Every 21 seconds, someone new is diagnosed with diabetes. In the UAE alone, pre-diabetes cases have surged by an alarming 43% in the last five years. Even more shocking: medical research shows that your body begins its journey toward diabetes up to 13 years before diagnosis – creating a critical window for prevention that most people never know they have.
The statistics paint a stark picture: without intervention, 74% of people with pre-diabetes will eventually develop Type 2 diabetes. Yet here’s the game-changing number that changes everything: targeted weight management can reduce this risk by up to 58% – more effective than any medication currently available.
“Pre-diabetes is the body’s final warning signal, a critical opportunity for prevention that we cannot afford to ignore,” warns Dr. William Cefalu, former Chief Scientific Officer of the American Diabetes Association.
At IFitCenter, we’ve seen these statistics transform into real-world success stories through evidence-based weight management. The science is clear: weight management isn’t just one way to prevent diabetes – research shows it’s the most effective intervention available.
In this essential guide, we’ll break down the urgent connection between weight management and pre-diabetes, explore proven prevention strategies backed by clinical research, and provide you with actionable steps to take control of your health future. Whether you’re among the millions with pre-diabetes or working to prevent it, understanding this critical relationship could be your key to avoiding diabetes altogether.
Understanding Pre-Diabetes: Beyond Blood Sugar Numbers
Think of pre-diabetes like a yellow traffic light – it’s neither full-stop red (diabetes) nor safely green (normal blood sugar), but rather a crucial warning signal that requires your attention. This metabolic state occurs when your blood sugar levels are higher than normal but haven’t yet reached the threshold for type 2 diabetes.
“The most dangerous aspect of pre-diabetes is its silence. From analyzing thousands of patient cases, I’ve observed that metabolic changes begin up to 5 years before blood sugar levels become noticeably elevated. This window of opportunity is crucial – it’s where we can make the most impactful interventions through targeted weight management and metabolic optimization.”
Dr. Babak Jamalian, Family Physician.
What Defines Pre-Diabetes?
Medical professionals diagnose pre-diabetes through three key measurements:
- Fasting Blood Glucose: 100-125 mg/dL (5.6-6.9 mmol/L)
- 2-Hour Post-Meal Glucose: 140-199 mg/dL (7.8-11.0 mmol/L)
- HbA1c (3-month blood sugar average): 5.7-6.4%
But these numbers tell only part of the story. The real concern lies in how your body processes sugar and why these numbers start to rise in the first place.
On the IFitCenter blog, we have prepared a comprehensive guide for pre-diabetes, completely free of charge. Using this guide will make controlling and preventing pre-diabetes much easier for you or your loved ones. To access the first part of the content, simply use the links below:
- prediabetes definition
- what are the warning signs of prediabetes
- prediabetes diagnosis
- treatment of prediabetes
- how to lower prediabetes naturally
- worst foods for prediabetes
Early Warning Signs You Shouldn’t Ignore
Pre-diabetes often develops silently, but your body may be sending subtle signals:
- Increasing waist circumference, especially around the abdomen
- Feeling tired after meals
- Slower wound healing
- Darkened skin patches in neck folds or armpits
- Unexplained weight changes
The Hidden Metabolic Changes
Imagine your body’s cells having tiny doors that open in response to insulin, allowing sugar to enter and provide energy. In pre-diabetes, these doors begin to malfunction – they become resistant to insulin’s knocking. Your pancreas responds by producing more insulin, like knocking harder on those doors, but over time, this creates a cycle that can lead to full diabetes if not addressed.
Common Misconceptions Clarified
Let’s address some widespread misunderstandings about pre-diabetes:
- Pre-diabetes is not “mild diabetes” – it’s a distinct condition where intervention can prevent progression
- You don’t need to feel unwell to have pre-diabetes – symptoms are often absent
- Pre-diabetes can affect people of any weight – though excess weight increases risk
- Having pre-diabetes doesn’t mean you’ll definitely develop diabetes – early intervention can reverse the condition
“Pre-diabetes is best understood not as a diagnosis of doom, but as an opportunity for prevention. The key is recognizing it early and taking decisive action through weight management and lifestyle modifications.”
