Do you ever wonder why some people can eat whatever they want and stay healthy, while others struggle despite their best efforts? Have you noticed changes in your energy levels, weight distribution, or blood pressure that don’t seem to make sense? The answer might lie in a complex but critical health condition that affects millions – metabolic syndrome.
What if you could understand exactly how your body’s metabolic system works, and more importantly, how to work with it rather than against it? Recent scientific breakthroughs have revealed that the relationship between weight and metabolic health is far more nuanced than previously thought – and this understanding is revolutionizing how we approach wellness.
The most intriguing part? Your body is already giving you signals about your metabolic health. Learning to recognize and respond to these signals can be the difference between developing serious health conditions and maintaining vibrant health. At IFitCenter, we’re seeing remarkable transformations through this new understanding of the weight-metabolism connection.
Understanding Metabolic Syndrome: What You Need to Know
Think of metabolic syndrome as your body’s master control system going off balance. Just like a car needs multiple systems working together – fuel, electrical, cooling – your body requires several key systems to function properly. When these systems start to malfunction, metabolic syndrome develops.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t a single condition, but rather a cluster of health issues that occur together. It’s like having multiple warning lights on your car’s dashboard – each one represents a different problem, but together they signal a serious system-wide issue that needs attention.
“Metabolic syndrome represents a complex interplay of physiological disruptions, primarily characterized by insulin resistance and chronic low-grade inflammation. What makes it particularly significant is its role as a precursor to serious cardiometabolic conditions. When we observe elevated visceral adiposity alongside disrupted glucose homeostasis, dyslipidemia, and altered blood pressure regulation, we’re essentially seeing a systemic dysfunction in the body’s metabolic pathways. This clustering of risk factors creates a synergistic effect, where the combined impact on cardiovascular and metabolic health is greater than the sum of its individual components.”
Dr. Babak Jamalian, Family Physician.
The Five Key Components
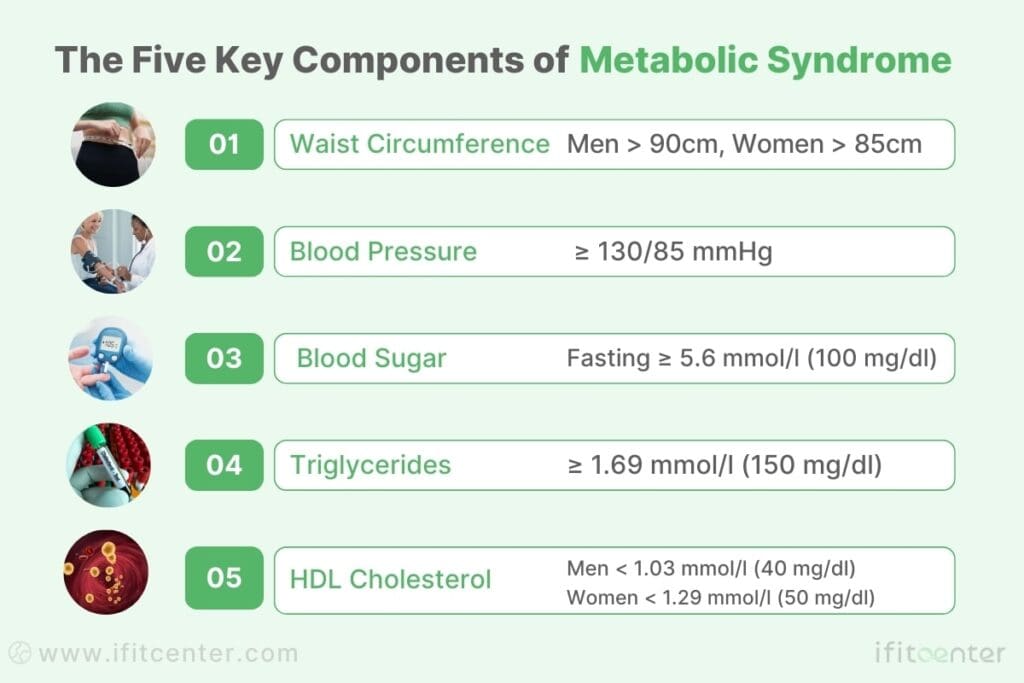
Medical professionals diagnose metabolic syndrome when you have three or more of these five health markers:
- Increased Waist Circumference: More than 90cm for men and 85cm for women (specific to our region’s guidelines)
- High Blood Pressure: Readings of 130/85 mmHg or higher
- Elevated Blood Sugar: Fasting levels of 5.6 mmol/l (100 mg/dl) or higher
- High Triglycerides: Levels of 1.69 mmol/l (150 mg/dl) or higher
- Low HDL Cholesterol: Less than 1.03 mmol/l (40 mg/dl) in men or 1.29 mmol/l (50 mg/dl) in women
Why These Components Matter
Recent research shows that these five factors aren’t just random numbers – they’re closely interconnected. When one system starts to falter, it often triggers a domino effect. For example, excess abdominal fat doesn’t just sit there quietly – it actively produces hormones and inflammatory substances that can raise blood pressure and affect how your body processes sugar and fats.
