Have you ever followed all the “right” dietary advice yet still experienced mid-afternoon energy crashes? Or meticulously avoided sugar but found your glucose levels stubbornly high? If so, you’re not alone—and contrary to popular belief, blood sugar control isn’t simply about avoiding desserts or counting carbohydrates.
What if you could stabilize your blood sugar without extreme diets or medication? What if simple adjustments to how you sequence your meals could dramatically reduce glucose spikes? And what if common kitchen ingredients already in your pantry could help maintain steadier energy levels throughout your day?
At IFitCenter, we’re dedicated to bringing you evidence-based approaches to natural blood sugar control that go beyond conventional wisdom. In this comprehensive guide, we’ll explore five scientifically-validated techniques that can help you maintain balanced glucose levels throughout the day—techniques that are practical, sustainable, and don’t require radical lifestyle overhauls.
Meal Sequencing: The Order That Makes All the Difference
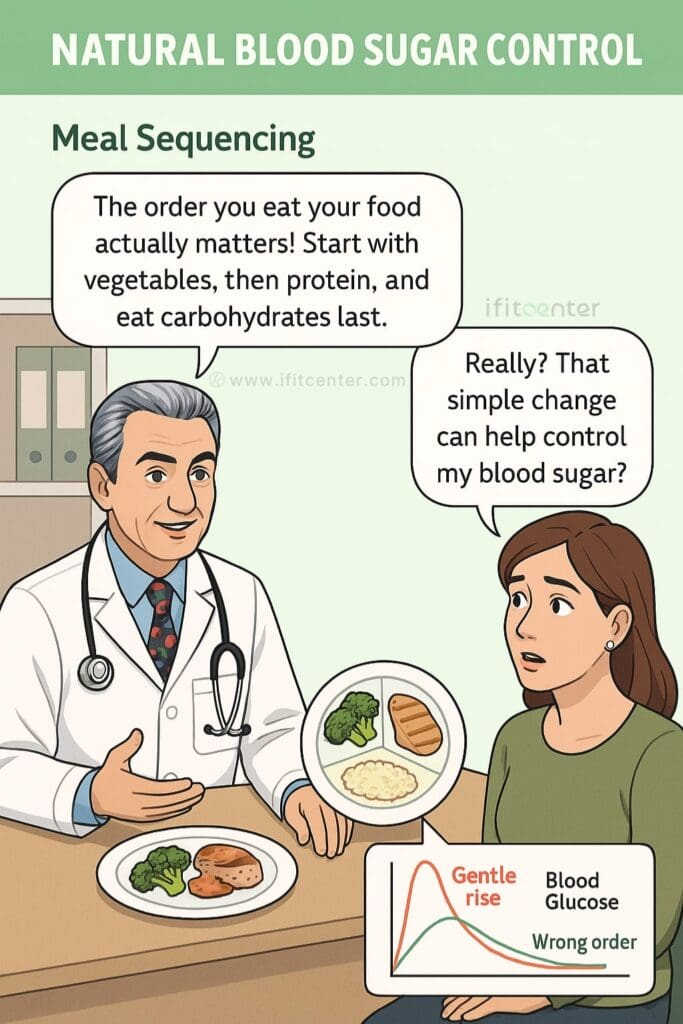
Did you know that simply changing the order in which you eat your food can dramatically improve your blood sugar control? This strategy doesn’t require special foods or restrictive diets—just a simple rearrangement of what’s already on your plate.
The Science Behind Food Order and Blood Sugar Control
Research published in Diabetes Care found that eating vegetables and protein before carbohydrates reduced post-meal glucose levels by up to 37% compared to eating the same foods in reverse order. This powerful technique for controlling blood sugar has since been confirmed in multiple studies, including a comprehensive review in the journal Nutrients.
