Do you find yourself rushing to the bathroom multiple times during the night? Are you constantly thirsty regardless of how much water you drink? Have you noticed unexplained weight loss despite your appetite increasing? These aren’t just random inconveniences – they could be your body sounding the alarm about a serious condition. These are classic signs and symptoms of diabetes, a condition affecting millions worldwide, yet often overlooked until complications arise.
What makes recognizing these symptoms so critical is that diabetes can remain silent for years, with nearly half of all cases going undiagnosed. The American Diabetes Association reports that of the approximately 37.3 million Americans with diabetes, a shocking 8.5 million remain undiagnosed, unaware that their blood sugar levels are gradually damaging their bodies. By learning to identify the signs and symptoms of diabetes early, you gain valuable time to take control of your health before complications develop.
In this comprehensive guide at IFitCenter, we’ll examine the complete spectrum of diabetes symptoms – from the well-known warning signs shared by both type 1 and type 2 diabetes to the gender-specific indicators and unique manifestations in children that often go unrecognized. Understanding these crucial signals could make all the difference between early intervention and dealing with serious health complications down the road.
Common Symptoms of Type 1 and Type 2 Diabetes
Despite their different underlying causes, Type 1 and Type 2 diabetes share many common symptoms. These warning signs occur because of one central problem: when glucose can’t enter your cells properly, it builds up in your bloodstream, triggering a cascade of effects throughout your body. Recognizing these symptoms early can lead to prompt diagnosis and better health outcomes.
The Classic “Three Ps” of Diabetes
Healthcare professionals often refer to the “three Ps” as the cardinal signs of diabetes. These symptoms are so closely associated with diabetes that their presence should prompt immediate medical attention:
- Polydipsia (Excessive Thirst): When your blood sugar rises, your kidneys work overtime to filter and absorb the excess glucose. When they can’t keep up, this excess glucose is excreted into your urine, dragging along fluids from your tissues. This makes you dehydrated, triggering intense thirst that seems unquenchable. It’s not just the occasional desire for water after exercise—imagine feeling parched even after drinking several glasses of water.
- Polyuria (Frequent Urination): As your kidneys expel the excess glucose through urine, you’ll find yourself urinating more frequently—including during the night (nocturia). Many people describe having to map out bathroom locations whenever they go somewhere new, or waking up multiple times nightly to urinate, disrupting their sleep.
- Polyphagia (Increased Hunger): Despite having high blood glucose levels, your cells are effectively starving. Without insulin working properly, glucose remains in your bloodstream instead of moving into your cells for energy. Your body responds by triggering hunger signals, creating a frustrating situation where you feel constantly hungry despite eating normal or even increased amounts of food.
These three symptoms often appear together and create a troubling cycle: you drink more, which leads to more urination, which triggers more thirst, all while feeling increasingly hungry.
Fatigue and Weakness
Persistent fatigue is one of the most commonly reported symptoms of diabetes, yet often one of the most overlooked. This isn’t the typical tiredness after a poor night’s sleep—it’s a profound exhaustion that doesn’t improve with rest.
When your cells can’t access glucose for energy, your body becomes less efficient at everything it does. Simple tasks may leave you winded, you might notice decreased physical endurance, or find yourself needing afternoon naps just to get through the day. Many people describe this fatigue as feeling like “running on empty” or as if they’re “moving through molasses.”
Unexplained Weight Loss
Losing weight without trying might seem like a welcome surprise, but when it occurs alongside other diabetes symptoms, it signals a problem. This is particularly common in Type 1 diabetes but can occur in uncontrolled Type 2 diabetes as well.
When glucose can’t enter your cells, your body thinks it’s starving. In response, it begins breaking down fat stores and muscle tissue for energy, resulting in weight loss despite normal or even increased food intake. Some individuals report losing 10-20 pounds over just a few months without any changes to their diet or exercise habits—a red flag that warrants medical attention.
