Do you frequently feel exhausted after meals, despite getting adequate sleep? Have you noticed darkened patches of skin around your neck or armpits that won’t go away? Are you struggling with unexplained hunger, despite eating regular meals? These seemingly unrelated issues could be your body’s way of signaling prediabetes—a critical metabolic state that precedes diabetes but often goes unrecognized.
What if you could identify prediabetes symptoms years before a doctor’s diagnosis, potentially preventing permanent damage to your health? Research shows that prediabetes typically develops over 10-15 years before progressing to diabetes, but 90% of those affected remain completely unaware of their condition until it’s too late.
Why do so many miss these warning signs? Unlike dramatic symptoms that send us rushing to emergency rooms, prediabetes symptoms often masquerade as everyday inconveniences. That tingling in your feet? Maybe it’s just from sitting too long. That increasing thirst? Perhaps it’s the weather. But what if these subtle changes are actually your body’s sophisticated warning system, alerting you to metabolic changes while they’re still reversible?
At IFitCenter, we’re tackling these important questions by exploring the full spectrum of prediabetes signs and symptoms. Understanding these warning signals isn’t just about preventing diabetes—it’s about recognizing an opportunity to restore metabolic balance before your body reaches the point of no return. Join us as we examine the ten key symptoms identified by medical research and explain why catching them early matters for your long-term health.
Understanding the Progression to Diabetes
Prediabetes doesn’t appear overnight. Instead, it develops gradually through a process that begins with insulin resistance—a condition where your body’s cells become less responsive to insulin, similar to how you might eventually tune out a car alarm that’s been going off too long. Your pancreas compensates by producing more insulin, just as you might raise your voice when someone isn’t listening to you.
This process typically unfolds in a predictable sequence:
- Phase 1: Initial Insulin Resistance – Your cells begin resisting insulin’s signals to absorb glucose
- Phase 2: Compensatory Insulin Increase – Your pancreas produces 5-7 times more insulin than normal to overcome this resistance
- Phase 3: Pancreatic Fatigue – After years of overproduction, the insulin-producing beta cells become exhausted
- Phase 4: Blood Sugar Rise – As insulin production can no longer keep pace with resistance, blood glucose levels begin to rise
What’s remarkable is that this entire process can take 10-15 years before blood sugar levels become noticeably elevated. During most of this time, your blood tests might show normal glucose levels despite significant metabolic dysfunction already occurring.
Diagnostic Criteria: The Numbers That Matter
Medical professionals diagnose prediabetes using specific blood test thresholds:
| Test | Normal | Prediabetes | Diabetes |
|---|---|---|---|
| Fasting Plasma Glucose (FPG) | Below 100 mg/dL | 100-125 mg/dL | 126 mg/dL or higher |
| Hemoglobin A1c (HbA1c) | Below 5.7% | 5.7-6.4% | 6.5% or higher |
| Oral Glucose Tolerance Test (OGTT) | Below 140 mg/dL | 140-199 mg/dL | 200 mg/dL or higher |
Think of these numbers as speedometer readings: normal is cruising at a safe speed, prediabetes is approaching the danger zone, and diabetes is exceeding the safety limit where damage occurs.
On the IFitCenter blog, we have prepared a comprehensive guide for pre-diabetes, completely free of charge. Using this guide will make controlling and preventing pre-diabetes much easier for you or your loved ones. To access the first part of the content, simply use the links below:
- what is prediabetes?
- how to test for prediabetes?
- can prediabetes be reversed?
- prediabetes natural remedies
- weight loss for prediabetes
- foods to avoid with prediabetes
The Critical Difference Between Prediabetes and Diabetes
The most crucial distinction between prediabetes and diabetes lies in reversibility. Prediabetes involves beta cell dysfunction—these insulin-producing cells in your pancreas aren’t working optimally, but haven’t suffered permanent damage yet. It’s like a strained muscle that can recover with proper care. Diabetes, however, represents irreversible beta cell damage, more like a torn muscle that can’t fully heal.
