Are you sitting quietly for five full minutes before measuring your blood pressure? Is your arm positioned at heart level with your back supported? Are you taking multiple readings and averaging them? If you answered “no” to any of these questions, you might be getting blood pressure readings that are off by 10-20 mmHg—enough to completely change your diagnosis from normal to hypertensive, or vice versa.
How confident are you that your home blood pressure readings are accurate? When was the last time you verified your monitor’s calibration? Do you know if your device has been clinically validated for accuracy? For the millions of people monitoring blood pressure at home, these aren’t just technical details—they’re questions that could affect life-altering medical decisions.
What if the “high blood pressure” you’ve been treating isn’t actually high at all? Or more dangerously, what if your normal-looking readings are masking hypertension because of measurement errors? At IFitCenter, these aren’t hypothetical scenarios—they’re real situations we encounter with patients who haven’t been properly instructed in blood pressure measurement techniques.
In this detailed guide, we’ll answer all these critical questions and provide clear, evidence-based instructions for measuring your blood pressure correctly at home. We’ll also identify the most common mistakes people make and show y10 Common Blood Pressureou exactly how to avoid them. Whether you’re monitoring existing hypertension or checking your blood pressure as part of a healthy lifestyle, these techniques will ensure your readings truly reflect your cardiovascular status.
Understanding Blood Pressure Numbers and Measurement Units
Blood pressure is measured using two numbers, and understanding what these numbers mean is crucial for interpreting your readings correctly. Think of your cardiovascular system as a plumbing network, with your heart as the pump and your blood vessels as the pipes carrying water throughout your home.
Systolic vs. Diastolic: What the Numbers Mean
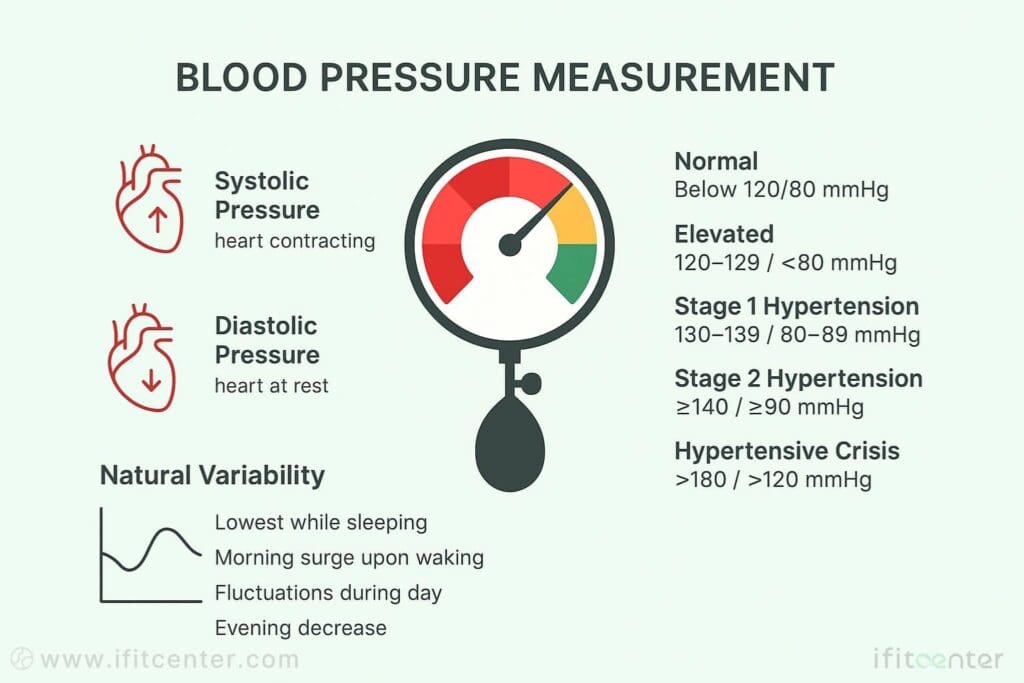
When you see a blood pressure reading like 120/80 mmHg, you’re looking at two distinct measurements:
- Systolic pressure (the top number): This measures the force your blood exerts against your artery walls when your heart contracts or beats. Think of it like the surge of water pressure in your home’s pipes when someone suddenly turns on a faucet. In our example, the systolic pressure is 120 mmHg.
- Diastolic pressure (the bottom number): This measures the force when your heart is at rest between beats. Continuing our plumbing analogy, this is like the baseline pressure that remains in your pipes even when no water is actively flowing. In our example, the diastolic pressure is 80 mmHg.