Blurred Vision
Vision changes can be particularly alarming and are often what finally prompts someone to seek medical care. High blood glucose levels affect your eyes by changing fluid levels, causing the lenses to swell and change shape. This alters how light is focused inside your eye, resulting in blurred vision.
Many people describe this as difficulty focusing, especially when switching from looking at something close-up to something far away. Some notice they suddenly need to hold reading material further away to see it clearly. These changes may fluctuate throughout the day as blood sugar levels rise and fall.
On the IFitCenter blog, we have provided a comprehensive guide for diabetes, completely free of charge and based on the latest research. By viewing these articles, in addition to increasing your general knowledge in this field, you can easily manage this disease in a principled manner. To access the first part of the articles, simply use the links below:
- What is Diabetes?
- Difference Between Type 1 and Type 2 Diabetes
- What Are the Complications of Diabetes?
- Diabetes Diagnosis Method
- Can Diabetes Be Cured?
- Does Obesity Cause Diabetes?
Slow-Healing Wounds
Do paper cuts linger for weeks? Does a small scrape refuse to heal? Elevated blood sugar impairs your body’s natural healing processes in several ways. It reduces blood flow to tissues, weakens immune system function, and creates an inflammatory environment that interferes with repair mechanisms.
This slow healing is most noticeable in extremities like feet and legs, where circulation might already be compromised. Even minor injuries—blisters from new shoes, small cuts from grooming—may take weeks longer to heal than they would in someone without diabetes. This delayed healing also increases infection risk, creating a dangerous cycle.
Frequent Infections
High blood sugar creates an ideal environment for bacterial and fungal growth while simultaneously weakening your immune response. The result? More frequent, more severe, and longer-lasting infections.
Common infection patterns that may signal diabetes include:
- Recurring urinary tract infections
- Frequent yeast infections (vaginal thrush in women, jock itch in men)
- Skin infections like boils, styes, or nail infections
- Persistent gum disease despite good oral hygiene
- Fungal infections, especially in warm, moist areas like between toes (athlete’s foot)
These infections often respond slower to standard treatments and may return quickly after treatment ends.
Classic Symptoms of Hyperglycemia (High Blood Sugar)
Beyond the classic symptoms, high blood sugar can manifest in additional ways that might not immediately suggest diabetes:
- Dry, itchy skin: Dehydration from excess urination can leave skin dry and prone to itching
- Headaches: Fluctuating blood glucose levels can trigger headaches similar to those experienced when skipping meals
- Difficulty concentrating: Your brain relies heavily on glucose for fuel; when levels fluctuate dramatically, cognitive function can suffer
- Recurrent skin problems: Conditions like acanthosis nigricans (dark, velvety skin patches typically in body folds) can signal insulin resistance
- Fruity-smelling breath: In severe hyperglycemia, your body produces ketones that create a distinctive fruity breath odor—a warning sign requiring immediate medical attention
Symptoms of Low Blood Sugar (Hypoglycemia)
While diabetes primarily involves high blood sugar, people with diabetes (especially those on certain medications) can also experience dangerously low blood sugar levels. Recognizing hypoglycemia symptoms is crucial, as this condition can quickly become life-threatening:
- Sudden shakiness or trembling: Often one of the first noticeable signs
- Sweating, chills, or clamminess: Your body’s stress response activating
- Irritability or sudden mood changes: Low glucose affects brain function, often manifesting as mood swings
- Anxiety or nervousness: Another result of your body’s stress hormones responding to falling glucose
- Confusion or difficulty speaking: Brain cells failing to receive adequate glucose
- Hunger or nausea: Your body sending mixed signals about needing fuel
- Weakness, dizziness, or light-headedness: Lack of cellular energy affecting physical function
- Sleepiness: The brain conserving energy when glucose levels fall
- Headache: Common when brain cells are deprived of their primary fuel source
In severe cases, hypoglycemia can progress to seizures, loss of consciousness, or even coma if not treated promptly. Anyone with diabetes should be familiar with these warning signs and have a plan for addressing low blood sugar episodes.