According to research published in the journal Diabetes Care, approximately 5-10% of people with prediabetes progress to type 2 diabetes annually. Without intervention, up to 70% will eventually develop diabetes in their lifetime. However, the American Diabetes Association notes that with appropriate lifestyle changes, progression can be reduced by 58%—significantly better than the 31% reduction achieved with medication alone.
This reversibility represents a crucial window of opportunity. During prediabetes, changes in diet, activity, and lifestyle can reverse the metabolic dysfunction before permanent damage occurs. This is why recognizing the symptoms early is so important—it allows intervention while the condition remains reversible.
The 10 Key Signs of Prediabetes
Recognizing prediabetes symptoms early can make the difference between reversing the condition or progressing to diabetes. While blood tests provide definitive diagnosis, your body often sends warning signals long before lab numbers reach concerning levels. Based on clinical research and medical expertise, here are 10 key signs and symptoms of prediabetes to be aware of:
Prediabetes Symptoms Darkened Skin (Acanthosis Nigricans)
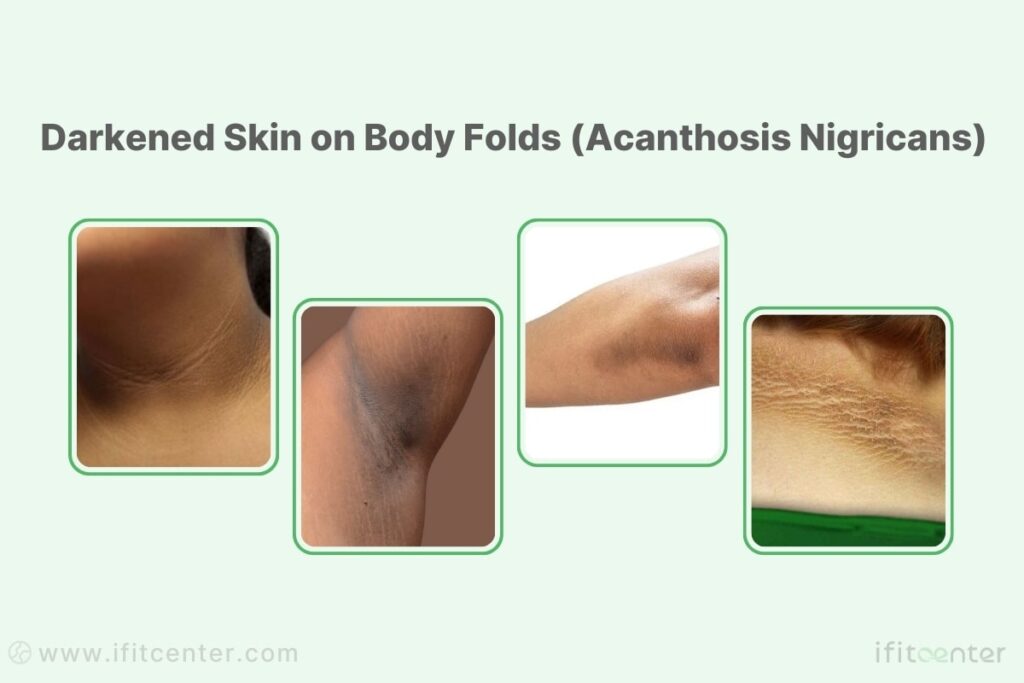
One of the most visible prediabetes skin symptoms appears as darkened, velvety patches of skin in body folds. This condition, called acanthosis nigricans, typically develops on the neck, armpits, and groin area.
The darkening occurs because elevated insulin levels stimulate skin cells to reproduce more rapidly. As insulin resistance develops and your body compensates by producing more insulin, these skin cells respond by creating pigmentation and thickening. Think of it as your skin visibly reacting to the excess insulin circulating in your bloodstream.
How to distinguish acanthosis nigricans from other skin conditions:
- Location: Primarily appears in skin folds and creases
- Texture: Velvety or slightly raised, not scaly or itchy
- Color: Usually brown or black, darker than surrounding skin
- Symmetry: Often appears on both sides of the body
According to research published in the Annals of Dermatology, approximately 74% of people with prediabetes or type 2 diabetes exhibit some degree of acanthosis nigricans. This makes it one of the most reliable visual indicators of insulin resistance, appearing often years before blood glucose levels become elevated.
