“Can I eat bananas with fatty liver disease?” “Is Apple Good for Fatty Liver” “Should I avoid all fruits completely?” These are questions we hear daily from people struggling with fatty liver disease. The confusion is understandable – especially when different sources offer contradicting advice about fruits and liver health.
What if you could know exactly which fruits support liver healing and which ones might be hindering your progress? Recent clinical studies published in Hepatology International have identified specific fruits that can actively reduce liver fat content, while others may contribute to its accumulation. At IFitCenter, we’re breaking down this complex topic to provide clear, science-based guidance about fruits for fatty liver disease.
The key lies in understanding not just which fruits to eat, but also when and how to consume them. A 2024 study in the Journal of Hepatology found that proper fruit selection and timing can make the difference between supporting liver health and potentially compromising it. Let’s explore what medical science really tells us about the best and worst fruits for fatty liver disease.
Understanding Fruit’s Impact on Fatty Liver Disease
To understand how fruits affect your fatty liver, imagine your liver as a busy processing plant. When you eat fruit, your liver acts like a sophisticated sorting facility, processing different types of sugars in distinct ways. But not all sugars are treated equally by your liver, and this is where the story gets interesting.
“Many patients focus solely on eliminating fruits completely, but this overlooks a crucial scientific fact: not all fruits impact your liver the same way. While your liver must process nearly 100% of fructose from fruit juices and dried fruits, whole fruits contain natural compounds that help regulate this process. It’s why someone consuming whole fruits has a very different liver response compared to drinking the same amount in juice form.”
Dr. Babak Jamalian, Family Physician.
How Your Liver Processes Different Fruit Sugars
When you eat fruit, you’re primarily consuming two types of sugar: glucose and fructose. Glucose is like a universal fuel that every cell in your body can use. Your liver processes about 20% of it, while the rest is distributed to other cells throughout your body.
Fructose, however, is different. Your liver must process nearly 100% of the fructose you consume. Think of it like this: while glucose has multiple processing plants (your body’s cells), fructose has just one – your liver. When you consume too much fructose, this single processing plant can become overwhelmed.
The Critical Relationship Between Fructose and Liver Health
Recent research published in the Journal of Hepatology has shown that excessive fructose consumption can increase liver fat accumulation To a considerable extent in just six weeks. Unlike glucose, when your liver processes fructose, it’s more likely to convert it directly into fat, especially when consumed in large amounts.
However, this doesn’t mean all fruits are harmful. The key lies in understanding that whole fruits come packaged with fiber, vitamins, and antioxidants that help modulate how your body processes their sugars. It’s why eating an apple has a very different effect on your liver than drinking apple juice.
Key Factors That Determine If a Fruit Helps or Harms Liver Health
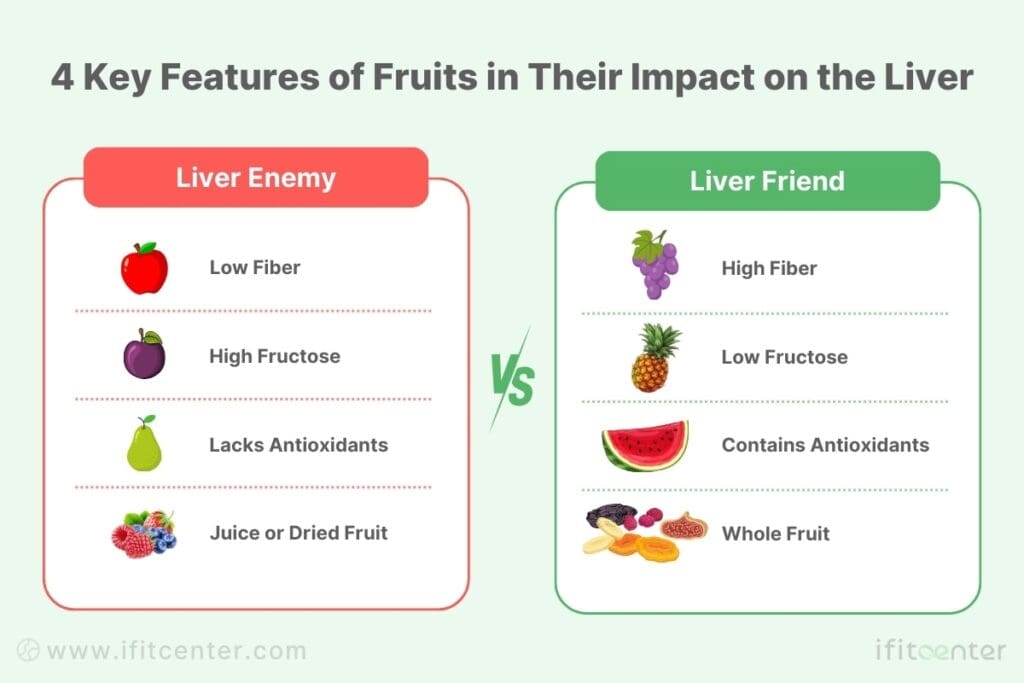
- Fiber Content: Higher fiber content slows sugar absorption
- Total Fructose Load: Lower amounts are easier for your liver to process
- Antioxidant Profile: Certain antioxidants help protect liver cells
- Form of Consumption: Whole fruits versus juices or dried fruits
Understanding these factors helps explain why berries, with their high antioxidant content and relatively low fructose load, consistently show beneficial effects on liver health in research studies, while fruit juices often show the opposite effect.