Recognizing these common symptoms of diabetes is the first step toward diagnosis and treatment. If you’re experiencing any combination of these symptoms, especially the “three Ps,” consulting with a healthcare provider for proper testing is essential. Early detection can make all the difference in managing diabetes effectively and preventing serious complications.
Specific Symptoms of Type 1 Diabetes
While Type 1 and Type 2 diabetes share many symptoms, Type 1 diabetes has distinct characteristics that set it apart. Type 1 diabetes results from an autoimmune process where the body’s immune system mistakenly attacks insulin-producing beta cells in the pancreas, leading to an absolute insulin deficiency.
To access the second part of the articles related to diabetes, you can use the following links:
- The Difference Between Prediabetes and Diabetes
- Insulin Resistance and Diabetes
- Understanding Blood Sugar Numbers
- Weight Loss for Type 2 Diabetes
- Type 1 Diabetes
- What is HbA1C test?
- The Relationship Between Genetics and Diabetes
Rapid Onset of Symptoms
Unlike Type 2 diabetes, which typically develops gradually over years, Type 1 diabetes symptoms often appear suddenly and progress rapidly, sometimes over just a few weeks or months. This quick onset can be alarming and is often what prompts immediate medical attention.
Many patients or their parents report a distinct “before and after” moment – a child who was perfectly healthy suddenly becomes constantly thirsty, starts wetting the bed again, and rapidly loses weight despite eating well.
Signs of Diabetic Ketoacidosis (DKA)
One of the most dangerous aspects of Type 1 diabetes is the risk of diabetic ketoacidosis (DKA), a potentially life-threatening condition that can occur at diagnosis or during times of illness. When the body cannot use glucose for energy due to insulin deficiency, it breaks down fat too quickly, producing ketones that make the blood acidic.
Warning signs of DKA include:
- Fruity-smelling breath – often described as similar to nail polish remover or fruit
- Deep, rapid breathing (Kussmaul respiration) – the body attempting to remove excess acid
- Nausea and vomiting – often mistaken for stomach flu
- Stomach pain – frequently in the abdominal area
- Confusion or difficulty concentrating – as the brain is affected by ketones
- Extreme fatigue – beyond typical tiredness
DKA requires immediate emergency medical attention and is often the event that leads to a Type 1 diabetes diagnosis.
Dramatic Weight Loss
While weight loss can occur in both types of diabetes, it’s particularly pronounced in Type 1. Even with increased hunger and food intake, people with undiagnosed Type 1 diabetes often experience significant, rapid weight loss as the body breaks down fat and muscle tissue for energy it cannot get from glucose.
This weight loss can be dramatic – some patients report losing 10-20 pounds within a few weeks, which is especially noticeable in children and lean adults who don’t have much weight to lose. Parents might notice a child’s clothes suddenly becoming loose or ribs becoming visible despite normal or even increased eating.
Key Differences from Type 2 Diabetes Symptoms
Several features help distinguish Type 1 from Type 2 diabetes symptoms:
- Age at onset – Type 1 is more commonly diagnosed in children and young adults, though it can develop at any age
- Body type – Type 1 often develops in people with normal or thin body types, unlike Type 2 which is more commonly (though not exclusively) associated with overweight or obesity
- Symptom intensity – Type 1 symptoms are typically more severe and develop more quickly
- DKA risk – Much higher in Type 1 diabetes, especially at diagnosis
- Response to lifestyle changes – Type 1 symptoms will not improve with lifestyle modifications alone, unlike some cases of Type 2
Age-Related Symptom Presentation
Type 1 diabetes symptoms can present differently depending on age:
In Young Children (under 5)
Very young children may not be able to express thirst or other symptoms verbally. Parents might notice:
- Increased wet diapers or bedwetting in toilet-trained children
- Extreme irritability or mood changes
- Lethargy or unusual sleepiness
- Sudden weight loss making ribs visible
- Sweet or fruity smell on the breath
In School-Age Children
- Declining school performance due to difficulty concentrating
- Increased bathroom breaks during class
- Constant hunger and thirst
- Fatigue affecting sports or play activities
In Teens and Young Adults
- Performance issues in sports or studies
- Extreme fatigue mistaken for depression or stress
- Vision changes affecting driving or reading
- Recurrent infections or slow healing
In Adults Over 30 (“LADA” or Latent Autoimmune Diabetes in Adults)
- May initially resemble Type 2 diabetes but fail to respond to oral medications
- More gradual onset than childhood Type 1, but more rapid than typical Type 2
- Progressive worsening despite lifestyle improvements
Specific Symptoms of Type 2 Diabetes
Type 2 diabetes develops when the body becomes resistant to insulin or when the pancreas cannot produce enough insulin to overcome this resistance. Unlike Type 1 diabetes, the symptoms of Type 2 often develop gradually and can be subtle enough to go unnoticed for years.