Memory Issues and Cognitive Changes Warning Symptoms of Prediabetes
Do you frequently misplace items, forget appointments, or struggle to focus on tasks? These cognitive symptoms might not be just normal aging or stress – they could be early signs of prediabetes affecting your brain function.
The brain is highly dependent on proper glucose metabolism. Insulin resistance affects how your brain cells (neurons) receive energy, impairing cognitive processes. Research published in Diabetes Care demonstrates that insulin resistance can reduce cerebral glucose metabolism by up to 15% in key brain regions responsible for memory and executive function.
Specific cognitive symptoms that may indicate prediabetes include:
- Increased forgetfulness (misplacing keys, forgetting where you parked)
- Difficulty maintaining focus on tasks or conversations
- Mild confusion or mental “fogginess”
- Reduced verbal fluency or word-finding difficulties
- Decreased ability to plan or organize tasks
Studies show that people with prediabetes perform about 12% worse on cognitive tests compared to those with normal blood sugar levels. More concerning, these cognitive changes often begin during the insulin resistance phase, before blood glucose levels become elevated enough for a prediabetes diagnosis.
Post-Meal Fatigue: Prediabetes Symptoms Fatigue
Feeling unusually tired or sleepy after meals – particularly carbohydrate-rich ones – is a significant but often overlooked symptom of prediabetes. While it’s normal to feel slightly less energetic after eating, pronounced fatigue or the need to nap after meals is not typical and warrants attention.
This fatigue occurs due to glucose metabolism disruption. In a metabolically healthy person, blood sugar rises moderately after eating, then insulin helps cells absorb that glucose efficiently for energy. With insulin resistance, your cells can’t properly take up glucose despite rising insulin levels. This creates a paradoxical situation where blood sugar fluctuates dramatically while cells remain energy-deprived.
Post-meal fatigue in prediabetes typically follows this pattern:
- Initial energy while eating (due to rising blood glucose)
- Pronounced fatigue 1-2 hours after carbohydrate-rich meals
- Strong urge to nap, particularly after lunch
- Difficulty concentrating during this post-meal window
“What many patients find surprising is that post-meal fatigue isn’t just about feeling tired—it’s a metabolic alarm signal. When someone consistently needs to nap after meals, especially carbohydrate-rich ones, their cells are essentially starving for energy despite having plenty of glucose in the bloodstream. This paradox occurs because insulin resistance prevents glucose from entering cells efficiently. I’ve observed that this symptom often appears 3-5 years before blood tests show abnormal glucose levels, making it one of our most valuable early detection tools.”
Dr. Babak Jamalian, Family Physician Specialist.
Abdominal Fat Accumulation
The pattern of where your body stores fat can be a visible sign of metabolic dysfunction. Specifically, excess fat around your abdomen—what medical professionals call central or visceral adiposity—strongly correlates with insulin resistance and prediabetes.
Unlike subcutaneous fat (the kind you can pinch), visceral fat surrounds your internal organs and produces inflammatory compounds that actively worsen insulin resistance. This creates a dangerous cycle: insulin resistance promotes visceral fat storage, which then produces inflammation that further impairs insulin sensitivity.
To identify if your abdominal fat might indicate prediabetes:
- Waist circumference: For women, greater than 35 inches (88 cm) indicates risk; for men, greater than 40 inches (102 cm)
- Waist-to-hip ratio: Values above 0.85 for women and 0.9 for men suggest unhealthy fat distribution
- Visual assessment: Looking down and being unable to see your feet while standing
According to a meta-analysis published in Diabetes Care examining over 500,000 individuals, people with significant central obesity have a 3.5-fold higher risk of developing prediabetes regardless of their total body weight. Even more striking, research from the American Diabetes Association shows that approximately 84% of people with prediabetes have excess visceral fat, making this one of the most common physical manifestations of insulin resistance.