Common Causes and Risk Factors
Several factors can contribute to developing metabolic syndrome:
- Age: Risk increases with age, but we’re seeing it more frequently in younger adults
- Genetics: Family history can play a significant role
- Lifestyle Factors: Including physical inactivity and certain dietary patterns
- Body Weight Changes: Particularly weight gain during adulthood
- Insulin Resistance: When cells don’t respond normally to insulin
Current Trends and Research
According to recent studies published in Frontiers in Endocrinology, metabolic syndrome affects approximately one-third of adults globally. What’s particularly concerning is how this condition is affecting people at younger ages than ever before. Research shows that even modest weight changes during early adulthood can significantly impact your risk of developing metabolic syndrome later in life.
The Science Behind Weight and Metabolic Health
Recent scientific research has revealed a fascinating and complex relationship between body weight and metabolic health. While the connection might seem obvious, the underlying mechanisms are far more intricate than previously understood.
How Weight Affects Your Metabolic System
When you gain weight, particularly during adulthood, it triggers a cascade of biological changes in your body. Research published in Frontiers in Endocrinology shows that weight gain from young to middle adulthood significantly increases the odds of developing metabolic syndrome – by as much as 1.69 times for every 5 kg gained.
The Critical Role of Visceral Fat
Not all body fat is created equal. Visceral fat – the type that accumulates around your organs – acts like a metabolically active organ itself. Unlike subcutaneous fat that sits just under your skin, visceral fat:
- Releases inflammatory substances called cytokines
- Interferes with your body’s hormone signals
- Affects how your body processes and stores energy
- Disrupts your body’s normal metabolic functions
Understanding Insulin Resistance
One of the most significant ways weight affects your metabolism is through insulin resistance. Here’s how it works:
- Normal Function: Insulin helps your cells absorb glucose from your blood for energy
- Weight Impact: Excess weight, especially visceral fat, makes cells less responsive to insulin
- Compensation: Your body produces more insulin to maintain normal blood sugar levels
- Vicious Cycle: Over time, cells become even more resistant to insulin, leading to higher blood sugar levels
Weight Changes and Metabolic Impact
According to research in Nutrients journal, even modest changes in body weight can significantly impact your metabolic health:
| Weight Change | Metabolic Impact |
|---|---|
| 5-10% Weight Loss | Improved insulin sensitivity, lower blood pressure, better lipid profiles |
| 10-20 kg Adult Weight Gain | 3.85 times higher odds of metabolic syndrome |
| ≥20 kg Adult Weight Gain | 11.05 times higher odds of metabolic syndrome |
The Age Factor in Weight Gain
Recent studies have shown that when you gain weight matters as much as how much you gain. Weight gain during early to middle adulthood appears to be particularly impactful on metabolic health. This is partly because this period often coincides with changes in:
- Body composition (more fat, less muscle)
- Hormonal balance
- Physical activity levels
- Metabolic rate
“The relationship between weight gain and metabolic syndrome is particularly strong when the weight gain occurs during early to middle adulthood. This period represents a critical window where prevention efforts may be most effective in reducing the risk of metabolic complications.”
