metabolic evaluations ensure your diet aligns perfectly with your insulin therapy, helping you achieve stable blood glucose and maintain a healthy weight, improving both your daily well-being and long-term health outcomes.
Take control of your diabetes management—start your personalized nutrition and weight management journey today.
Is There a Permanent Cure for Type 1 Diabetes?
Currently, there is no permanent cure for Type 1 diabetes. Despite significant advances in treatment options and management technologies, Type 1 diabetes remains a lifelong condition requiring insulin therapy. Once the autoimmune process has destroyed the insulin-producing beta cells in the pancreas, they cannot regenerate on their own.
However, promising research continues in several areas, including immunotherapy to preserve remaining beta cells in newly diagnosed patients, beta cell transplantation techniques, stem cell therapies that could potentially create new insulin-producing cells, and closed-loop insulin delivery systems (artificial pancreas technology) that automate insulin delivery.
While these developments offer hope for better management and potentially a type 1 diabetes cure in the future, people with Type 1 diabetes today need to focus on effective management strategies to maintain optimal health.
Living with Type 1 Diabetes
Beyond insulin therapy and glucose monitoring, successfully managing Type 1 diabetes involves integrating the condition into daily life. Two critical aspects of living well with Type 1 diabetes include physical activity management and emotional wellbeing.
Exercise and Type 1 Diabetes: Physical Activity Guidelines
Regular physical activity provides numerous benefits for people with Type 1 diabetes, including improved insulin sensitivity, cardiovascular health, and overall wellbeing. However, exercise affects blood glucose in complex ways that require planning and monitoring.
Exercise Effects on Blood Glucose
- Aerobic exercise (walking, swimming, cycling) typically lowers blood glucose by increasing insulin sensitivity
- Anaerobic exercise (weight lifting, sprinting) may temporarily raise blood glucose due to stress hormone release
- Mixed activities (team sports, interval training) can have variable effects requiring careful monitoring
- Timing matters – exercise effects can last for 24+ hours, potentially causing delayed hypoglycemia
Safety Guidelines for Exercise
- Check blood glucose before, during (for longer sessions), and after exercise
- Consider reducing insulin doses before planned exercise
- Have fast-acting carbohydrates readily available
- Wear medical identification indicating you have diabetes
- Exercise with a partner when possible, especially when trying new activities
- Stay hydrated to maintain accurate glucose readings
Strategies to Prevent Exercise-Related Hypoglycemia
- Consume 15-30g of carbohydrates before exercise if glucose is below target range
- Reduce pre-exercise bolus insulin by 25-75% depending on exercise intensity and duration
- For pump users, consider temporary basal rate reductions
- For prolonged activity, consume carbohydrates during exercise (10-15g per hour)
- Monitor glucose closely overnight after daytime exercise to catch delayed hypoglycemia
People with Type 1 diabetes participate successfully in virtually every sport and physical activity, from recreational to professional levels. With proper planning and glucose management, physical activity can be safely integrated into life with Type 1 diabetes.
Emotional Health and Type 1 Diabetes: Managing Psychological Impact
Living with Type 1 diabetes involves constant decision-making and attention to detail that can take a psychological toll. Recognizing and addressing the emotional aspects of diabetes management is essential for overall health.
Common Psychological Challenges
- Diabetes distress – Feelings of overwhelm, frustration, and burnout related to diabetes management demands
- Fear of hypoglycemia – Anxiety about low blood sugar that may lead to keeping glucose levels intentionally high
- Diabetes burnout – Exhaustion from constant management leading to reduced self-care
- Social concerns – Worries about how others perceive diabetes management activities
- Depression and anxiety – Higher rates among people with Type 1 diabetes compared to the general population
Building Emotional Resilience
- Set realistic management goals rather than aiming for perfection
- Practice self-compassion when glucose levels don’t cooperate despite best efforts
- Develop problem-solving skills for diabetes-related challenges
- Use positive self-talk to counter diabetes-related frustration
- Engage in stress-reduction practices like mindfulness, deep breathing, or yoga
When to Seek Support
Consider professional help if you experience:
- Persistent feelings of sadness, hopelessness, or anxiety
- Significant trouble maintaining diabetes management tasks
- Disordered eating behaviors related to diabetes management
- Social withdrawal or relationship difficulties due to diabetes
- Regular feelings of being overwhelmed by diabetes
Building Your Support Network
- Connect with diabetes peer support groups in-person or online
- Include family and friends in diabetes education
- Work with a mental health professional familiar with diabetes
- Join diabetes advocacy organizations or community events
- Consider diabetes camp programs for children and teens
Remember that attending to emotional health is just as important as physical management in living well with Type 1 diabetes. Acknowledging challenges and seeking appropriate support are signs of strength, not weakness, in the diabetes journey.