When you eat carbohydrates first, they quickly break down into glucose, causing blood sugar levels to spike rapidly. However, consuming vegetables and protein first activates several mechanisms that help maintain stable glucose levels:
- Physical barrier effect: Fiber from vegetables slows carbohydrate absorption
- Hormonal response: Protein and fat trigger hormones that delay gastric emptying
- Enhanced insulin action: This sequence improves your body’s insulin response
Practical Meal Sequencing for Glycemic Control
Implementing this strategy for blood sugar management is straightforward:
- Start with non-starchy vegetables: Begin meals with salad, broccoli, or green beans
- Eat protein second: Consume your protein source (meat, fish, eggs, tofu) next
- Save carbohydrates for last: Finish with starches (bread, rice, pasta, potatoes)
“What many people don’t realize about blood sugar control is that it’s not just about what you eat, but how you eat it. patients who implement proper meal sequencing often see significant improvements in their glucose response even without reducing their overall carbohydrate intake. This approach is particularly valuable because it allows for greater dietary flexibility while still supporting metabolic health.”
Dr. Babak Jamalian, Family Physician.
| Meal | Optimal Sequence for Sugar Control |
|---|---|
| Breakfast | Eggs/protein → vegetables → toast/cereal |
| Lunch | Salad → protein portion → sandwich bread/wrap |
| Dinner | Vegetables → protein → rice/pasta/potatoes |
Continuous glucose monitoring has shown that this simple change can transform how your body processes a meal. The same foods eaten in the optimal sequence typically raise blood glucose by only 10-20 mg/dL, compared to spikes of 30-50 mg/dL when carbohydrates are consumed first.
For many people struggling with high blood sugar, this approach provides a practical way to maintain more stable glucose levels without giving up foods they enjoy—making it one of the best methods for controlling blood sugar naturally.
Note: If you’re taking medications to control high sugar levels, consult your healthcare provider before making changes, as this strategy may affect your medication requirements.
The Vinegar Strategy: A Powerful Tool in Your Kitchen
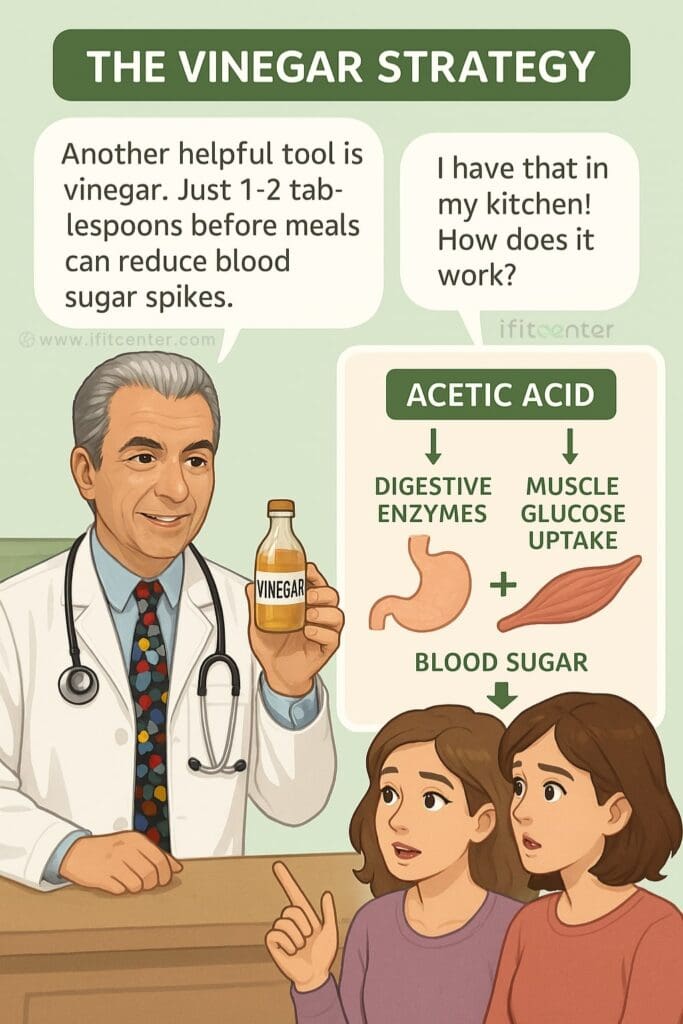
Looking for a simple, affordable way to control blood sugar that’s backed by science? The answer might already be in your kitchen. Research has consistently shown that vinegar—particularly its active component, acetic acid—can significantly reduce blood sugar spikes after meals.