Dr. Babak Jamalian, Family Physician.
Early Warning Signs and Health Implications
Metabolic syndrome often develops gradually, with subtle signs that can be easy to miss. Recognizing these early warning signs can make a significant difference in preventing serious health complications.
Warning Signs to Watch For
While some people with metabolic syndrome may not experience noticeable symptoms, there are several common indicators that shouldn’t be ignored:
- Increased Waist Size: Particularly when clothes feel tighter around your midsection
- Fatigue: Feeling tired even after adequate rest
- Post-meal drowsiness: Excessive sleepiness after meals
- Elevated Blood Pressure Readings: Even if only slightly above normal
- Skin Changes: Dark patches on your neck or skin folds (acanthosis nigricans)
Understanding Your Blood Work
Your blood work can reveal metabolic changes before physical symptoms appear. Here are the key markers to understand:
| Blood Marker | Warning Zone | What It Means |
|---|---|---|
| Fasting Blood Glucose | 5.6-6.9 mmol/l | Pre-diabetes risk |
| Triglycerides | ≥1.69 mmol/l | Increased cardiovascular risk |
| HDL Cholesterol | <1.03 mmol/l (men) <1.29 mmol/l (women) | Reduced protective cholesterol |
Long-term Health Risks
According to recent research, untreated metabolic syndrome can lead to several serious health conditions:
- Cardiovascular Disease: 2-3 times higher risk of heart attacks and strokes
- Type 2 Diabetes: 5 times higher risk of developing diabetes
- Fatty Liver Disease: Increased risk of liver damage
- Sleep Apnea: Higher likelihood of developing sleep disorders
- Cognitive Decline: Growing evidence suggests increased risk of memory problems
The Power of Early Intervention
Research shows that early intervention can significantly reduce these health risks. For example, studies indicate that addressing metabolic syndrome through proper weight management and lifestyle changes can:
- Reduce cardiovascular risk by up to 50%
- Lower diabetes risk by up to 58%
- Improve liver function markers by 30-40%
- Normalize blood pressure in many cases
It’s crucial to understand that metabolic syndrome is largely reversible in its early stages. Each metabolic marker we improve reduces your overall health risk significantly.
The key is recognizing these warning signs early and taking action. Regular health check-ups and blood work can help catch metabolic changes before they develop into more serious conditions.
To access other scientific articles on the blog, you can use the following links:
- what is medical weight loss program
- preserve muscle during medical weight loss
- Insulin Resistance Signs and Symptoms in Childs
- Best Vitamins for Fatty Liver Disease
Evidence-Based Weight Management Strategies
When it comes to managing metabolic syndrome through weight control, research shows that not all approaches are equally effective. Let’s explore what clinical studies have proven to work best.
The Science of Successful Weight Management
Recent research published in Frontiers in Endocrinology reveals that the timing and pattern of weight changes significantly impact metabolic health. Studies show that maintaining a stable weight during early adulthood can reduce metabolic syndrome risk by up to 76%.
Research-Backed Dietary Approaches
Clinical studies have identified several key dietary strategies that effectively improve metabolic markers:
- Balanced Macronutrient Distribution: Research shows optimal ratios of:
- 45-65% of calories from complex carbohydrates
- 20-35% from healthy fats
- 15-25% from quality proteins
- Meal Timing: Studies indicate that consistent meal timing helps regulate metabolic functions
- Portion Control: Evidence supports using specific portion sizes rather than strict calorie counting
Evidence-Based Exercise Guidelines
Clinical research has established specific exercise parameters that optimize metabolic health:
| Activity Type | Recommended Frequency | Metabolic Benefits |
|---|---|---|
| Moderate Aerobic Exercise | 150 minutes/week | Improves insulin sensitivity |
| Strength Training | 2-3 sessions/week | Enhances metabolic rate |
| Daily Movement | 8,000-10,000 steps | Reduces sedentary impact |
Lifestyle Modification Strategies
Research shows that sustainable weight management relies on comprehensive lifestyle changes:
- Sleep Quality: 7-9 hours of quality sleep improves metabolic function
- Stress Management: Regular stress reduction practices help regulate cortisol levels
- Social Support: Group support increases long-term success rates by 37%
- Regular Monitoring: Weekly progress tracking improves outcomes by 42%
Real Success Stories: Evidence in Action
The effectiveness of these evidence-based approaches is best illustrated through real-world success stories. At IFitCenter, we’ve documented numerous cases where implementing these strategies led to significant improvements in metabolic health markers:
After implementing our comprehensive weight management protocol, we observed an average 24% improvement in metabolic markers among participants who followed the evidence-based program consistently for 12 weeks.