Gradual Development of High Blood Sugar Symptoms
While Type 1 diabetes often appears suddenly, Type 2 diabetes typically develops slowly over time. Blood sugar levels rise gradually, allowing the body to partially adapt, which means early symptoms may be mild or dismissed as normal aging. Many people have Type 2 diabetes for years before receiving a diagnosis.
The classic diabetes symptoms—increased thirst, frequent urination, and increased hunger—still occur in Type 2 diabetes, but they usually appear more gradually and might not be as intense as in Type 1. This slower progression can delay diagnosis and treatment, allowing complications to develop.
Symptoms Often Mistaken for Aging
Many Type 2 diabetes symptoms overlap with what people consider normal signs of aging, making them easy to overlook:
- Increasing fatigue: Often attributed to “just getting older” rather than recognized as a blood sugar issue
- Vision changes: Might be dismissed as normal age-related vision decline instead of diabetes-related changes
- Increased urination at night: Many assume this is a natural part of aging or, in men, related to prostate issues
- Slower healing: Cuts and scrapes taking longer to heal might be considered normal for older adults
- Weight changes: Unlike the weight loss common in Type 1, Type 2 may cause either weight loss or gain, which might be attributed to metabolism changes with age
Early Warning Signs Often Missed
Before the classic symptoms of diabetes become obvious, several subtle warning signs might appear:
- Recurrent infections: Particularly urinary tract, skin, or gum infections that seem to occur more frequently or take longer to resolve
- Increased drowsiness after meals: Feeling unusually tired or needing to nap after eating, especially carbohydrate-heavy meals
- Irritability or mood changes: Blood sugar fluctuations can affect mood and mental clarity
- Dry mouth and itchy skin: Early signs of the dehydration caused by excess urination
- Changes in hunger patterns: Either increased hunger or loss of appetite
Don’t Ignore the Subtle Signs—Take Action for Your Health
Early signs of diabetes, such as fatigue, gradual weight changes, and frequent infections, can often be mistaken for ordinary issues or normal aging. However, these subtle symptoms may indicate developing insulin resistance or diabetes, both strongly linked to excess weight and lifestyle factors.
At iFitCenter, our medically supervised weight-loss and lifestyle programs are specifically designed to address these underlying metabolic issues. With personalized nutritional guidance and comprehensive metabolic assessments, we help you manage your weight effectively, improve insulin sensitivity, and prevent diabetes complications from developing.
Recognize the signs early and regain control of your health—schedule your consultation today.