In the IFitCenter blog, we have prepared a free information database about diseases, including diabetes, for our dear readers. By reviewing this information, you will gain valuable insights for controlling and preventing these conditions. To access the first part of this information, you can use the links below:
- what is diabetes?
- diabetes sign and symptoms
- how to test for diabetes
- Difference Between Type 1 and Type 2 Diabetes
How Vinegar Helps Control High Sugar Levels
Vinegar works through two primary mechanisms to help maintain stable blood glucose:
- Enzyme inhibition: Acetic acid temporarily inhibits alpha-amylase, an enzyme that breaks down carbohydrates into glucose. This slows the conversion of complex carbs into sugar, preventing rapid spikes in blood glucose levels.
- Enhanced muscle glucose uptake: Research published in the Journal of Diabetes Research found that vinegar consumption increases insulin-stimulated glucose uptake by muscle cells, helping remove sugar from the bloodstream more efficiently.
A systematic review and meta-analysis published in Diabetes Research and Clinical Practice confirmed that vinegar consumption reduces both post-meal glucose and insulin responses. The effect is particularly notable when vinegar is consumed before carbohydrate-rich meals.
Practical Ways to Use Vinegar for Blood Sugar Control
Incorporating vinegar into your daily routine doesn’t mean drinking it straight (which isn’t recommended). Here are practical, palatable methods:
- Timing: Consume 1-2 tablespoons of vinegar 10-20 minutes before carbohydrate-containing meals for optimal effect on blood sugar
- Salad dressing: Mix vinegar with olive oil for a pre-meal salad
- Diluted drink: Mix 1 tablespoon of vinegar in a large glass of water (add a small amount of honey if needed for palatability)
- Cooking ingredient: Use vinegar in marinades, sauces, and as a flavor enhancer
- Pickled vegetables: Enjoy vinegar-pickled vegetables as an appetizer before main meals
Most types of vinegar contain acetic acid and can provide benefits:
- Apple cider vinegar
- Red wine vinegar
- White vinegar
- Rice vinegar
Important Safety Considerations
While vinegar is generally safe for most people, certain groups should exercise caution:
- People with gastric issues, ulcers, or acid reflux may experience worsened symptoms
- Those taking diabetes medications should monitor blood sugar carefully, as vinegar may enhance the medication’s effects
- Individuals with kidney problems should consult a healthcare provider before regular use
- Undiluted vinegar can damage tooth enamel and irritate the throat and digestive tract
Progressive healthcare providers are increasingly recommending vinegar as a complementary approach to blood sugar management, particularly for those seeking natural remedies to control blood sugar. When used correctly, this simple kitchen ingredient can be a valuable addition to your glucose control toolkit.
Strategic Carbohydrate Management
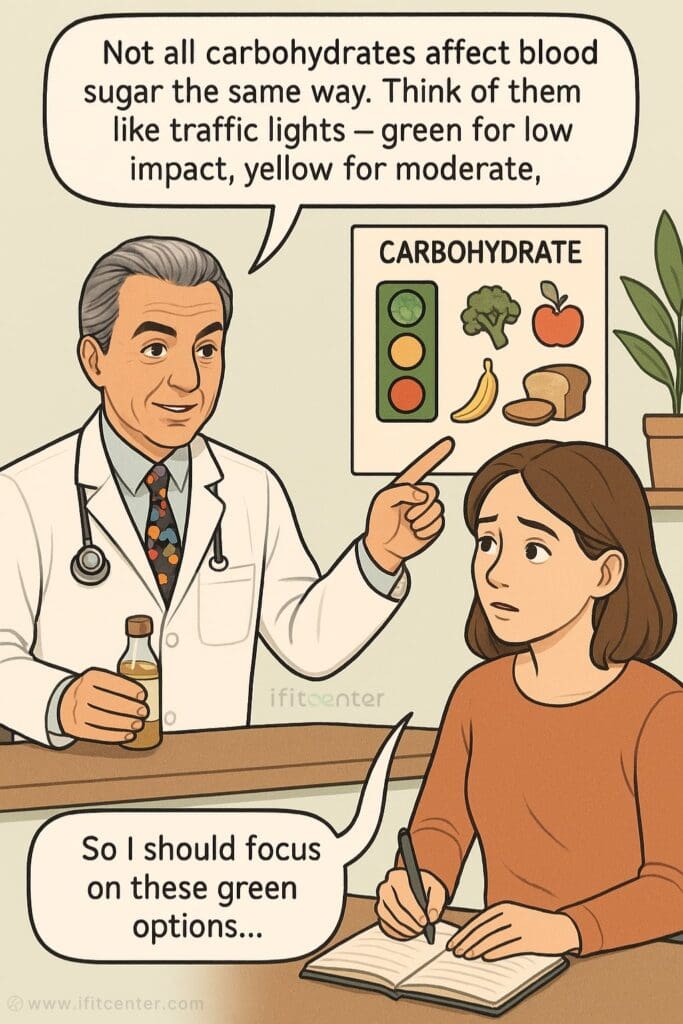
Not all carbohydrates affect your blood sugar the same way. Understanding which carbs cause rapid spikes and which have minimal impact is key to maintaining stable glucose levels without giving up foods you enjoy.