Type 1 Diabetes Complications and Challenges
Living with Type 1 diabetes involves navigating both short-term challenges and preventing long-term complications. Understanding how to manage these situations effectively is crucial for maintaining health and wellbeing.
Managing Sick Days with Type 1 Diabetes
Illness can make diabetes management more challenging as the body releases stress hormones that increase blood glucose levels. Key sick day management principles include:
- Continue taking insulin, even if eating less than usual
- Check blood glucose more frequently (every 2-4 hours)
- Test for ketones when blood glucose is consistently above 240 mg/dL
- Stay hydrated with sugar-free fluids
- Have easy-to-consume carbohydrates available (juice, regular soda, gelatin)
- Contact healthcare providers if vomiting persists, ketones are moderate to high, or blood glucose remains elevated despite correction doses
Hypoglycemia: Prevention and Treatment
Hypoglycemia (low blood glucose, typically below 70 mg/dL) requires prompt attention. Understanding its causes, symptoms, and treatment is essential:
- Common causes: Too much insulin, delayed/missed meals, unplanned exercise, alcohol consumption
- Warning signs: Shakiness, sweating, hunger, irritability, confusion, dizziness, blurred vision
- Treatment: Follow the 15-15 rule—consume 15g of fast-acting carbohydrates, wait 15 minutes, retest, and repeat if necessary
- Prevention strategies: Regular monitoring, consistent meal timing, adjusting insulin for activity, carrying fast-acting glucose
Severe hypoglycemia, where assistance is needed, may require glucagon administration by a caregiver. Glucagon emergency kits and nasal glucagon are available by prescription and should be part of every Type 1 diabetes emergency plan.
Hyperglycemia and Diabetic Ketoacidosis
Persistent high blood glucose (hyperglycemia) can lead to diabetic ketoacidosis (DKA), a serious condition requiring immediate medical attention:
- Causes of hyperglycemia: Insufficient insulin, excessive carbohydrate intake, illness, stress, certain medications
- Signs of hyperglycemia: Increased thirst and urination, fatigue, blurred vision, headache
- DKA warning signs: Nausea/vomiting, abdominal pain, fruity-smelling breath, deep rapid breathing, confusion
- Prevention: Regular monitoring, taking insulin as prescribed, adjusting doses when needed, knowing how to handle sick days
Long-term Complications and Preventive Care
Consistent diabetes management helps prevent or delay long-term complications affecting various body systems:
- Eye complications (retinopathy): Annual comprehensive eye exams help detect early changes
- Kidney disease (nephropathy): Regular urine and blood tests can identify early kidney damage
- Nerve damage (neuropathy): Foot examinations and proper foot care help prevent complications
- Cardiovascular disease: Managing blood pressure, cholesterol, and avoiding smoking reduces risk
Recommended screening schedule for adults with Type 1 diabetes:
- Comprehensive eye exam: Annually
- Kidney function tests: Annually
- Comprehensive foot exam: Annually (self-checks daily)
- Blood pressure: At routine visits
- Cholesterol levels: Annually
- Dental examinations: Twice yearly
Type 1 Diabetes Research and Technology
Technological advancements and ongoing research continue to transform Type 1 diabetes management, offering improved quality of life and hope for better treatments.
Advanced Diabetes Management Technologies
- Next-generation continuous glucose monitoring (CGM): Newer systems offer improved accuracy, longer sensor wear times, and smartphone integration
- Automated insulin delivery systems: “Hybrid closed-loop” systems that automatically adjust basal insulin delivery based on CGM readings
- Smart insulin pens: Track insulin doses, timing, and can suggest dose calculations
- Digital health platforms: Apps and cloud-based solutions that integrate diabetes data for better decision-making
Research shows that CGM technology significantly improves glycemic control in Type 1 diabetes compared to traditional finger-stick monitoring, with particular benefits for those with higher baseline HbA1c levels.