Frequent Hunger and Carbohydrate Cravings
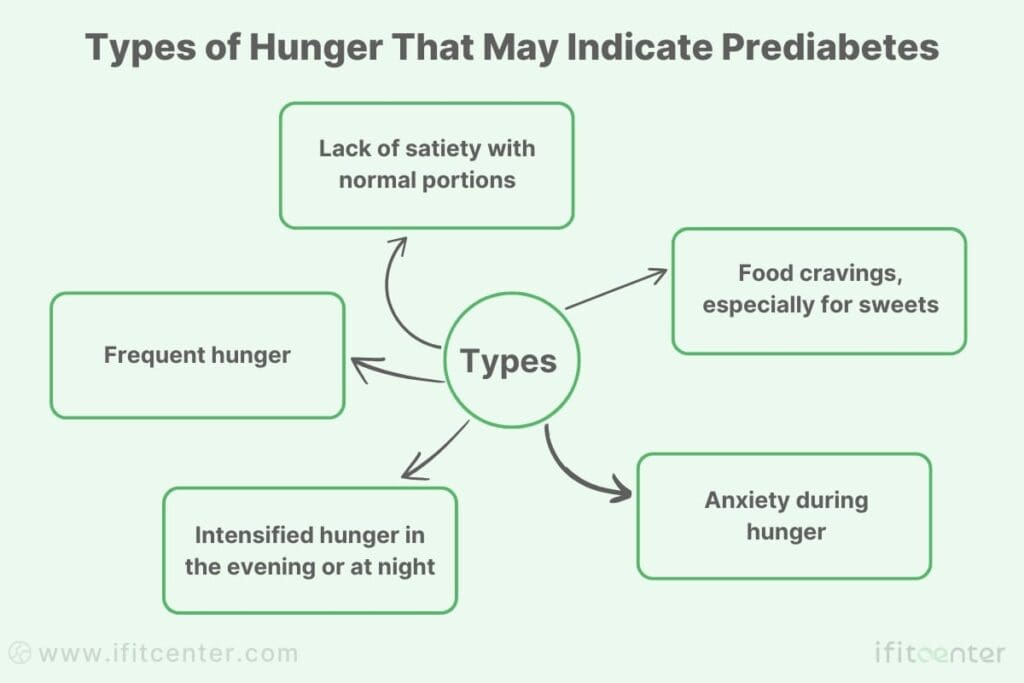
If you find yourself unable to go more than 2-3 hours without feeling hungry or experiencing intense cravings for carbohydrate-rich foods, your body may be signaling insulin resistance—a hallmark of prediabetes.
This symptom stems from a cellular energy crisis. Despite consuming adequate or even excess calories, your cells struggle to access glucose due to insulin resistance. This creates a mismatch: high blood glucose and insulin levels circulating in your bloodstream, yet cellular starvation at the same time. Your brain, detecting this energy deficit, triggers hunger signals and specific cravings for quick-energy carbohydrates.
Research-identified patterns of hunger in prediabetes include:
- Inability to feel satisfied after normal-sized meals
- Recurring hunger within 2-3 hours of eating
- Specific cravings for bread, pasta, sweets, or starchy foods
- Evening/nighttime hunger intensification
- Feeling irritable or anxious when hungry (“hangry”)
Clinical studies published in the Journal of Clinical Investigation have demonstrated that people with insulin resistance experience a 50-65% faster return of hunger after standardized meals compared to metabolically healthy individuals. This accelerated hunger cycle often leads to frequent snacking, which further elevates insulin levels and worsens insulin resistance, creating a vicious cycle.
Slow Wound Healing in Prediabetes
If you’ve noticed that cuts, scrapes, or other minor injuries take longer than usual to heal, this could be an early warning sign of prediabetes. This seemingly unrelated symptom has a direct connection to how your body processes glucose.
When blood sugar levels remain consistently elevated, even slightly, it impairs the healing process in multiple ways. First, higher glucose levels stiffen blood vessels and reduce circulation to injured areas. Second, elevated blood sugar interferes with the function of white blood cells that fight infection and coordinate tissue repair. Third, the proteins needed for wound healing become damaged through a process called glycation when exposed to excess glucose.