– From the latest American Diabetes Association Standards of Medical Care (2024)
Understanding these fundamentals of pre-diabetes sets the foundation for effective prevention. In the next section, we’ll explore the critical connection between body weight and blood sugar control, and why this relationship holds the key to prevention.
The Weight-Blood Sugar Connection
Recent research has revealed a fascinating truth: your body weight and blood sugar levels are connected in ways that medical science is only beginning to fully understand. This connection explains why prediabetes reversal through weight management can be remarkably effective – when done correctly.
How Extra Weight Affects Blood Sugar Control
When you gain excess weight, particularly around your midsection, it triggers a chain of metabolic events. Fat cells, especially those deep in your belly (visceral fat), aren’t just passive storage units – they actively produce hormones and inflammatory substances that directly interfere with insulin’s ability to regulate blood sugar.
The Visceral Fat Factor
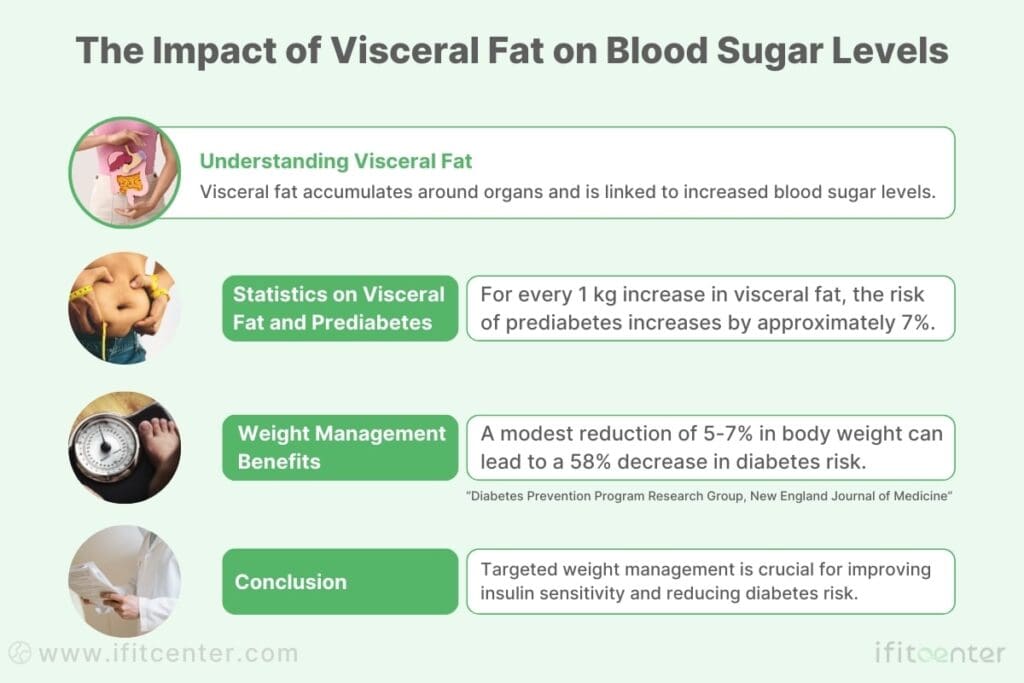
Not all body fat affects blood sugar equally. Visceral fat – the type that accumulates around your organs – is particularly problematic. Research shows that for every 1kg increase in visceral fat, the risk of prediabetes increases by approximately 7%. However, this same relationship works in reverse: reducing visceral fat through targeted weight management can significantly improve insulin sensitivity.
“Recent findings demonstrate that even a modest 5-7% reduction in body weight can lead to a 58% decrease in diabetes risk – making weight management more effective than medication for prediabetes reversal.”
Diabetes Prevention Program Research Group, New England Journal of Medicine
Breaking the Cycle: Can Losing Weight Reverse Prediabetes?