The unit “mmHg” stands for millimeters of mercury, which comes from the traditional way blood pressure was measured using a column of mercury that would rise and fall with each heartbeat.
Blood Pressure Categories: What’s Normal and What’s Not
According to the latest clinical guidelines from the American Heart Association and the American College of Cardiology, blood pressure readings fall into these categories:
| Category | Systolic (mmHg) | Diastolic (mmHg) | |
| Normal | Less than 120 | and | Less than 80 |
| Elevated | 120-129 | and | Less than 80 |
| Hypertension Stage 1 | 130-139 | or | 80-89 |
| Hypertension Stage 2 | 140 or higher | or | 90 or higher |
| Hypertensive Crisis | Higher than 180 | and/or | Higher than 120 |
It’s important to note that these classifications were updated in 2017, lowering the threshold for hypertension from 140/90 mmHg to 130/80 mmHg. This change meant that many people who previously had “pre-hypertension” were reclassified as having Stage 1 hypertension.
On the IFitCenter blog, we have prepared a free information database about various diseases, including high blood pressure, for you, our dear readers. By reviewing these resources, you will gain valuable information for controlling and preventing these conditions. To access the first part of the information, you can use the links below:
- What Is Normal Blood Pressure?
- Blood Pressure Chart
- Cause of High Blood Pressure
- Signs and Symptoms of High Blood Pressure
- How to Lower Blood Pressure Naturally?
Why Both Numbers Matter in Blood Pressure Measurement
While both systolic and diastolic blood pressure measurements are important, research has shown that they can predict different types of cardiovascular risks depending on your age and health status.
For most adults, especially those over 50, the systolic blood pressure is more important for predicting future cardiovascular events. This is because systolic pressure tends to rise naturally with age as arteries become stiffer. According to the Framingham Heart Study, elevated systolic pressure is associated with increased risk of heart attack, stroke, heart failure, and kidney disease.
However, for adults under 50, the diastolic pressure often provides more valuable information. Elevated diastolic pressure in younger people can indicate increased resistance in small blood vessels and may be an early warning sign of cardiovascular disease.
The relationship between these two numbers can also tell your healthcare provider important information about your cardiovascular health. For instance, a wide pulse pressure (the difference between systolic and diastolic readings) may indicate arterial stiffness, especially in older adults.
Blood Pressure Variability Throughout the Day
Your blood pressure isn’t constant—it naturally fluctuates throughout the day in response to various factors. Typically, blood pressure is:
- Lowest while sleeping (with a natural dip of 10-20% during the night)
- Rises sharply upon waking (the morning surge)
- Fluctuates during the day in response to stress, physical activity, digestion, and emotions
- Often highest in the middle of the afternoon
- Begins to decrease again in the evening
These natural fluctuations are why healthcare professionals recommend taking multiple readings at the same time each day over several days to establish your true blood pressure pattern. A single reading—especially one taken during a stressful doctor’s visit—may not accurately reflect your typical blood pressure.
Understanding these natural variations can help you avoid unnecessary concern over isolated high readings, while also helping you recognize when a pattern of elevated readings might require medical attention.
Choosing the Right Blood Pressure Measurement Instrument
Selecting the proper blood pressure measurement instrument is just as important as using the correct technique. The wrong device can lead to inaccurate readings, potentially resulting in improper treatment decisions.
Types of Blood Pressure Monitors: Which One Should You Choose?
There are several types of blood pressure monitors available for home use, each with its own advantages and limitations:
- Automatic upper arm monitors: These are the most recommended devices for home use. They automatically inflate the cuff and provide digital readings of your blood pressure and pulse rate. Research shows these devices offer the best balance of accuracy, ease of use, and reliability for most people.
- Manual sphygmomanometers: These traditional devices consist of an inflatable cuff, a measuring unit, and a stethoscope to listen for Korotkoff sounds. While they can be very accurate when used correctly, they require proper training and skill. Unless you’ve been trained in auscultatory technique, automatic monitors are a better choice.
- Wrist monitors: These are more portable than upper arm monitors but generally less accurate. Even small variations in wrist position relative to your heart can significantly affect readings. They’re only recommended in specific situations where upper arm measurement isn’t possible, such as for people with very large arm circumference.
- Finger monitors: These devices are not recommended for clinical use or reliable home monitoring. They’re highly susceptible to measurement errors due to peripheral vasoconstriction, circulation issues, and improper positioning.