Signs that your wounds may be healing abnormally slowly:
- Minor cuts or scrapes taking more than 7-10 days to close
- Lingering redness or swelling beyond the initial injury phase
- Wounds that begin healing but then stall in progress
- Frequent infections in small injuries
Increased Urination and Thirst
Frequent urination, especially at night (nocturia), combined with persistent thirst, represents a classic but often overlooked warning sign of prediabetes. While many people attribute these changes to aging, medication side effects, or drinking habits, they can actually signal developing insulin resistance.
The physiological mechanism behind this symptom involves your kidneys’ response to blood glucose levels. Normally, your kidneys filter glucose and reabsorb it completely. However, as blood glucose begins rising—even slightly above optimal range—the kidneys’ capacity to reabsorb glucose becomes overwhelmed. This results in glucose spilling into the urine, drawing water with it through a process called osmotic diuresis.
This process creates a cascade effect:
- Elevated blood glucose exceeds kidney reabsorption threshold
- Glucose spills into urine, pulling water with it
- Increased urine production leads to frequent urination
- Water loss triggers thirst mechanisms
- Increased fluid intake further increases urination frequency
Nighttime urination is particularly significant as a prediabetes warning sign. Research published in Diabetes Care found that people who wake up to urinate two or more times per night have a 40% higher likelihood of having undiagnosed prediabetes compared to those who sleep through the night. This connection is strong enough that the American Diabetes Association now recommends blood glucose screening for individuals reporting new or worsening nocturia without other obvious causes.
Skin Changes: Dryness and Itching
Beyond the darkened skin patches of acanthosis nigricans, prediabetes can cause several other skin symptoms that many people fail to connect with blood sugar issues. Persistent skin dryness and unexplained itching often serve as early signs of prediabetes that affect quality of life well before diabetes develops.
These skin changes occur through several mechanisms. First, elevated blood glucose alters the skin’s natural moisture barrier through glycation—a process where sugar molecules attach to proteins in skin tissues, damaging their normal function. Second, mild dehydration from increased urination reduces skin moisture. Third, reduced microcirculation to skin tissues limits nutrient delivery and waste removal, further compromising skin health.
Common prediabetes-related skin symptoms include:
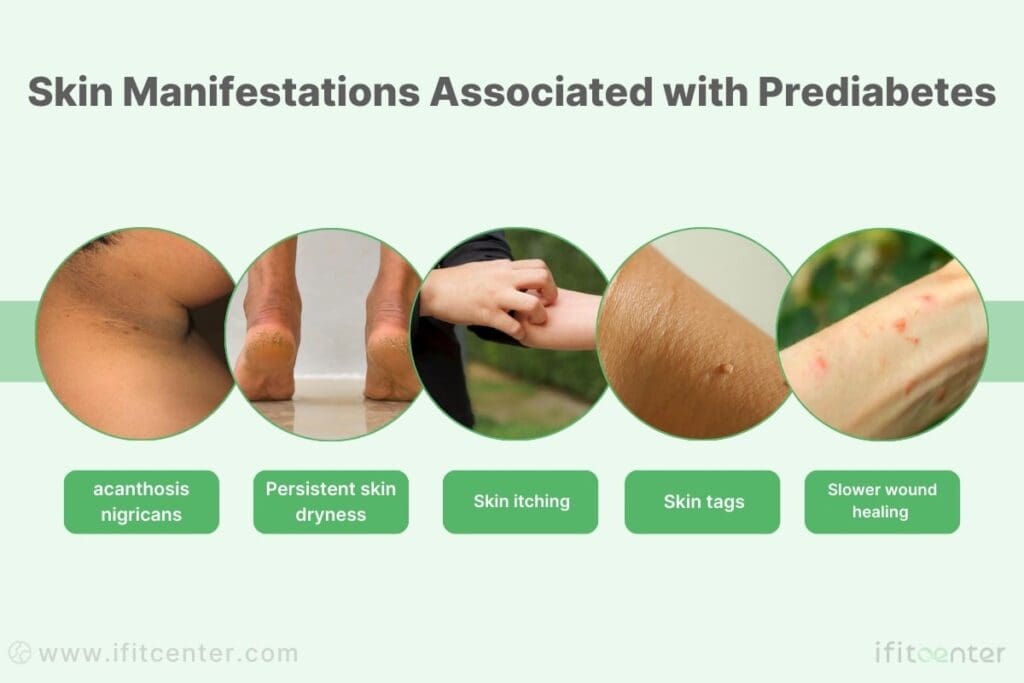
- Persistent dryness despite moisturizing (especially on lower legs and feet)
- Unexplained itching without visible rash (pruritus)
- Skin tags (small flesh-colored growths) appearing on neck, armpits, or groin
- Slower healing of minor skin irritations
A systematic review in the Journal of the European Academy of Dermatology and Venereology found that approximately 63% of individuals with prediabetes experience at least one abnormal skin condition related to their glucose metabolism, with itching being the most commonly reported symptom (affecting about 49% of prediabetic patients). Most notably, these skin changes often appear years before other more recognized symptoms of blood sugar dysfunction.