Fruits Good for Fatty Liver: Scientific Evidence and Guidelines
Not all fruits affect your liver the same way. Research published in the Journal of Clinical Endocrinology and Metabolism reveals that specific categories of fruits can actively support liver healing when consumed appropriately. Let’s explore these beneficial fruits based on their key properties.
On the IFitCenter blog, we have published a free content database about fatty liver disease that can have a significant impact for you in controlling and preventing this disease. For access, simply use the links below:
- what is a fatty liver and what causes it?
- causes of fatty liver
- fatty liver signs and symptoms
- types of fatty liver
- fatty liver fasting
- fatty liver disease diagnosis
Low-Fructose Fruits: Safe Options for Fatty Liver Recovery
When choosing fruits for fatty liver disease, fructose content is a crucial factor. Recent research in Hepatology International shows that low-fructose fruits can be safely incorporated into a liver-healthy diet. Here are the best options:
- Berries (strawberries, raspberries, blackberries)
– Contains only 3-4g fructose per 100g serving
– Rich in liver-protective compounds - Citrus fruits (lemons, limes, grapefruit)
– Lower fructose content compared to other fruits
– High in vitamin C for liver support - Avocados
– Minimal fructose content
– High in healthy fats that support liver function
Antioxidant-Rich Fruits That Support Liver Health
A study in the Antioxidants, 2022 found that fruits rich in specific antioxidants can reduce liver inflammation by up to 20%. These powerful compounds include:
- Anthocyanins (found in dark berries)
– Reduce liver inflammation
– Support liver cell regeneration - Flavonoids (found in citrus fruits)
– Help reduce liver fat accumulation
– Protect liver cells from damage - Polyphenols (found in pomegranates)
– Combat oxidative stress in the liver
– Support overall liver function
High-Fiber Fruits for Improved Liver Function
According to research published in Frontiers in Public Health, 2022, dietary fiber plays a crucial role in liver health by supporting healthy gut bacteria and reducing fat accumulation. The following fruits offer optimal fiber content:
- Pears
– 5.5g fiber per medium fruit
– Helps regulate blood sugar levels - Apples
– 4.5g fiber per medium fruit
– Contains pectin for liver detoxification - Blackberries
– 7.6g fiber per cup
– Combines fiber benefits with antioxidant properties
Recommended Serving Guidelines for Liver Health
Research indicates that timing and portion control are crucial for maximizing benefits while minimizing fructose load:
- Limit fruit servings to 1-2 cups per day
- Pair fruits with protein or healthy fats to slow sugar absorption
- Choose whole fruits over juices or dried options
Remember: Even beneficial fruits should be consumed in moderation. The key is selecting the right types and eating them at appropriate times and amounts.
Personalized Nutrition for a Healthier Liver
Not all fruits are created equal—some support liver recovery, while others may worsen fatty liver. The key to long-term health is choosing the right fruits, in the right portions, at the right times.
At IFitCenter, we provide:
✔ Tailored meal plans designed to improve liver function
✔ Expert advice on which fruits to include and which to avoid
✔ A structured approach to reducing liver fat and improving metabolism
Start making smarter food choices today!