Essential Features for a Quality Home Blood Pressure Monitor
When choosing a blood pressure measurement instrument for home use, look for these important features:
- Clinical validation: This is the most important factor. Only use devices that have been validated for accuracy using established protocols from organizations like the Association for the Advancement of Medical Instrumentation (AAMI), the European Society of Hypertension (ESH), or the International Organization for Standardization (ISO).
- Appropriate cuff size options: A properly fitting cuff is crucial for accurate readings. The width of the bladder inside the cuff should be about 40% of your upper arm circumference, and the length should be 80-100% of your arm circumference. Many monitors come with medium-sized cuffs that fit most adults, but if you have a larger or smaller arm, look for a device that offers multiple cuff sizes.
- Memory and averaging functions: Devices that store previous readings and calculate averages are helpful for tracking your blood pressure over time. Some advanced monitors can store readings for multiple users.
- User-friendly interface: Look for clear displays with large, easy-to-read numbers and intuitive buttons, especially important for older adults or those with visual impairments.
- Battery life and power options: Consider how the device is powered and how often you’ll need to replace batteries or recharge it.
Verifying Clinical Validation: How to Know Your Device is Accurate
Only 6-15% of blood pressure devices on the market have been properly validated for accuracy. To verify if your device is clinically validated:
- Check validation status through independent resources:
- STRIDE BP (international database)
- ValidateBP (American Medical Association)
- British and Irish Hypertension Society
- Look for statements on packaging or in the device manual mentioning validation according to protocols like AAMI/ESH/ISO 81060-2.
- Consult with healthcare professionals about recommended validated devices.
Using a validated device is critical—unvalidated monitors can produce readings that differ by 10-15 mmHg or more from actual values, potentially leading to incorrect treatment decisions.
The Critical Importance of Proper Cuff Size
Using the wrong cuff size is one of the most common causes of inaccurate blood pressure readings. A cuff that’s too small can artificially increase readings by 2-10 mmHg, while a cuff that’s too large might give readings that are falsely low.
To determine the right cuff size:
- Measure around the middle of your upper arm, midway between your shoulder and elbow.
- Use a cuff with a bladder length that’s 80-100% of your arm circumference and a width that’s 40% of arm circumference.
- Most manufacturers provide size ranges for their cuffs:
- Small adult: 22-26 cm (8.5-10.2 inches)
- Standard adult: 27-34 cm (10.6-13.3 inches)
- Large adult: 35-44 cm (13.7-17.3 inches)
- Extra large: 45-52 cm (17.7-20.5 inches)
Remember that the right instrument to measure blood pressure is one that’s appropriately validated, fits your arm correctly, and that you’ll use consistently. Accuracy is far more important than convenience when it comes to blood pressure monitoring.
The Correct Way to Measure Blood Pressure at Home: Step-by-Step Guide
Following the proper technique when measuring your blood pressure at home is essential for obtaining accurate readings. Even small deviations from the recommended procedure can lead to significant measurement errors.