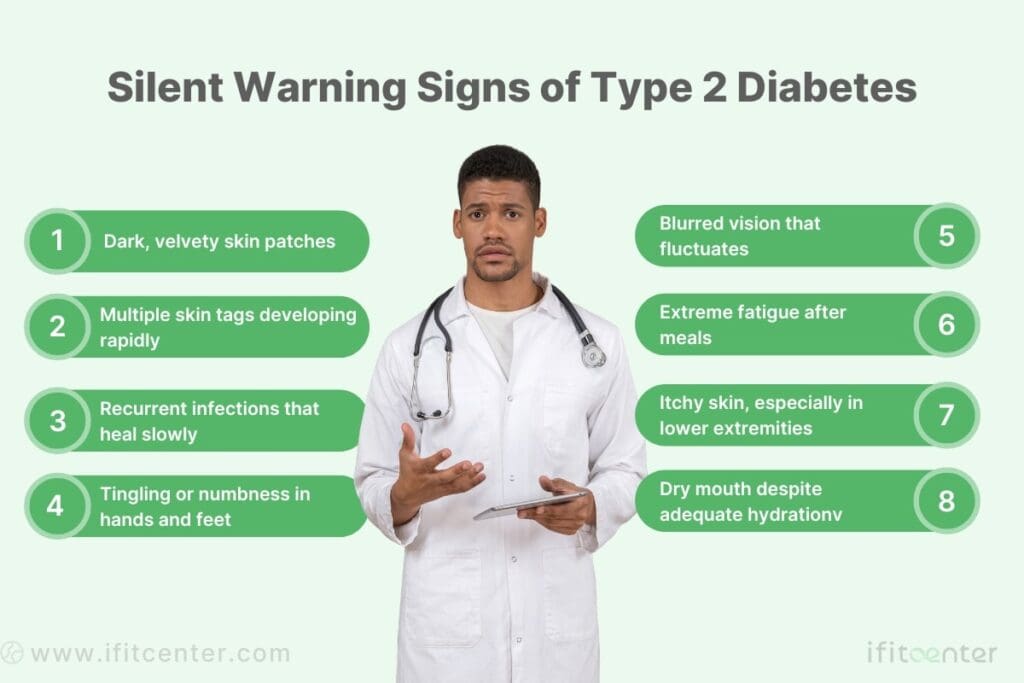
Skin Changes as Warning Signals
The skin often shows some of the earliest and most visible signs of Type 2 diabetes:
- Acanthosis nigricans: Dark, velvety patches in body folds, particularly the neck, armpits, or groin. This skin condition strongly signals insulin resistance, often appearing before diabetes is diagnosed.
- Skin tags: Small, soft skin growths that hang from the skin surface, particularly in areas where skin rubs against skin. Multiple skin tags can be an early indicator of insulin resistance.
- Diabetic dermopathy: Small, round, light brown scaly patches, often on the shins. Sometimes called “shin spots,” these lesions result from changes in the small blood vessels.
- Dry, itchy skin: General skin dryness, particularly in the lower extremities, can occur as elevated blood sugar affects circulation and sweat gland function.
Frequent Infections
People with developing Type 2 diabetes often experience recurring infections as elevated blood sugar creates favorable conditions for bacterial and fungal growth:
- Yeast infections: Both women and men may experience frequent yeast infections. For women, this manifests as vaginal yeast infections; for men, as jock itch or fungal infections under the foreskin.
- Urinary tract infections: The sugar-rich urine provides an ideal environment for bacterial growth.
- Gum disease and oral infections: Diabetes reduces the body’s ability to fight bacteria in the mouth.
- Skin infections: Minor cuts or scrapes may become infected more easily and heal more slowly.
Nerve-Related Symptoms
Nerve damage (neuropathy) can begin before Type 2 diabetes is diagnosed, as insulin resistance and mildly elevated blood sugar levels can damage nerves over time:
- Numbness or tingling: Often beginning in the toes and fingers, this “pins and needles” sensation can be intermittent initially
- Burning pain: Particularly in the feet, often worse at night
- Loss of sensation: Decreased ability to feel pain, temperature, or pressure, especially in the feet
- Muscle weakness: May begin subtly in the feet and legs
These nerve-related symptoms are particularly important to recognize early, as they can progress and lead to serious complications if blood sugar remains uncontrolled.