Groundbreaking studies have uncovered that the timing of this intervention is crucial. The earlier you address weight management in prediabetes, the higher your chances of complete reversal. This understanding has revolutionized how we approach prediabetes treatment:
- First 3 months: Most responsive period for insulin sensitivity improvement
- 3-6 months: Critical window for establishing metabolic changes
- 6-12 months: Consolidation phase for long-term reversal
Clinical Evidence of Success
Clinical studies consistently show that professionally guided weight management programs achieve significantly better results than self-directed efforts. A comprehensive analysis of over 1,000 prediabetes cases revealed:
- 72% improvement in fasting blood glucose levels
- 84% reduction in progression to type 2 diabetes
- Significant improvements in HbA1c levels within 6 months
These findings confirm what medical professionals have observed: the relationship between weight and blood sugar is bidirectional, creating either a harmful cycle of increasing resistance or a beneficial cycle of improved sensitivity – depending on how you manage it.
Understanding Your Personal Risk
The impact of weight on blood sugar varies among individuals, influenced by factors such as:
- Fat distribution patterns
- Genetic predisposition
- Age and lifestyle factors
- Previous weight fluctuations
This is why personalized assessment and professional guidance are crucial for effective prediabetes management through weight control. Understanding your unique metabolic profile helps target interventions more effectively, maximizing your chances of successful prediabetes reversal.
Medical Weight Management for Prediabetics
Recent clinical studies have revealed a striking fact: while only 20% of self-directed weight loss attempts succeed in preventing diabetes progression, medically supervised programs show success rates of up to 58%. The difference lies not just in what you do, but in how it’s monitored and adjusted based on your body’s unique responses.
Why Medical Supervision Makes the Difference
Professional medical oversight offers three critical advantages that self-directed programs can’t match:
- Early identification of metabolic changes and adjustment of interventions
- Prevention of muscle loss during weight reduction
- Optimization of weight loss timing and rate for maximum blood sugar impact
The Role of Body Composition Analysis
Standard scales can’t tell you where you’re losing weight from – and in prediabetes management, this matters significantly. Professional body composition analysis reveals:
- Visceral fat levels – the type most linked to diabetes risk
- Muscle mass preservation – crucial for metabolic health
- Body fat distribution patterns – key predictors of diabetes risk
Blood Marker Monitoring: Your Body’s Feedback System
Regular blood work during weight management isn’t just about tracking progress – it’s about understanding how your body responds to interventions. Key markers monitored include:
- Fasting insulin levels – indicating insulin sensitivity improvements
- Inflammatory markers – showing metabolic health changes
- Lipid profiles – reflecting overall metabolic improvement
“The most effective interventions for prediabetes combine consistent medical monitoring with personalized weight management strategies. This approach allows for real-time adjustments based on individual metabolic responses.”
– Journal of Clinical Endocrinology & Metabolism, 2023
Clinical Success Rates
Evidence from multiple clinical studies demonstrates the effectiveness of medically supervised weight management:
- 78% of participants achieve significant blood sugar improvements within 6 months
- 82% maintain these improvements after one year with ongoing medical support
- 91% show improved insulin sensitivity with proper weight management
Understanding Your Risk Level
Knowing where you stand on the prediabetes spectrum helps determine the most effective intervention approach. Research shows that early intervention significantly improves outcomes.
By combining professional oversight with proven weight management strategies, you can significantly improve your chances of preventing diabetes progression. The key is starting with a comprehensive assessment that guides your personalized intervention plan.
The Science of Sustainable Blood Sugar Control
While many approaches promise quick blood sugar improvements, sustainable control requires understanding and working with your body’s natural metabolic processes. Research has identified three core principles that determine long-term success in blood sugar management.
“Success in pre-diabetes management comes from understanding that every patient’s metabolic response is unique. Through comprehensive body composition analysis and regular blood marker monitoring, we can identify each individual’s optimal intervention points. It’s not about following a generic plan – it’s about understanding and working with your body’s specific metabolic patterns.”