Before You Measure: Essential Preparation Steps
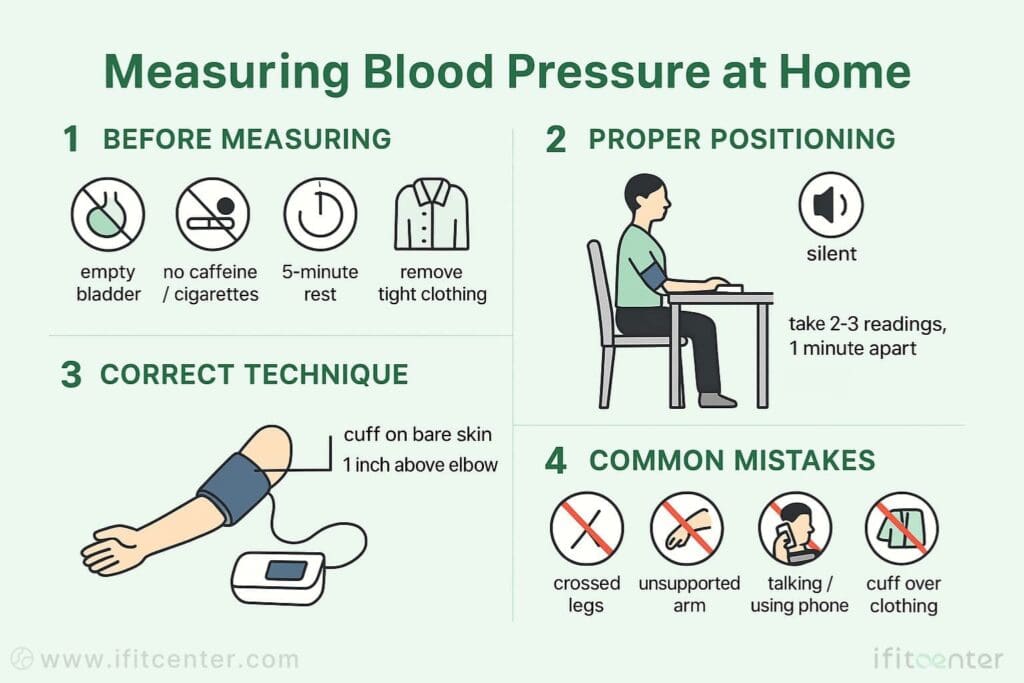
Proper preparation is crucial for accurate blood pressure readings. Before you begin:
- Empty your bladder – A full bladder can raise your blood pressure reading by 10-15 mmHg
- Avoid stimulants – No caffeine, nicotine, or alcohol for at least 30 minutes before measurement
- Rest before measuring – Avoid exercise for 30 minutes and sit quietly for 5 minutes before taking your reading
- Remove restrictive clothing – Roll up your sleeve or remove tight clothing from your arm
- Find a quiet environment – Choose a place free from distractions and noise
Proper Positioning for Accurate Measurement
Your body position significantly affects blood pressure readings. The correct position includes:
- Sitting upright – Use a chair with back support, not a stool or couch edge
- Feet flat on the floor – Uncross your legs and keep both feet flat on the ground
- Arm supported at heart level – Rest your arm on a table or armrest; arm dangling too low or held too high can alter readings by 5-10 mmHg
- Remain silent – Talking during measurement can raise readings by 10-15 mmHg
Step-by-Step Measurement Procedure
Follow these steps for the most accurate blood pressure readings:
- Position the cuff correctly – Place it on bare skin, about 1 inch (2-3 cm) above the bend of your elbow, with the bottom edge of the cuff at the same level as your heart
- Secure the cuff – It should be snug but not too tight. You should be able to slip two fingertips under the edge
- Position your arm – Keep your palm facing upward with your arm slightly bent
- Start the measurement – Activate your device and remain still and quiet during the entire process
- Wait one minute – Then take a second reading to verify the result
- Take a third reading – If the first two readings differ by more than 5 mmHg
- Calculate the average – For multiple readings, use the average value
- Record your results – Note the date, time, readings, and which arm you used
Common Measurement Pitfalls to Avoid
- Rushing the process – Not resting for 5 minutes can elevate readings by 10-20 mmHg
- Incorrect cuff position – Placing the cuff over clothing or incorrectly on the arm
- Poor body position – Slouching, crossing legs, or unsupported arms
- Taking only one reading – Blood pressure naturally varies, so single readings can be misleading
- Inconsistent timing – Measuring at different times of day without accounting for natural variations
By following these guidelines, you can ensure your home blood pressure readings are as accurate as possible, giving you and your healthcare provider reliable information for managing your cardiovascular health.
Boost Heart Health with IFitCenter
Accurate blood pressure monitoring is essential, but sustainable management often requires targeted lifestyle changes. At IFitCenter, guided by Dr. Babak Jamalian, our specialized weight-loss and wellness programs directly support healthy blood pressure through:
✔ Customized nutritional advice
✔ Targeted weight-loss strategies
✔ Continuous health monitoring
Take the proactive step toward lasting cardiovascular health today.
10 Common Blood Pressure Measurement Errors to Avoid
Even with the right equipment, your blood pressure readings can be significantly inaccurate if you make these common measurement mistakes. Each error can impact your readings by several points, potentially leading to misdiagnosis or inappropriate treatment decisions.