“Many patients come to me describing vague symptoms like persistent fatigue, frequent infections, or skin changes they’ve had for months or even years before diagnosis. What’s crucial to understand is that Type 2 diabetes often develops silently, with blood glucose levels rising gradually enough that the body partially adapts. This adaptation masks the warning signals, allowing damage to blood vessels and nerves to occur long before obvious symptoms emerge. This is why I advise patients with risk factors like family history or excess weight not to wait for classic symptoms to appear before screening.”
Dr. Babak Jamalian, Family Physician.
Specific Symptoms of Diabetes by Gender
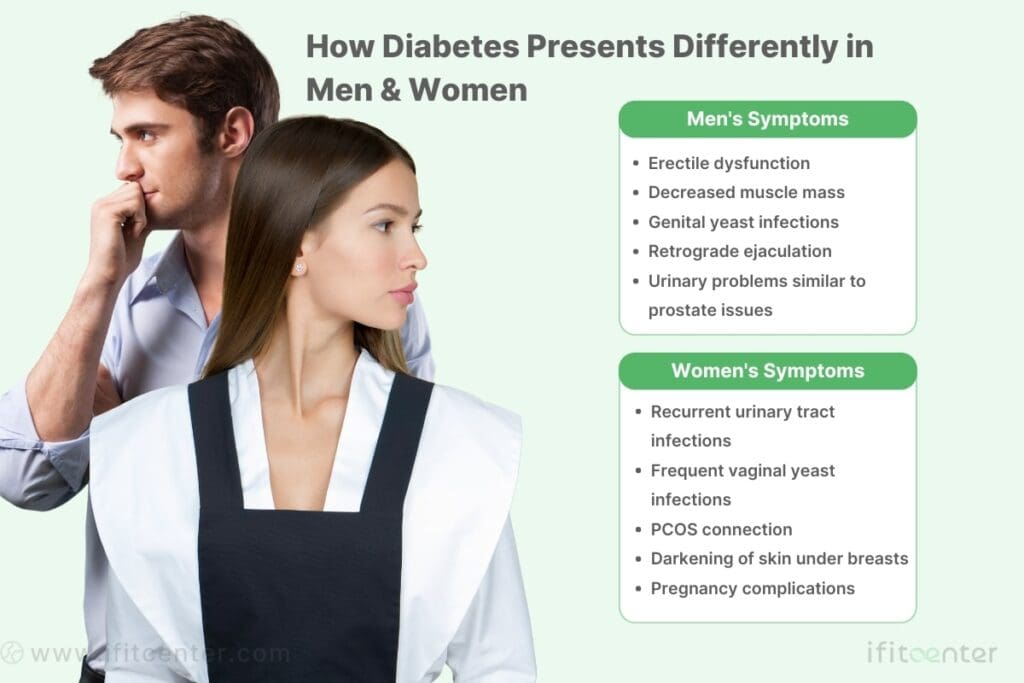
While many diabetes symptoms are common across genders, women and men may experience distinct warning signs that can help with earlier detection.
Diabetes Symptoms in Women
Women with diabetes often experience specific symptoms that can sometimes be misattributed to other conditions:
- Recurrent urinary tract infections: Elevated sugar in urine creates an ideal environment for bacteria. Multiple UTIs within a short period, despite antibiotic treatment, may signal blood sugar issues.
- Vaginal yeast infections: Excess sugar in the body promotes yeast growth. Recurring infections characterized by itching, burning, and unusual discharge can indicate diabetes.
- PCOS connection: Women with Polycystic Ovary Syndrome have higher insulin resistance. Symptoms like irregular periods, unexplained abdominal weight gain, and unusual hair growth may signal both PCOS and developing diabetes.
- Female-specific skin changes: Women may notice darkening of skin under the breasts, skin tags along the bra line, or unusual rashes in genital areas.
- Pregnancy complications: Unexplained miscarriages or delivering unusually large babies may warrant diabetes screening, especially when other risk factors are present.
Diabetes Symptoms in Men
Men may experience several distinct diabetes symptoms that are often overlooked:
- Erectile dysfunction: High blood sugar damages blood vessels and nerves essential for normal erectile function. ED can appear years before other diabetes symptoms, especially in younger men or when it develops suddenly.