Fruits to Avoid for Fatty Liver Disease: What to Avoid and Why
While fruits can be part of a healthy diet with fatty liver disease, research published in the Journal of Hepatology shows that certain fruits may contribute to liver fat accumulation. Understanding which fruits to limit can be as important as knowing which ones to eat.
High-Fructose Fruits That May Worsen Fatty Liver
According to research in Hepatology International, when your liver is already struggling with fat accumulation, high-fructose fruits can add to the burden. A 2023 study found that excessive fructose intake can increase liver fat by up to 38% in just six weeks.
- Mangoes
– Contains 14.8g fructose per fruit
– Can spike blood sugar rapidly - Grapes
– High fructose concentration
– Easy to overconsume - Cherries
– Concentrated natural sugars
– Often eaten in large quantities
Better alternatives include berries, citrus fruits, and green apples, which contain less fructose and more beneficial compounds for liver health.
The Hidden Dangers of Dried Fruits and Fruit Concentrates
Research published in The Lancet Gastroenterology & Hepatology reveals that concentrated fruit products can deliver up to five times more fructose than their fresh counterparts. This concentration effect makes them particularly problematic for fatty liver disease.
Forms to Avoid:
- Dried Fruits
– Raisins (concentrated grape sugars)
– Dried dates (extremely high sugar content)
– Dried figs (concentrated natural sugars) - Fruit Juices
– Even 100% natural juices lack fiber
– Concentrated fructose load - Fruit Syrups
– Highly concentrated sugars
– Rapid liver absorption
Guidelines for Occasional Consumption
If you choose to include these fruits occasionally:
- Limiting the Consumption of Dried Fruits
- Always pair with protein or healthy fats
- Consume earlier in the day
- Choose fresh alternatives when possible
Remember: The form of fruit matters as much as the type. Whole fruits contain fiber and other compounds that help regulate sugar absorption, while processed forms can overwhelm your liver’s processing capacity.
To access the second part of the fatty liver content, I invite you to use the links below:
- foods to avoid with fatty liver
- eggs and fatty liver
- diet for liver disease recovery
- weight loss for fatty liver
- fasting and fatty liver
- best cooking oil for heart and diabetes
Smart Fruit Consumption Strategies for Fatty Liver Recovery
When it comes to managing fatty liver disease, it’s not just about which fruits you eat – timing and portions play crucial roles. Consuming fruit at specific intervals may help improve blood sugar management and reduce the fructose load on the liver.
Best Times to Eat Fruit with Fatty Liver Disease
According to recent studies in Hepatology International, the timing of fruit consumption significantly impacts how your liver processes fructose. Here are evidence-based guidelines:
- Morning (Best Time) – Higher insulin sensitivity – Better sugar metabolism – More active liver enzymes
- Pre-Exercise – Enhanced sugar utilization – Reduced liver storage
- Post-Meal Timing – Avoid eating fruits immediately after large meals – Wait at least 2-3 hours after main meals
Optimal Food Combinations for Liver Health
Research in The Lancet Gastroenterology & Hepatology demonstrates that combining fruits with certain foods can enhance their benefits while minimizing potential negative impacts:
- Protein Pairings – Slows sugar absorption – Stabilizes blood glucose – Example: Apple with almonds
- Healthy Fat Combinations – Reduces sugar spike – Improves nutrient absorption – Example: Berries with Greek yogurt
Smart Portion Control Guidelines
A 2023 study published in Hepatology shows that portion control is crucial for maximizing benefits while minimizing fructose load:
- Berries: 1/2 – 3/4 cup per serving
- Apple/Pear: 1 small fruit
- Citrus fruits: 1 medium fruit
- Total daily fruit servings: 1-2 maximum
Sample Daily Fruit Schedule
- Morning: Small apple with 1 tbsp almond butter
- Mid-Morning: 1/2 cup berries with Greek yogurt
- Afternoon: Small citrus fruit (if active)
Special Considerations: Adapting Fruit Consumption to Your Fatty Liver Stage
Recent research published in Hepatology International reveals that the effectiveness of fruit consumption varies significantly based on your fatty liver stage. Understanding your specific stage helps create a more targeted approach to fruit consumption.