The Most Common Measurement Mistakes and Their Impact
- Not resting before measurement
Skipping the recommended 5-minute rest period before measuring can elevate your systolic reading by 5-11 mmHg. Your body needs time to reach a true resting state for accurate readings. - Using incorrect cuff size
A cuff that’s too small can artificially increase readings by 2-11 mmHg, while one that’s too large may give falsely low readings by 5-10 mmHg. Always measure your arm circumference and use the appropriate cuff size. - Improper arm position
Position matters significantly—an arm held below heart level can raise readings by 5-17 mmHg, while holding it above heart level can lower readings by a similar amount. Always rest your arm on a surface at heart level. - Crossing your legs
This seemingly minor position issue can increase readings by 5-15 mmHg by affecting blood flow. Keep both feet flat on the floor with uncrossed legs. - Talking during measurement
Even casual conversation during measurement can raise systolic pressure by 7-15 mmHg. Remain quiet throughout the entire measuring process. - Not emptying your bladder
A full bladder can elevate readings by 10-15 mmHg due to increased abdominal pressure and nervous system activation. Always use the bathroom before measuring. - Recent caffeine, nicotine, or exercise
These stimulants can increase blood pressure by up to 20 mmHg, with effects lasting 30 minutes or more. Avoid these activities before taking measurements. - Measuring over clothing
Taking readings over clothing can cause inaccurate results that vary depending on thickness. Always place the cuff on bare skin. - Taking only one reading
Blood pressure naturally fluctuates, making single readings unreliable. Always take at least two readings one minute apart and calculate the average. - Using uncalibrated or unvalidated equipment
Devices that haven’t been clinically validated can produce readings that differ significantly from actual values. Always use validated equipment and periodically verify calibration.
These errors are particularly concerning because most of them tend to artificially increase readings, potentially leading to unnecessary medication and treatment. By avoiding these common mistakes, you can ensure more accurate home monitoring and better health decisions.
“What many patients don’t realize is that even brief talking during measurement can raise systolic blood pressure by up to 15 mmHg. I’ve seen patients whose blood pressure classification changed entirely from normal to hypertensive simply because they were explaining their symptoms while the cuff was inflating. This one error alone can lead to unnecessary medication with potential side effects.”
Dr. Babak Jamalian, Family Physician
Tracking and Understanding Your Blood Pressure Results
Proper blood pressure monitoring isn’t just about taking accurate measurements—it’s also about tracking results over time to identify patterns and trends. Systematic recording of your readings provides valuable information that can help guide treatment decisions and lifestyle adjustments.
How Often to Measure Your Blood Pressure at Home
The ideal monitoring frequency depends on your specific situation:
- For initial assessment: Follow a 7-day protocol with duplicate morning and evening readings (before taking medications and meals). Take two readings 1 minute apart each time, resulting in 28 measurements total. This provides a reliable baseline.
- For stable, controlled blood pressure: Weekly monitoring is usually sufficient. Choose consistent days and times to maintain comparability.
- During medication adjustments: Daily measurements help track how your body responds to new medications or dosage changes. Measure at the same times each day, including when medications are expected to have peak effect.
- For hypertensive conditions: 2-3 times per week at varying times can help ensure continued control and identify any developing patterns.
Methods for Recording Blood Pressure Measurements
Consistent recording is essential for meaningful tracking. Choose from these effective methods:
- Paper journals: Simple, accessible, and doesn’t require technology. Record date, time, readings, which arm was used, and any relevant factors (medication timing, unusual stress, etc.).
- Device memory: Most modern blood pressure monitors store previous readings. This is convenient but limits your ability to add notes about circumstances.
- Smartphone apps: Many free and paid apps are designed specifically for blood pressure tracking. They often provide trend analysis and can export reports for your healthcare provider.
- Spreadsheets: Create a simple template to track readings and calculate averages automatically.
For each entry, record: date, time, systolic pressure, diastolic pressure, pulse rate, which arm was used, and any relevant notes (recent meals, medications, physical or emotional state).
Analyzing Trends: What to Look For in Your Blood Pressure Data
Regular tracking allows you to identify important patterns that may require attention:
- Morning hypertension: Consistently higher readings within 1-2 hours of waking may indicate increased cardiovascular risk and might require medication timing adjustments.
- High variability: Fluctuations greater than 20 mmHg in systolic readings on the same day or between days may warrant medical consultation.
- Sustained high readings: Three or more consecutive readings above 135/85 mmHg at home (equivalent to 140/90 mmHg in clinical settings) should be discussed with your healthcare provider.
- Significant arm differences: A consistent difference of 10 mmHg or more between arms could indicate underlying vascular issues and should be reported to your doctor.
- Lack of nighttime dipping: If you’re using 24-hour monitoring and your blood pressure doesn’t decrease during sleep, this may indicate increased cardiovascular risk.
“The true value of home blood pressure monitoring isn’t in the individual readings but in the patterns they reveal over time. I’ve observed that patients who diligently track morning and evening readings discover that their blood pressure follows distinct circadian rhythms. This knowledge allows us to time medications more effectively and identify issues like non-dipping patterns—where pressure doesn’t decrease during sleep—which is associated with increased cardiovascular risk despite seemingly normal daytime readings.”