- Decreased muscle mass: Unusual muscle wasting, particularly in the upper arms and thighs, may occur as the body breaks down muscle protein for energy when it cannot properly use glucose.
- Male-pattern baldness connection: Early-onset baldness (before age 35) combined with other risk factors like increased thirst or fatigue may signal insulin resistance.
- Genital issues: Men may experience balanitis (inflammation of the penis head), retrograde ejaculation (semen entering the bladder during orgasm), or genital thrush (yeast infections causing redness and itching).
- Urological problems: Diabetes can affect bladder function, causing difficulty starting urination, weak stream, or incomplete emptying—symptoms often mistaken for prostate issues.
Understanding these gender-specific warning signs can lead to earlier diagnosis and treatment. If you’re experiencing any of these symptoms, especially alongside classic diabetes signs, consider speaking with a healthcare provider about appropriate screening.
Symptoms of Diabetes in Children and Adolescents
Diabetes symptoms in children can be easily overlooked or confused with normal childhood behavior. Parents should be alert to these warning signs:
For Type 1 diabetes, which often develops rapidly in children:
- Excessive thirst and urination: Suddenly drinking unusual amounts and frequent bathroom trips, including bedwetting in previously toilet-trained children
- Unexplained weight loss: Losing weight despite normal or increased appetite
- Constant hunger: Eating more but still losing weight
- Unusual fatigue: Lacking energy for normal activities
- Sweet-smelling breath: A fruity odor that signals ketone production
“The presentation of diabetes in children can be dramatically different from adults, something many parents don’t realize. While adults might experience gradual symptom onset over months or years, children—especially with Type 1 diabetes—can go from seemingly healthy to seriously ill within weeks. What makes early recognition particularly challenging is that initial symptoms like increased thirst, frequent urination, and mood changes can easily be attributed to normal childhood behaviors. I always tell parents to pay attention when multiple small changes appear together, as this pattern often signals something more significant than typical childhood development.”
Dr. Babak Jamalian, Family Physician.
For Type 2 diabetes, which develops more gradually in youth:
- Dark skin patches: Velvety areas on the neck or in skin folds (acanthosis nigricans)
- Slow-healing wounds: Cuts or scrapes taking longer to heal
- Tiredness after eating: Especially after high-carbohydrate meals
- Frequent infections: Recurring skin or urinary tract infections
Watch for changes in behavior and development:
- School problems: Declining grades or difficulty concentrating
- Vision changes: Squinting or complaints about blurry vision
- Mood swings: Unusual irritability or behavior changes
- Growth issues: Slowed height growth or unexpected weight patterns
- Sleep disruptions: Waking frequently to use the bathroom
Seek immediate medical attention if you notice:
- Rapid, deep breathing
- Extreme drowsiness or confusion
- Severe abdominal pain with nausea
- Fruity breath odor
Early diagnosis is crucial for children with diabetes. If you notice any combination of these symptoms, consult a healthcare provider promptly.
Conclusion
Recognizing the signs and symptoms of diabetes is crucial for early detection and treatment. Whether it’s the classic symptoms like excessive thirst, frequent urination, and unexplained weight loss, or more subtle indicators that vary by diabetes type, age, or gender, being aware of these warning signals can make a significant difference in health outcomes.
Early intervention is key to preventing serious complications. When diabetes is detected and treated promptly, many of the long-term effects on the eyes, kidneys, nerves, and cardiovascular system can be minimized or avoided altogether. This is particularly important for children, whose growing bodies are especially vulnerable to the effects of uncontrolled blood sugar.
If you recognize any combination of diabetes symptoms in yourself or a loved one, don’t hesitate to seek medical evaluation. A simple blood test can confirm or rule out diabetes, providing peace of mind or the opportunity to begin appropriate treatment quickly.