Vision Changes
Subtle changes in vision quality can serve as an important early warning sign of prediabetes. While many dismiss minor vision fluctuations as normal aging or eye strain, these changes often reflect how elevated blood glucose affects the delicate tissues of the eye.
Even modest elevations in blood sugar affect vision through several mechanisms. First, the lens of the eye is rich with glucose-absorbing aquaporin proteins that change shape when exposed to excess glucose, altering the lens’s refractive properties. Second, mild glucose fluctuations cause fluid shifts in the eye tissues, changing intraocular pressure. Third, early microvascular damage to retinal blood vessels occurs even in prediabetes, affecting visual processing.
Specific vision symptoms that may indicate prediabetes include:
- Fluctuating visual clarity throughout the day
- Temporary blurred vision, especially after high-carbohydrate meals
- Difficulty adapting to changes in lighting conditions
- New or worsening difficulty with night vision
- Seeing occasional “floaters” or spots in your field of vision
What distinguishes these changes from normal age-related vision decline is their fluctuating nature—often better in the morning and worse after meals or at the end of the day. In contrast, age-related changes tend to be more stable and consistent throughout the day.
Tingling and Numbness in Extremities
Experiencing intermittent tingling, numbness, or burning sensations in your hands, feet, or legs represents one of the most serious early warning signs of prediabetes. These sensations, technically known as peripheral neuropathy, signal that elevated blood glucose is beginning to affect your peripheral nervous system.
Contrary to conventional medical understanding, research now confirms that neuropathy often begins during prediabetes, not just after diabetes develops. Even mild but persistent elevation in blood glucose can damage the small blood vessels (vasa nervorum) that supply peripheral nerves. This microvascular injury, combined with direct glucose toxicity to nerve fibers, leads to nerve dysfunction that you experience as abnormal sensations.
How early prediabetic neuropathy typically presents:
- Intermittent (rather than constant) symptoms
- Often worse at night or when resting
- Typically begins in the feet and progresses upward symmetrically
- May include sensations of “pins and needles,” burning, or sensitivity to touch
- Often described as feeling like wearing invisible socks or gloves
The presence of neuropathic symptoms should prompt immediate medical evaluation, as it represents one of the clearest indicators that prediabetes is advancing toward more serious complications.
Reversing Prediabetes Through Medical Weight Management
Prediabetes is a critical warning sign, but it’s also an opportunity for intervention. Excess weight and insulin resistance are closely linked, making targeted weight loss one of the most effective ways to restore metabolic balance and prevent diabetes.
At IFitCenter, under the expert supervision of Dr. Babak Jamalian, we provide a medically guided weight management program tailored to lower insulin resistance, stabilize blood sugar levels, and reduce diabetes risk. Take control of your health today—our team is here to guide you toward lasting metabolic improvement.
Gender-Specific Prediabetes Symptoms
While the core metabolic processes of prediabetes affect everyone, how these changes manifest can differ significantly between men and women. These gender-specific variations occur due to differences in hormonal environments, body composition, and physiological responses to insulin resistance. Understanding these distinctions can help you identify symptoms that might otherwise be attributed to gender-specific health concerns rather than underlying prediabetes.