Understanding Glycemic Impact: The Traffic Light Approach
The glycemic index (GI) measures how quickly a food raises blood sugar compared to pure glucose. The glycemic load (GL) takes into account both the GI and the actual carbohydrate content in a typical serving—providing a more practical measure of a food’s real-world impact on blood glucose.
Think of carbohydrates like traffic signals for your blood sugar:
High GI Foods (Red Light)
- White bread (GI: 75)
- White rice (GI: 73)
- Instant oatmeal (GI: 79)
- Cornflakes (GI: 81)
- Potato chips (GI: 75)
- Soda/juice (GI: 68)
Medium GI Foods (Yellow Light)
- Basmati rice (GI: 58)
- Sweet potato (GI: 63)
- Whole wheat bread (GI: 69)
- Bananas (GI: 55)
- Pineapple (GI: 59)
- Steel-cut oats (GI: 55)
Low GI Foods (Green Light)
- Lentils (GI: 32)
- Chickpeas (GI: 28)
- Non-starchy vegetables (GI: <20)
- Greek yogurt (GI: 11-19)
- Apples (GI: 36)
- Popcorn (GI: 55)
The goal isn’t to eliminate carbohydrates completely but to choose wisely and manage their impact. Selecting more “green light” and fewer “red light” carbs can help maintain stable blood sugar levels without drastic dietary restrictions.
Practical Strategies for Carbohydrate Management
1. Portion Control
Even low-GI foods can raise blood sugar when consumed in large quantities. Some practical portion guidelines:
- Grains/starchy vegetables: ½ cup cooked (about the size of your fist)
- Bread: 1 slice or ½ a standard sandwich
- Fruit: 1 small piece or ½ cup berries
2. Strategic Timing
When you eat carbohydrates matters almost as much as what you eat:
- Consume higher-GI carbs around exercise when muscles can better utilize glucose
- Avoid eating high-carb foods right before bedtime
- Space carbohydrates throughout the day rather than consuming them all at once
3. The Resistant Starch Technique
When certain starchy foods are cooked and then cooled, some of the digestible starch transforms into resistant starch—a type of fiber that doesn’t raise blood sugar. This process is called retrogradation.
Try these examples:
- Cooled potatoes: Make potato salad with potatoes cooked and refrigerated overnight
- Chilled rice: Use leftover refrigerated rice for stir-fries
- Overnight oats: Prepare oats with yogurt and refrigerate overnight
This approach can lower the glucose impact of starchy foods by 20-40%.
Combining Strategies for Maximum Effect
For optimal blood sugar control, combine carbohydrate management with the previously discussed techniques:
- Choose lower-GI carbs when possible
- Practice correct meal sequencing (vegetables and protein first)
- Consider vinegar before higher-carb meals
- Take a brief walk after consuming carbohydrates
These evidence-based nutritional approaches offer practical ways to enjoy carbohydrates while maintaining stable blood glucose levels. The focus isn’t on restriction but on making informed choices that support metabolic health.