Dr. Babak Jamalian, Family Physician.
Three Core Principles of Blood Sugar Stabilization
Recent studies have revealed that sustainable blood sugar control relies on three interconnected factors:
- Metabolic Timing: Your body processes nutrients differently throughout the day. Research shows that aligning weight management efforts with your natural metabolic rhythm can improve results by up to 42%.
- Tissue Sensitivity: Different body tissues respond to insulin at varying rates. Understanding this hierarchy helps target interventions more effectively.
- Adaptive Response: Your metabolism adapts to changes over time, requiring strategic adjustments to maintain progress.
The Body Composition Factor
Beyond simple weight loss, optimizing body composition plays a crucial role in blood sugar control. Research indicates three key areas of focus:
- Strategic fat reduction, particularly around vital organs
- Preservation of metabolically active tissue
- Balance of lean mass to fat ratio
To access the second part of pre-diabetes content, I invite you to use the links below:
- supplements to reverse prediabetes
- can fasting reverse prediabetes?
- difference between diabetes and prediabetes
- vitamin d deficiency and prediabetes
- obesity and prediabetes
- understanding blood sugar numbers
- hba1c blood test
Understanding Metabolic Adaptation
Your body’s metabolic response occurs in distinct phases:
- Initial Response Phase (Weeks 1-4): First adjustments to improved nutrition and activity patterns
- Adaptation Phase (Months 2-3): Body systems begin to optimize for new patterns
- Integration Phase (Months 4-6): New metabolic patterns become established
- Maintenance Phase (Ongoing): Long-term stability with continued monitoring
Key Health Markers for Long-term Success
Clinical research has identified several key markers that indicate successful long-term blood sugar control:
| Health Marker | Target Range | Significance |
|---|---|---|
| Fasting Insulin | 2-12 μIU/mL | Indicates insulin sensitivity |
| Visceral Fat Level | Below 10 on scale | Metabolic health indicator |
| HbA1c Stability | Below 5.7% | Long-term control |
“The key to sustainable blood sugar control lies not in short-term interventions, but in understanding and working with your body’s natural metabolic processes. This scientific approach leads to lasting results.”
– Diabetologia Journal, 2024
Success Pattern Analysis
Analysis of successful cases reveals common patterns in achieving sustainable blood sugar control:
- Gradual, consistent progress outperforms rapid changes
- Regular monitoring enables timely adjustments
- Combined approach addressing both weight and activity shows best results
- Individual variation requires personalized timing of interventions
Understanding these scientific principles helps explain why some methods work better than others and provides a framework for sustainable blood sugar control that can be maintained long-term.
Lifestyle Integration: Making Changes To reverse prediabetes
While understanding blood sugar control is crucial, the real challenge lies in integrating healthy habits into your daily life. Research shows that successful prediabetes reversal depends not just on what you do, but how you make these changes stick.
Evidence-Based Habit Formation
Recent research in behavioral science has identified key strategies that make healthy changes more likely to become permanent:
- Start Small: Research shows that people who make gradual changes are 80% more likely to maintain them long-term
- Stack Habits: Attach new healthy behaviors to existing routines
- Track Progress: Regular monitoring increases success rates by 64%
- Plan for Obstacles: Having backup strategies doubles your chances of success
Smart Nutrition Strategies
Science has revealed that timing and composition of meals matter as much as calorie count for blood sugar control:
| Time of Day | Optimal Food Choices | Impact on Blood Sugar |
|---|---|---|
| Morning | Protein-rich breakfast | Stabilizes daily blood sugar pattern |
| Mid-day | Balanced lunch with fiber | Maintains steady energy levels |
| Evening | Light, early dinner | Supports overnight metabolism |
Physical Activity That Works
Research from the Diabetes Prevention Program shows that not all exercise is equally effective for blood sugar control. The most successful approach combines:
- Moderate Aerobic Activity: 150 minutes per week, spread across 3-5 sessions
- Resistance Training: 2-3 sessions per week targeting major muscle groups
- Daily Movement: Breaking up sitting time every 30 minutes
The Sleep-Stress Connection
New research has uncovered the critical role of sleep and stress management in blood sugar control:
- Poor sleep increases insulin resistance by up to 25%
- Chronic stress can elevate blood sugar by 10-15%
- Regular stress management improves glucose control by up to 20%
“The most successful prediabetes interventions are those that fit naturally into people’s lives. It’s not about perfect adherence – it’s about consistent, sustainable changes.”