“A fascinating pattern I’ve observed in treating fatty liver disease is that the same fruit can have dramatically different effects based on when and how it’s consumed. For example, consuming berries with a protein source in the morning typically shows better liver enzyme responses compared to eating them alone or late in the day. This is why personalized timing and combination strategies are often more important than just fruit selection alone.”
Dr. Babak Jamalian, Family Physician.
Early-Stage Fatty Liver Fruit Guidelines
According to studies in the Journal of Hepatology, early-stage fatty liver patients show the most significant improvements with proper fruit consumption. During this stage:
- Recommended Fruits – Moderate consumption of low-fructose fruits (such as berries and apples) accompanied by protein or healthy fats
- Timing Flexibility – Can typically tolerate morning and afternoon consumption – 2-3 servings spread throughout day
- Progress Indicators – Sustainable Changes in Liver Enzymes Are Typically Observed After 6 Months of a Comprehensive Regimen (Including Weight Loss and Exercise)
Advanced Fatty Liver Considerations
For advanced stages, research shows that stricter guidelines may be necessary. A 2023 study in The Lancet Gastroenterology & Hepatology found that advanced fatty liver patients require more careful fruit selection:
- Avoiding dried fruits and fruit juices
- Limiting high-fructose fruits (such as grapes and mangoes)
- Critical Monitoring Points – Blood sugar response – Liver enzyme changes – Abdominal comfort levels
Monitoring Your Progress
Research indicates that tracking specific markers helps optimize fruit consumption for your liver stage:
- Key Indicators to Track – Liver enzyme levels – Blood sugar patterns – Body composition changes – Energy levels
- Adjustment Triggers – Increased fatigue after fruit consumption – Digestive discomfort – Changes in liver markers
Understanding your specific fatty liver stage is crucial for optimal fruit consumption. Different stages require different approaches, and what works in early stages may need modification as the condition progresses.
Managing Fruit Consumption with Diabetes and Fatty Liver Disease
When you have both diabetes and fatty liver disease, fruit consumption requires extra attention. Research published in The Lancet Gastroenterology & Hepatology shows that up to 70% of people with type 2 diabetes also have fatty liver disease, making this combination particularly common and challenging to manage.
Blood Sugar Impact and Liver Health
According to recent studies in the Journal of Hepatology, blood sugar fluctuations can significantly impact liver health. Understanding this connection helps make smarter fruit choices:
- Blood Sugar Response
– Rapid rises increase liver stress
– Can worsen insulin resistance
– May accelerate fat accumulation - Insulin Sensitivity
– Morning hours show better response
– Exercise improves fruit tolerance
– Individual responses vary significantly
Best Fruit Options for Diabetic Fatty Liver
Research in Hepatology International identifies specific fruits that minimize blood sugar impact while supporting liver health:
- Top Choices
– Berries (lowest glycemic impact)
– Green apples (high in pectin)
– Lemons/limes (minimal sugar content) - Portion Guidelines
Consumption of low glycemic index fruits such as raspberries or small apples in moderate amounts is recommended.
Essential Monitoring Strategies
A 2024 study in Diabetes Care recommends specific monitoring approaches:
- Before Consumption
– Check blood sugar levels
– Note time of day
– Record last meal timing - After Consumption
– Monitor at 1 and 2 hours
– Track energy levels
– Note any symptoms
Safe Consumption Guidelines
Clinical evidence suggests following these key principles:
- Timing Considerations
– Early morning consumption preferred
– Space 4 hours between servings - Food Combinations
– Pair with protein
– Include healthy fats
– Avoid combining with other carbs - Warning Signs
– Increased thirst
– Unusual fatigue
– Digestive changes
Remember: Individual responses to fruit can vary significantly. What works for one person may not work for another, making personal monitoring essential for success.
“The key to successfully including fruits in a diabetic fatty liver diet lies in careful selection, proper timing, and consistent monitoring. Small, strategic changes can make a significant difference in both blood sugar control and liver health.”
Practical Guide: Implementing Healthy Fruit Choices for Fatty Liver Recovery
Transforming scientific recommendations into daily habits can be challenging. Research published in Hepatology International shows that Following a regular diet plan with low-fructose fruits may lead to significant improvements in liver health.