Post-Meal Movement: The 15-Minute Solution
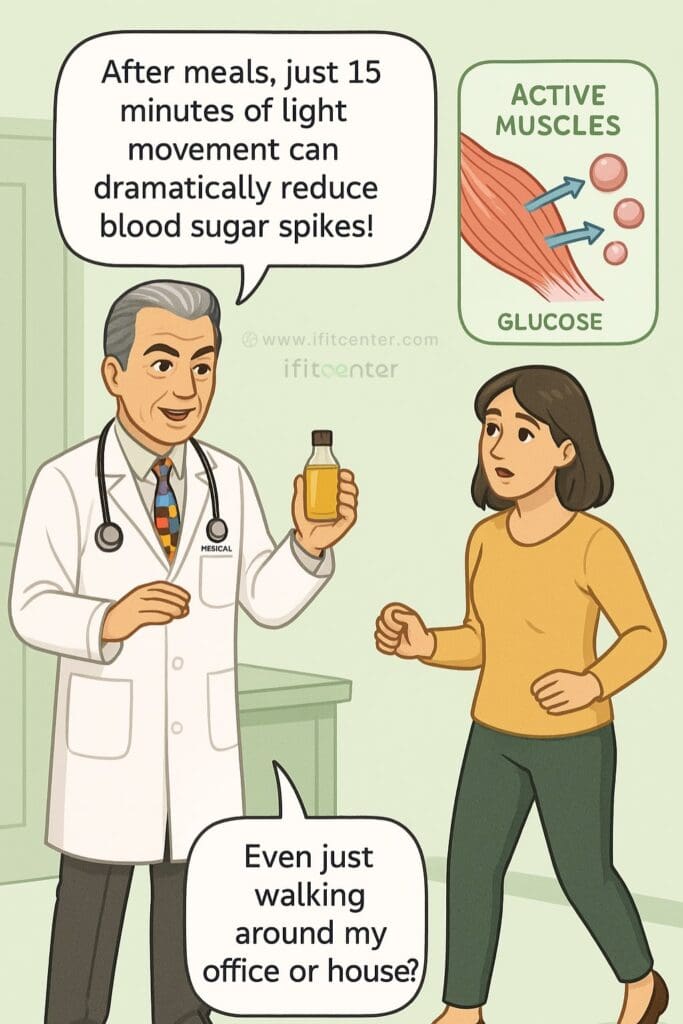
Looking for one of the simplest, most effective ways to control blood sugar? Move your body after eating. Just 15 minutes of light activity following meals can dramatically reduce blood glucose spikes—no gym membership or special equipment required.
Why Post-Meal Movement Works for Blood Sugar Control
Research published in Diabetes Therapy examined the timing of exercise for glucose management and found a clear winner: activity performed immediately after meals was significantly more effective at reducing blood sugar spikes than exercise before eating or no exercise at all.
The science is straightforward: When you exercise, your muscles become more efficient at absorbing glucose from your bloodstream, and they can do this independently of insulin. Think of active muscles as “glucose sponges” that help clear sugar from your blood without requiring additional insulin.
To access the second part of the information, you can use the links below:
- Fruits to Avoid with Diabetes
- Can You Drink Alcohol with Diabetes?
- Is Vinegar a Natural Solution for Managing Diabetes?
- How to Prevent Diabetes
Simple Post-Meal Activities for Blood Sugar Management
The key is light to moderate movement—nothing strenuous is needed. Here are practical options for different settings:
At Home:
- A casual 15-minute walk around your neighborhood
- Light housework (sweeping, vacuuming, tidying up)
- Simple standing exercises like marching in place or gentle stretching
- Dancing to a few favorite songs
At Work:
- Walking meeting with colleagues
- Taking the stairs instead of the elevator
- Standing at your desk while doing gentle movements
- Walking to a colleague’s desk instead of sending an email
Overcoming Common Barriers
| Common Barrier | Practical Solution |
|---|---|
| Time constraints | Even 5 minutes helps; split it into shorter sessions if needed |
| Physical limitations | Chair exercises, gentle arm movements, or ankle rotations still activate muscles |
| Weather issues | Indoor options: hallway walking, mall walking, home movement |
| Workplace restrictions | Bathroom breaks with extra walking, standing phone calls, desk stretches |
Clinical observations consistently confirm that post-meal movement is one of the most accessible and effective strategies for blood sugar control. Unlike many other approaches, this technique works regardless of fitness level and can be implemented immediately with virtually no cost or special preparation.