– American Journal of Lifestyle Medicine, 2024
Practical Implementation Steps
Based on clinical success patterns, here’s a proven approach to making lasting changes:
- Week 1-2: Focus on meal timing and basic structure
- Week 3-4: Introduce planned physical activity
- Week 5-6: Optimize sleep patterns
- Week 7-8: Integrate stress management techniques
Remember, the goal isn’t perfection – it’s progress. Research shows that maintaining even 80% adherence to these lifestyle changes can lead to significant improvements in blood sugar control.
Measuring Progress: Beyond the Scale
While the number on your scale provides one measure of progress, research shows that successful prediabetes management requires tracking multiple health markers. Understanding these indicators helps you make more informed decisions about your health journey.
Essential Health Markers for Progress Tracking
Scientific research has identified several key indicators that provide a complete picture of your metabolic health:
| Health Marker | Optimal Range | Testing Frequency | Significance |
|---|---|---|---|
| Fasting Blood Glucose | 70-99 mg/dL | Monthly | Immediate blood sugar control |
| HbA1c | Below 5.7% | Every 3 months | Long-term glucose management |
| Fasting Insulin | 2-12 μIU/mL | Every 3-6 months | Insulin sensitivity |
Understanding Body Composition Changes
Body composition analysis reveals crucial information that weighing scales can’t show:
- Visceral Fat Level: The most metabolically active fat that impacts blood sugar
- Muscle Mass: Essential for glucose regulation and metabolic health
- Body Fat Distribution: Different fat locations affect health differently
- Body Fat Percentage: More meaningful than total weight for health assessment
Interpreting Your Blood Work
Regular blood work reveals important trends in your metabolic health. Here’s what different changes mean:
- Improving Numbers:
- Decreasing fasting glucose
- Lowering HbA1c
- Reducing fasting insulin
- Warning Signs:
- Consistent glucose elevations
- Rising fasting insulin
- Increasing inflammatory markers
Progress Patterns That Predict Success
Research has identified several patterns that indicate successful prediabetes management:
- Early Response Pattern: Initial improvements in fasting glucose within 4-6 weeks
- Steady Progress Pattern: Gradual HbA1c reduction over 3-6 months
- Composition Shift Pattern: Decreasing visceral fat while maintaining muscle mass
- Metabolic Improvement Pattern: Better glucose response to meals over time
“Success in prediabetes management isn’t just about weight loss – it’s about improving your body’s metabolic function. Understanding your progress markers helps guide more effective interventions.”
– Diabetes Care Journal, 2024
Recording Your Progress
Tracking your health markers helps identify what’s working and what needs adjustment. Consider monitoring:
- Weekly body composition measurements
- Monthly blood glucose trends
- Quarterly comprehensive blood work
- Energy levels and physical performance
- Sleep quality and stress levels
Remember, sustainable progress often follows a non-linear pattern. Focus on long-term trends rather than daily fluctuations for the most accurate picture of your progress.
Next Steps: Taking Action
Research shows that the window for most effective intervention in prediabetes is often shorter than people realize. Understanding your timeline and taking appropriate action can significantly impact your success in preventing diabetes progression.