7-Day Integration Plan for Fatty Liver Recovery
- Days 1-2: Preparation Phase – Remove high-fructose fruits – Stock recommended fruits – Set up tracking system
- Days 3-4: Introduction Phase – Begin with one serving of berries – Monitor body response – Track energy levels
- Days 5-7: Full Integration – Implement timing strategies – Add variety within guidelines – Establish regular patterns
Smart Shopping Guide for Liver-Friendly Fruits
According to The Lancet Gastroenterology & Hepatology, fruit quality significantly impacts its liver health benefits:
- Selection Tips – Choose organic when possible – Look for deep, rich colors – Avoid overripe fruits (higher sugar content)
- Seasonal Choices – Spring: Strawberries, blackberries – Summer: Blueberries, raspberries – Fall/Winter: Green apples, citrus
- Budget-Friendly Options – Buy frozen berries – Look for seasonal deals – Consider local markets
Storage Strategies for Maximum Benefits
Research in the Journal of Hepatology shows that proper storage can preserve beneficial compounds for liver health:
- Preparation Methods – Wash just before eating – Pre-portion for convenience – Store cut fruits properly
Success Strategies and Common Challenges
- Common Obstacles – Fruit cravings – Portion control – Timing consistency
- Solution Strategies – Prepare fruit portions in advance – Keep a consumption diary – Set reminder alarms for timing
While these guidelines provide a solid foundation, every person’s journey with fatty liver disease is unique. Individual factors such as current liver health, lifestyle, and other medical conditions can impact how you should implement these changes.
Evidence-Based Summary: Key Points About Fruits and Fatty Liver Disease
Research shows that making informed choices about fruit consumption can play a significant role in managing fatty liver disease. A 2024 study published in the Journal of Hepatology demonstrated that regular consumption of whole citrus fruits may help reduce hepatic steatosis when incorporated into a balanced diet.
Research-Backed Guidelines for Fruit Consumption
- Recommended Fruit Types – Low-fructose options: berries, citrus fruits – Whole fruits with natural fiber – Fresh rather than processed forms
- Fruits to Limit – Concentrated fruit products (juices, dried fruits) – High-fructose fruits (mangoes, grapes) – Sweetened fruit products
Evidence-Based Consumption Guidelines
According to research published in Frontiers in Nutrition (2024), successful fruit consumption in fatty liver disease involves:
- Consumption Patterns – Moderate intake of whole fruits – Combined with protein sources when possible – Part of a balanced, nutrient-rich diet
- Important Considerations – Individual tolerance varies – Monitor personal response – Adjust intake based on symptoms
Practical Implementation Steps
- Assessment – Identify current fruit consumption patterns – Remove concentrated fruit products – Stock recommended whole fruits
- Integration – Introduce low-fructose fruits gradually – Monitor body response – Adjust based on individual tolerance
- Long-term Management – Maintain moderate consumption – Focus on whole fruit options – Continue monitoring response
Additional Resources
- Scientific Literature – Current research findings – Clinical guidelines – Nutritional studies
- Monitoring Tools – Symptom tracking guides – Progress monitoring resources – Educational materials
Remember: Individual responses to fruit consumption can vary significantly. What works well for one person may need adjustment for another. Consider working with healthcare professionals to develop a personalized approach.
To access other content on the IFitCenter’s blog, you can use the following links:
References for Fatty Liver Fruits
- Zhang, Y., et al. (2024). Fruit and vegetable intake and the risk of non-alcoholic fatty liver disease: A systematic review and meta-analysis. Frontiers in Nutrition, 11. DOI: 10.3389/fnut.2024.1398184
- Notarnicola, M., et al. (2024). Daily Orange Consumption Reduces Hepatic Steatosis Prevalence in Patients with Metabolic Dysfunction-Associated Steatotic Liver Disease. Nutrients, 16(18), 3191. DOI: 10.3390/nu16183191
- Krawczyk, M., et al. (2014). Dietary recommendations for patients with nonalcoholic fatty liver disease. PMC, 6(3), 228–239. DOI: 10.5114/pg.2014.40845.
- Basaranoglu, M., et al. (2013). Fructose as a key player in the development of fatty liver disease. Frontiers in Pharmacology, 12. DOI: 10.3389/fphar.2021.634344
- World Health Organization (WHO). Healthy diet.
- European Society for Clinical Nutrition and Metabolism (ESPEN). (2023). Guidelines on clinical nutrition in liver disease.