To access the second part of pre-diabetes content, I invite you to use the links below:
- pre-diabetic supplement
- best intermittent fasting for prediabetes?
- difference between prediabetic and diabetic
- vitamin d prediabetes
- prediabetes and obesity
- blood sugar number
- hba1c test
- Which oil is good for cholesterol
Symptoms of Prediabetes in Females
Women often experience a unique constellation of prediabetes symptoms due to the complex interplay between insulin and female reproductive hormones. Estrogen typically enhances insulin sensitivity, while progesterone can promote insulin resistance. This hormonal dance creates distinctive patterns of symptom presentation that women should be particularly aware of.
Research published in the Journal of Clinical Endocrinology and Metabolism has found that women with prediabetes commonly experience these prediabetes symptoms in females:
- Menstrual irregularities – Many women with undiagnosed prediabetes report changes in their menstrual cycle. This includes longer menstrual cycles, heavier bleeding, or more significant premenstrual symptoms.
- Recurrent yeast infections – Even slightly elevated blood glucose can increase vaginal glucose levels, creating an environment where yeast thrives. Women with prediabetes frequently experience more vaginal yeast infections than those with normal blood sugar.
- Hormonal acne – Insulin resistance increases androgen production and activity in women, leading to adult-onset acne, typically along the jawline and chin.
- Hair growth changes – The same androgen imbalance can cause increased facial and body hair growth (hirsutism) and/or thinning of scalp hair in women with prediabetes.
Perhaps the most significant connection exists between prediabetes and Polycystic Ovary Syndrome (PCOS). PCOS and prediabetes share a bidirectional relationship: insulin resistance is both a cause and consequence of PCOS. According to research in the journal Metabolism, a substantial majority of women with PCOS have measurable insulin resistance, and many display prediabetes symptoms before receiving either diagnosis.
For women of reproductive age, prediabetes also presents unique pregnancy-related concerns. Studies in Obstetrics & Gynecology demonstrate that women with undiagnosed prediabetes have:
- Significantly higher risk of gestational diabetes during pregnancy
- Increased risk of pregnancy-induced hypertension
- Higher likelihood of unexplained fertility challenges
Most concerning is that many women dismiss these symptoms as normal hormonal fluctuations rather than recognizing them as potential indicators of metabolic dysfunction. Research published in Women’s Health Issues found that women typically experience a substantial delay between first experiencing prediabetes symptoms and receiving proper diagnosis—notably longer than the average delay for men.
Signs of Prediabetes in Males
Men with prediabetes often display a different pattern of symptoms compared to women, largely due to testosterone’s complex relationship with insulin sensitivity. While optimal testosterone levels actually improve insulin sensitivity in men, insulin resistance itself can lower testosterone production, creating a problematic cycle that produces distinct symptoms in men.
According to research published in the Journal of Clinical Endocrinology and Metabolism, men with prediabetes frequently report these male-specific symptoms:
- Erectile dysfunction (ED) – This is perhaps the most significant early warning sign in men. Studies in Diabetes Care demonstrate that many men with undiagnosed prediabetes report some degree of erectile difficulty—often years before receiving a prediabetes diagnosis. This occurs because insulin resistance damages the small blood vessels and nerves critical for erectile function.
- Decreased morning erections – Even before full ED develops, a reduction in normal morning erections can signal developing insulin resistance.
- Reduced muscle mass despite regular activity – Insulin resistance interferes with protein synthesis and muscle development. Men with prediabetes often have less muscle mass than metabolically healthy men with similar activity levels.
- Sleep apnea – While this affects both sexes, men with prediabetes have a substantially higher prevalence of sleep apnea compared to metabolically healthy men, independent of BMI.
Testosterone plays a crucial role in this metabolic picture. Research published in the European Journal of Endocrinology has found that insulin resistance can significantly reduce testosterone production in men even before full diabetes develops. This creates a cascade of symptoms that many men incorrectly attribute solely to “low T” rather than underlying metabolic dysfunction.
Compared to women, men with prediabetes are more likely to develop central (abdominal) obesity. This fat distribution pattern both contributes to and results from the relationship between testosterone and insulin.