For optimal results, aim for movement within 30 minutes after finishing your meal—this timing aligns with when blood glucose typically begins to rise significantly. Remember that consistency matters more than intensity; gentle daily movement will provide better long-term benefits than occasional intense exercise.
Stabilize Blood Sugar with iFitCenter’s Weight Loss Solutions
Controlling your blood sugar effectively involves more than just dietary adjustments. At IFitCenter Clinic, Dr. Babak Jamalian offers personalized programs to support healthy weight management, enhancing your body’s natural glucose regulation through:
- Customized nutritional plans
- Lifestyle coaching
- Continuous professional oversight
Achieve lasting results by scheduling your consultation today.
Protein, Fat, and Fiber: The Blood Sugar Stabilizing Trio
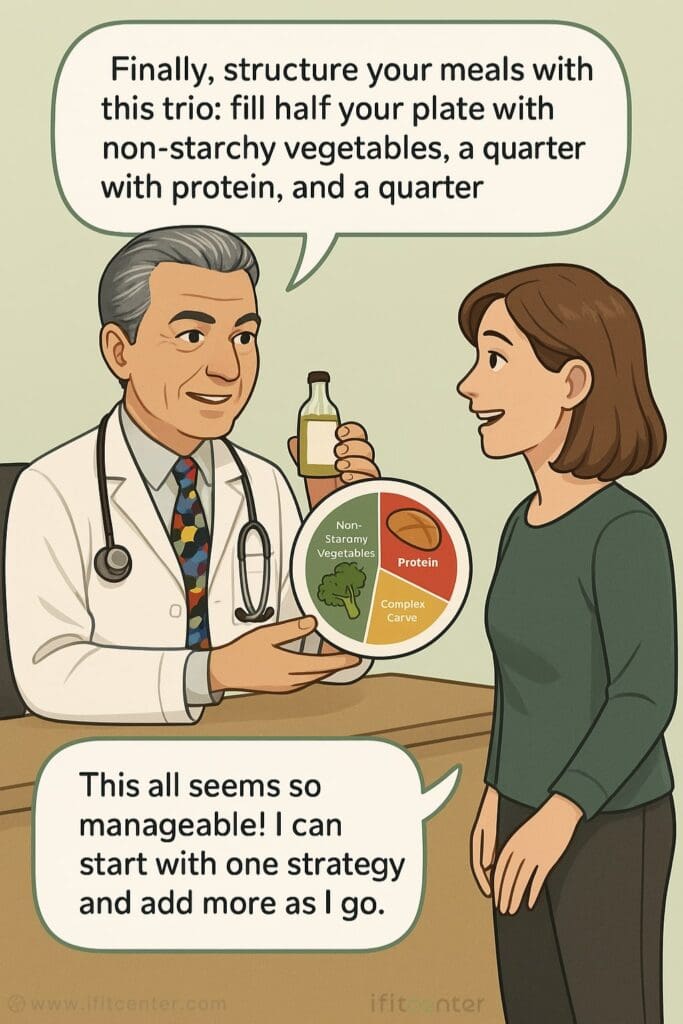
While carbohydrates raise blood glucose levels, protein, fat, and fiber can help keep them stable. Understanding how these three nutrients affect your blood sugar can transform your approach to meal planning without requiring strict dieting.