Modern diabetes management has evolved significantly, offering more options than ever before. Today’s approaches focus not just on controlling blood sugar but on comprehensive health, combining medication when needed with lifestyle modifications, technology-assisted monitoring, and personalized care plans.
To access other content on the IFitCenter’s blog, you can use the following links:
References for Classic Signs and Symptoms of Diabetes Mellitus
- American Diabetes Association. (2023). Standards of Medical Care in Diabetes—2023. Diabetes Care, 46(Supplement_1). https://diabetesjournals.org/care/issue/46/Supplement_1
- International Diabetes Federation. (2021). IDF Diabetes Atlas, 10th edition. https://diabetesatlas.org/
- Jones, A. G., & Hattersley, A. T. (2013). The clinical utility of C-peptide measurement in the care of patients with diabetes. Diabetic Medicine, 30(7), 803-817. DOI: 10.1111/dme.12159
- Ahlqvist, E., Storm, P., Käräjämäki, A., Martinell, M., Dorkhan, M., Carlsson, A., … & Groop, L. (2018). Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. The Lancet Diabetes & Endocrinology, 6(5), 361-369. DOI: 10.1016/S2213-8587(18)30051-2
- Chandrasekaran, S., & Weiskirchen, R. (2024). The Role of Obesity in Type 2 Diabetes Mellitus—An Overview. International Journal of Molecular Sciences, 25(3). DOI: 10.3390/ijms25031615
- Glovaci, D., Fan, W., & Wong, N. D. (2019). Epidemiology of Diabetes Mellitus and Cardiovascular Disease. Current Cardiology Reports, 21(4), 21. DOI: 10.1007/s11886-019-1107-y
- Ziegler, R., Neu, A. (2018). Diabetes in Childhood and Adolescence. Deutsches Ärzteblatt International, 115(9), 146-156. DOI: 10.3238/arztebl.2018.0146
- Fazeli Farsani, S., van der Aa, M. P., van der Vorst, M. M., Knibbe, C. A., & de Boer, A. (2013). Global trends in the incidence and prevalence of type 2 diabetes in children and adolescents: a systematic review and evaluation of methodological approaches. Diabetologia, 56(7), 1471-1488. DOI: 10.1007/s00125-013-2915-z
- Matti Uusitupa, Tauseef A Khan, Effie Viguiliouk, Hana Kahleova, Angela A Rivellese, Kjeld Hermansen, Andreas Pfeiffer, Anastasia Thanopoulou, Jordi Salas-Salvadó, Ursula Schwab, John L Sievenpiper. Prevention of Type 2 Diabetes by Lifestyle Changes: A Systematic Review and Meta-Analysis. Nutrients. 2019;11(11):2611. DOI: 10.3390/nu11112611
- Karla Ivette Galaviz, Mary Beth Weber, Audrey Straus, Jeehea Sonya Haw, KM Venkat Narayan, Mohammed Kumail Ali. Global Diabetes Prevention Interventions: A Systematic Review and Network Meta-analysis of the Real-World Impact on Incidence, Weight, and Glucose. Diabetes Care. 2018;41(7):1526–1534. DOI: 10.2337/dc17-2222
- Lu, X., Xie, Q., Pan, X. et al. Type 2 diabetes mellitus in adults: pathogenesis, prevention and therapy. Sig Transduct Target Ther 9, 262 (2024).
DOI: 10.1038/s41392-024-01951-9 - Zabetian, A., Keli, H. M., Echouffo-Tcheugui, J. B., Narayan, K. M., & Ali, M. K. (2013). Diabetes in the Middle East and North Africa. Diabetes Research and Clinical Practice, 101(2), 106-122. DOI: 10.1016/j.diabres.2013.03.010
- Bommer, C., Sagalova, V., Heesemann, E., Manne-Goehler, J., Atun, R., Bärnighausen, T., & Vollmer, S. (2018). Global Economic Burden of Diabetes in Adults: Projections From 2015 to 2030. Diabetes Care, 41(5), 963-970. DOI: 10.2337/dc17-1962