Perhaps most significantly, men demonstrate a different pattern of symptom awareness. Studies published in the American Journal of Men’s Health indicate that men are substantially less likely than women to attribute erectile difficulties, fatigue, or increased thirst to a potential metabolic health issue, often dismissing these symptoms until they become severe.
Self-Assessment: When to Seek Testing
Based on clinical guidelines from the American Diabetes Association, consider requesting blood sugar testing if you:
- Experience multiple symptoms described in this article
- Have a family history of type 2 diabetes
- Are over 35 with BMI over 25 (or over 23 for Asian Americans)
- Previously had gestational diabetes or gave birth to a baby over 9 pounds
- Have been diagnosed with PCOS, sleep apnea, or cardiovascular disease
- Have previously had an HbA1c of 5.5% or higher, even if it was considered “normal”
The most thorough assessment includes multiple tests – fasting glucose, HbA1c, and when possible, an oral glucose tolerance test – as research shows using multiple methods captures more cases than relying on a single test.
The Window of Reversibility
Unlike diabetes, which typically involves permanent damage to pancreatic beta cells, prediabetes represents a critical window where metabolic health can be restored. Research published in the New England Journal of Medicine has demonstrated that appropriate lifestyle modifications can reduce the risk of prediabetes progressing to diabetes by more than half.
The key elements that research has shown to effectively reverse prediabetes include:
- Dietary modifications – Reducing refined carbohydrates and focusing on protein, healthy fats, and fiber-rich foods
- Activity patterns – Incorporating both resistance and cardiovascular exercise into weekly routines
- Stress management – Addressing chronic stress through proven techniques like mindfulness or adequate sleep
- Environmental factors – Minimizing exposure to endocrine-disrupting chemicals and prioritizing quality sleep
What makes these approaches so effective is that they target the root cause – insulin resistance – rather than simply managing symptoms or blood sugar levels. By restoring cellular insulin sensitivity, many of the symptoms described throughout this article often improve or resolve completely.
A Message of Metabolic Hope
If you’ve recognized several prediabetes symptoms in yourself, view this as an opportunity rather than a cause for despair. The Diabetes Prevention Program research study demonstrated that people who took action during the prediabetes stage not only prevented diabetes but often restored normal blood sugar metabolism.
Even better, improvement begins quickly. Research from the Journal of Endocrinology shows that cellular insulin sensitivity can begin improving within days of dietary changes, with many prediabetes symptoms starting to resolve within weeks – long before significant weight loss or changes to diagnostic blood markers.
Your body’s ability to heal is remarkable when given the right environment. By recognizing these early warning signs and taking appropriate action, you’re not just avoiding diabetes – you’re reclaiming optimal metabolic health and all the energy, clarity, and vitality that comes with it.
If you’re concerned about prediabetes symptoms you’re experiencing, consider downloading our free Prediabetes Risk Assessment Guide, which includes a symptom tracker and personalized recommendations based on your specific symptom pattern. Early recognition paired with appropriate action truly can change the trajectory of your long-term health.
To access other content on the IFitCenter’s blog, you can use the following links:
References for “Prediabetes Signs and Symptoms”
- American Diabetes Association. Standards of Medical Care in Diabetes—2023. Diabetes Care. 2023;46(Supplement 1):S1-S28. DOI: 10.2337/dc23-Sint
- Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. The Lancet. 2012;379(9833):2279-2290. DOI: 10.1016/S0140-6736(12)60283-9
- Hostalek U. Global epidemiology of prediabetes – present and future perspectives. Clinical Diabetes and Endocrinology. 2019;5:5. DOI: 10.1186/s40842-019-0080-0
- Bansal N. Prediabetes diagnosis and treatment: A review. World Journal of Diabetes. 2015;6(2):296-303. DOI: 10.4239/wjd.v6.i2.296
- Echouffo-Tcheugui JB, Selvin E. Prediabetes and What It Means: The Epidemiological Evidence. Annual Review of Public Health. 2021;42:59-77. DOI: 10.1146/annurev-publhealth-090419-102644