“Recent research on immunotherapy in Type 1 diabetes is showing remarkable promise. In clinical trials, medications like ustekinumab have demonstrated a 49% higher preservation of beta cell function compared to placebo after 12 months. This represents a significant shift from merely managing symptoms to potentially altering the disease course by targeting the specific immune cells responsible for beta cell destruction. While we’re not at a cure yet, these targeted approaches may eventually lead to treatments that significantly reduce or delay insulin dependence.”
Dr. Babak Jamalian, Family Physician.
Current Research Directions
- Immunotherapy approaches: Treatments like ustekinumab showing promise in preserving beta cell function in recently diagnosed patients
- Beta cell replacement: Islet cell transplantation and encapsulation technologies to protect transplanted cells from immune attack
- Stem cell research: Developing insulin-producing cells from stem cells that could be transplanted into patients
- Smart insulins: Glucose-responsive insulin that would activate only when blood glucose rises
- Dual-hormone systems: Adding glucagon delivery to insulin pumps to prevent hypoglycemia
Progress Toward a Cure – Type 1 Diabetes New Cure
While a definitive cure for Type 1 diabetes remains elusive, several promising approaches offer hope:
- Prevention studies: Identifying high-risk individuals and intervening before diabetes develops
- Immune system modulation: Therapies that selectively target the autoimmune process while preserving overall immune function
- Regenerative medicine: Stimulating remaining beta cells to replicate or convert other pancreatic cells into insulin producers
- Gene therapy: Modifying genes to protect beta cells or enable other cells to produce insulin
While these research areas show promise, it’s important to maintain realistic expectations. Major advances typically progress through years of careful research and clinical trials before becoming widely available treatments.
In the meantime, focusing on optimal management with current tools and technologies remains the best approach for those living with Type 1 diabetes. Each technological advancement brings incremental improvements in quality of life and health outcomes while researchers continue pursuing more transformative solutions.
Living Well with Type 1 Diabetes
Type 1 diabetes requires daily management through insulin therapy, blood glucose monitoring, and thoughtful nutrition choices, but it doesn’t define a person’s capabilities or potential. With proper understanding of the autoimmune nature of the condition, appropriate management techniques, and attention to both physical and emotional wellbeing, people with Type 1 diabetes can lead full, active lives with minimal limitations. The evolution of management technologies like continuous glucose monitoring and advanced insulin delivery systems continues to make life with Type 1 diabetes increasingly manageable.
While there is currently no cure for Type 1 diabetes, focusing on effective management strategies today offers the best path to long-term health. Each person’s experience with Type 1 diabetes is unique, making personalized care plans essential. At IFitCenter, we understand the importance of individualized approaches to diabetes management that fit seamlessly into everyday life. Working closely with healthcare providers who understand the complexities of Type 1 diabetes provides the support needed to thrive while living with this condition.
To access other content on the IFitCenter’s blog, you can use the following links:
References for Explaining Type 1 Diabetes
- Harding, J. L., Wander, P. L., Zhang, X., Li, X., Karuranga, S., Chen, H., Sun, H., Xie, Y., Oram, R. A., Magliano, D. J., Zhou, Z., Jenkins, A. J., & Ma, R. C. W. (2022). The incidence of adult-onset type 1 diabetes: A systematic review from 32 countries and regions. Diabetes Care, 45(4), 994–1006.
DOI: 10.2337/dc21-1752 - Mobasseri, M., Shirmohammadi, M., Amiri, T., Vahed, N., Hosseini Fard, H., & Ghojazadeh, M. (2020). Prevalence and incidence of type 1 diabetes in the world: A systematic review and meta-analysis. Health Promotion Perspectives, 10(2), 98–115.
DOI: 10.34172/hpp.2020.18 - Fu, S., Li, L., Deng, S., et al. (2016). Effectiveness of advanced carbohydrate counting in type 1 diabetes mellitus: A systematic review and meta-analysis. Scientific Reports, 6, 37067.
DOI: 10.1038/srep37067 - Kaushik, A., Rekhi, T. K., Puri, S., & Tandon, N. (2024). Nutritional guidelines for patients with type 1 diabetes mellitus and its adherence: A narrative review. Indian Journal of Endocrinology and Metabolism, 28(5), 461–469.
DOI: 10.4103/ijem.ijem_104_24 - Teo, E., Hassan, N., Tam, W., & Koh, S. (2022). Effectiveness of continuous glucose monitoring in maintaining glycaemic control among people with type 1 diabetes mellitus: A systematic review of randomised controlled trials and meta-analysis. Diabetologia, 65(4), 604–619.
DOI: 10.1007/s00125-021-05648-4