How Each Nutrient Affects Your Blood Sugar
Protein
- Minimal impact on blood glucose
- Triggers glucagon release that balances insulin
- Provides satiety to prevent overeating
- Creates steadier energy than carbohydrates
Fat
- Negligible effect on blood sugar
- Slows digestion and glucose absorption
- Helps maintain fullness between meals
- Provides sustained energy without spikes
Fiber
- Creates physical barrier to slow carb absorption
- Feeds beneficial gut bacteria that improve glucose metabolism
- Prevents rapid blood sugar spikes
- Improves insulin sensitivity over time
Blood Sugar-Friendly Food Combinations
| Meal | Blood Sugar Stabilizing Combination |
|---|---|
| Breakfast | Greek yogurt + berries + nuts (protein + fiber + fat) |
| Lunch | Large salad with chicken, avocado and olive oil dressing (fiber + protein + fat) |
| Dinner | Grilled salmon + roasted vegetables + small portion of quinoa (protein + fiber + fat + limited complex carbs) |
| Snack | Apple slices with almond butter (fiber + fat + protein) |
Tips for Implementation
- Start small: Begin by adding just one balanced meal per day
- Prep in advance: Keep protein and fiber-rich foods readily available
- Read labels: Many “low-fat” products replace fat with sugar
- Stay hydrated: Water helps fiber work effectively for blood sugar control
Even when eating out, you can maintain this balance by choosing dishes with protein and non-starchy vegetables, and limiting refined carbohydrates. For example, order a protein with double vegetables instead of rice, or ask for salad instead of fries.
Conclusion: Your Path to Natural Blood Sugar Control
Controlling blood sugar doesn’t require restrictive diets or complex regimens. The five evidence-based strategies we’ve explored offer practical approaches that can fit into your everyday life:
- Meal Sequencing: Eat vegetables and protein before carbohydrates to reduce glucose spikes
- The Vinegar Strategy: Use 1-2 tablespoons before meals to improve insulin sensitivity
- Strategic Carbohydrate Management: Choose lower glycemic options and leverage resistant starch
- Post-Meal Movement: Take a 15-minute walk after eating to activate glucose uptake in muscles
- Protein, Fat, and Fiber Balance: Structure meals with this blood sugar-stabilizing trio
“The most effective approach to blood sugar management combines multiple complementary strategies rather than relying on a single intervention. I’ve observed that patients who implement at least three of these evidence-based techniques together—such as meal sequencing, strategic carbohydrate selection, and post-meal movement—typically achieve more stable glucose levels than those focusing on dietary restriction alone. This multi-faceted approach acknowledges the complex nature of glucose metabolism and provides multiple points of intervention.”
Dr. Babak Jamalian, Family Physician.
While each technique is effective on its own, combining multiple approaches creates synergistic benefits for optimal glycemic control. The research is clear: these natural methods can help maintain stable blood glucose levels as effectively as some medications, but without side effects.
Begin your journey by implementing just one strategy this week. Once it becomes a habit, add another. Small, consistent changes often lead to more sustainable results than attempting a complete lifestyle overhaul all at once.
To access other content on the IFitCenter’s blog, you can use the following links:
References
- Shukla AP, Iliescu RG, Thomas CE, Aronne LJ. Food Order Has a Significant Impact on Postprandial Glucose and Insulin Levels. Diabetes Care. 2015 Jun 11;38(7):e98-e99. doi: 10.2337/dc15-0429
- Engeroff T, Groneberg DA, Wilke J. After Dinner Rest a While, After Supper Walk a Mile? A Systematic Review with Meta-analysis on the Acute Postprandial Glycemic Response to Exercise Before and After Meal Ingestion in Healthy Subjects and Patients with Impaired Glucose Tolerance. Sports Med. 2023 Jan 30;53(4):849-869. doi: 10.1007/s40279-022-01808-7
- Kubota S, Liu Y, Iizuka K, Kuwata H, Seino Y, Yabe D. A Review of Recent Findings on Meal Sequence: An Attractive Dietary Approach to Prevention and Management of Type 2 Diabetes. Nutrients. 2020 Aug 19;12(9):2502. doi: 10.3390/nu12092502
- Qiu S, Cai X, Schumann U, Velders M, Sun Z, Steinacker JM. Impact of Walking on Glycemic Control and Other Cardiovascular Risk Factors in Type 2 Diabetes: A Meta-Analysis. Published: October 17, 2014. doi: 10.1371/journal.pone.0109767