Dr. Babak Jamalian, Family Physician
Calculating Your Average Blood Pressure
Weekly and monthly averages often provide more valuable information than individual readings:
- Discard the first day’s readings (these are often higher due to anxiety about the measurement process)
- For each measuring session, use the average of the two readings
- Calculate separate averages for morning and evening readings
- For weekly averages, add all valid measurements and divide by the number of readings
- Monthly averages can help identify gradual trends that might not be apparent in shorter timeframes
Accurate blood pressure measurement at home is a valuable skill that can significantly impact your health management. By following the guidelines outlined in this article, you can ensure your readings truly reflect your cardiovascular status and provide reliable information for healthcare decisions.
Let’s recap the essential elements of proper blood pressure measurement:
- Choose the right equipment: Use a clinically validated upper arm monitor with the correct cuff size for your arm
- Prepare properly: Empty your bladder, avoid stimulants, and rest quietly for 5 minutes before measuring
- Position correctly: Sit with back supported, feet flat on floor, and arm at heart level
- Follow the procedure: Place the cuff on bare skin, remain still and quiet during measurement, and take multiple readings
- Track consistently: Record your readings systematically and look for important patterns
Remember that home blood pressure monitoring is not just about getting numbers—it’s about gaining insights into your cardiovascular health that can guide lifestyle choices and treatment decisions. When done correctly, it’s one of the most powerful self-care practices for managing hypertension and preventing serious complications.
Final expert tip: If your readings vary significantly between arms (difference of 10 mmHg or more), consistently use the arm with the higher reading for future measurements, as this more accurately reflects your true blood pressure. However, be sure to discuss this difference with your healthcare provider, as it may indicate underlying vascular issues.
To access other content on the IFitCenter’s blog, you can use the following links:
References
- Mancia, G., Kreutz, R., Brunström, M., Burnier, M., Grassi, G., Januszewicz, A., Muiesan, M. L., Tsioufis, K., Agabiti-Rosei, E., Algharably, E. A. E., Azizi, M., Benetos, A., Borghi, C., Hitij, J. B., Cifkova, R., Coca, A., Cruickshank, V., Danser, A. H. J., Pinho, R. M. D., Delles, C., Dominiczak, A. F., Dorobantu, M., Doumas, M., Fernández-Alfonso, M. S., Halimi, J. M., Járai, Z., Jelaković, B., Jordan, J., Kuznetsova, T., Laurent, S., Lovic, D., Lurbe, E., Mahfoud, F., Manolis, A., Migliąs, M., Narkiewicz, K., Niiranen, T., Palatini, P., Parati, G., Pathak, A., Persu, A., Polonia, J., Redon, J., Sarafidis, P., Schmieder, R., Spronck, B., Stabouli, S., Stergiou, G., Taddei, S., Thomopoulos, C., Tomaszewski, M., Van de Borne, P., Wanner, C., Weber, T., Williams, B., Zhang, Z. Y., & Kjeldsen, S. E. (2023). 2023 ESH Guidelines for the management of arterial hypertension. Journal of Hypertension, 41(12), 1874-2071. DOI: 10.1097/HJH.0000000000003480
- Murthy, S., Rajwar, E., Johnson, R., Shrivastava, K., Kamath, P., Rahman, R., Devaria, A., Ismavel, V. A., Vetter, B. N., Jacob, A. G., & John, O. (2023). Validation of Blood Pressure Devices as per 2020 World Health Organization Technical Specifications: A Scoping Review of Global Literature. Hypertension, 80(5). DOI: 10.1161/HYPERTENSIONAHA.122.20425
- Theodosiadi, A., Ntousopoulos, V., Ntineri, A., Stathopoulou, P., Menti, A., Kyriakoulis, K. G., Kollias, A., & Stergiou, G. S. (2024). Validation of a novel professional automated auscultatory upper-arm cuff blood pressure monitor in a general population according to the AAMI/ESH/ISO Universal Standard: KOROT V2 Doctor (InBody BPBIO280KV). Blood Pressure Monitoring, 29(4), 212-216. DOI: 10.1097/MBP.0000000000000707
- Muntner, P., Shimbo, D., Carey, R. M., Charleston, J. B., Gaillard, T., Misra, S., Myers, M. G., et al. (2019). Measurement of Blood Pressure in Humans: A Scientific Statement From the American Heart Association. Hypertension, 73(5). DOI: 10.1161/HYP.0000000000000087