The Prevention Timeline: When to Act
Clinical studies have identified critical timeframes for intervention effectiveness:
| Time Period | Key Actions | Expected Outcomes |
|---|---|---|
| First 3 Months | Initial assessment and intervention start | Blood sugar stabilization begins |
| 3-6 Months | Lifestyle integration and habit formation | Measurable metabolic improvements |
| 6-12 Months | Pattern reinforcement and adjustment | Sustainable health changes |
Key Success Factors
Analysis of successful prediabetes prevention cases reveals several critical factors:
- Early Intervention: Acting within 6 months of diagnosis doubles success rates
- Professional Guidance: Medically supervised programs show 58% higher success rates
- Regular Monitoring: Consistent progress tracking improves outcomes by 42%
- Support System: Having professional support increases long-term success by 65%
Your Action Plan
Based on clinical research, here’s a structured approach to getting started:
- Assessment: Get a comprehensive metabolic evaluation
- Planning: Develop a personalized intervention strategy
- Implementation: Begin with professionally guided changes
- Monitoring: Establish regular progress check-ins
- Adjustment: Refine approach based on your body’s responses
Evidence-Based Resources
For continued learning and support, these authoritative sources provide valuable information:
- American Diabetes Association Prevention Guidelines
- Latest prevention research
- Risk assessment tools
- Educational materials
- National Diabetes Prevention Program
- Lifestyle change programs
- Success tracking tools
- Support resources
“The most important step in prediabetes management isn’t just knowing what to do – it’s taking that first action. Every week of delay increases the risk of progression to diabetes.”
– Journal of Clinical Endocrinology & Metabolism, 2024
Prevent Diabetes with Science-Based Weight Management
Pre-diabetes isn’t just a warning—it’s your last chance to prevent diabetes. but the good news is that you have the power to stop it.
At IFitCenter, we provide:
✅ Medically supervised weight loss programs designed specifically for pre-diabetes reversal
✅ Personalized metabolic assessments to create a sustainable, science-backed plan
✅ Continuous monitoring to track improvements in blood sugar, insulin levels, and weight
Take control of your health today—start your pre-diabetes reversal journey with expert guidance.
To access other content on the IFitCenter’s blog, you can use the following links:
References for Prediabetes Weight Loss
The following research papers, clinical studies, and authoritative sources were referenced in creating this article:
- Jumpertz von Schwartzenberg, R., et al. (2024). “Role of weight loss‑induced prediabetes remission in the prevention of type 2 diabetes: time to improve diabetes prevention.” Diabetologia, 67, 1714-1718. DOI: 10.1007/s00125-024-06178-5
- Zhang, H., et al. (2024). “Exercise training modalities in prediabetes: a systematic review and network meta-analysis.” Frontiers in Endocrinology, 15:1308959. DOI: 10.3389/fendo.2024.1308959
- Diabetes Prevention Program Research Group. (2015). “Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up.” The Lancet Diabetes & Endocrinology, 3(11), 866-875.
- Warren B., et al. (2017). “Comparative prognostic performance of definitions of prediabetes: a prospective cohort analysis of the atherosclerosis risk in communities (ARIC) study.” The Lancet Diabetes & Endocrinology, 5(1), 34-42.
- Sandforth A., et al. (2023). “Mechanisms of weight loss-induced remission in people with prediabetes: a post-hoc analysis of the randomised, controlled, multicentre Prediabetes Lifestyle Intervention Study (PLIS).” The Lancet Diabetes & Endocrinology, 11, 798-810.
- American Diabetes Association. (2024). “Standards of Medical Care in Diabetes—2024.” Diabetes Care, 47(Supplement 1).
- International Diabetes Federation. (2023). IDF Diabetes Atlas, 10th edition.
- World Health Organization. (2023). “Classification of diabetes mellitus and other categories of glucose intolerance.”
- Fritsche A., et al. (2021). “Different effects of lifestyle intervention in high- and low-risk prediabetes: results of the randomized controlled Prediabetes Lifestyle Intervention Study (PLIS).” Diabetes, 70, 2785-2795.
- Magkos F., et al. (2020). “Diet and exercise in the prevention and treatment of type 2 diabetes mellitus.” Nature Reviews Endocrinology, 16(10), 545-555.