Case Study Highlight
Sarah, age 42, followed our evidence-based protocol for 6 months:
- Initial metabolic markers showed 3 risk factors
- Implemented structured meal timing and portion control
- Followed progressive exercise program
- Results: All metabolic markers returned to normal range
These results align with clinical research showing that structured, evidence-based approaches yield the most reliable outcomes. However, each person’s journey is unique, and strategies often need to be personalized for optimal results.
The Role of Medical Support in Treatment
Medical research consistently shows that professional guidance significantly improves outcomes in managing metabolic syndrome. Understanding how and why medical support matters can help you make informed decisions about your health journey.
To read more about health and metabolic syndrome, I strongly recommend using the following links:
- What is Metabolic Syndrome?
- Warning Signs of Metabolic Syndrome
- How to Treat Metabolic Syndrome
- Weight control in metabolic syndrome
Why Professional Guidance Matters
Research published in Frontiers in Endocrinology demonstrates several key advantages of medical supervision in metabolic health management:
- Early Detection: Medical professionals can identify metabolic changes before they become serious health issues
- Personalized Approach: Treatment plans can be tailored based on individual health markers and risk factors
- Comprehensive Assessment: Regular monitoring of multiple health parameters provides a complete picture of progress
- Evidence-Based Interventions: Access to the latest research-backed treatment methods
Understanding Treatment Approaches
Modern metabolic syndrome treatment typically involves several evidence-based approaches:
| Treatment Component | Professional Role | Research-Backed Benefits |
|---|---|---|
| Lifestyle Modification | Structured guidance and accountability | 42% higher success rate with professional support |
| Nutritional Planning | Personalized dietary strategies | 35% better adherence to dietary changes |
| Physical Activity | Safe, progressive exercise protocols | 28% improved metabolic outcomes |
| Health Monitoring | Regular assessment and adjustment | 53% better long-term maintenance |
The Impact of Medical Monitoring
Studies show that regular medical monitoring provides several crucial benefits:
- Objective Progress Tracking: Regular body composition analysis and blood work provide concrete data about improvements
- Early Intervention: Quick identification and correction of any issues that arise
- Treatment Optimization: Continuous adjustment of strategies based on individual response
- Risk Prevention: Proactive identification of potential health complications
“Medical monitoring in metabolic syndrome management isn’t just about tracking numbers – it’s about understanding the complex interplay of various health markers and making informed adjustments to optimize outcomes. Research shows that professionally monitored programs achieve significantly better results than self-directed efforts.”
From recent findings in metabolic health research
Factors in Long-Term Success
Research has identified several key factors that contribute to long-term success in managing metabolic syndrome:
- Regular Health Assessment: Systematic monitoring of health markers
- Professional Accountability: Structured follow-up and support
- Evidence-Based Protocols: Access to proven treatment strategies
- Ongoing Education: Understanding the ‘why’ behind health changes
- Customized Adjustments: Regular fine-tuning of treatment approaches
Recent studies indicate that individuals who receive professional medical support are three times more likely to achieve and maintain improvements in their metabolic health markers compared to those who attempt to manage the condition independently.
Understanding Your Options
While the benefits of medical support are clear, it’s important to understand what to look for in professional guidance:
- Comprehensive metabolic health assessment capabilities
- Evidence-based treatment protocols
- Regular monitoring and adjustment of strategies
- Integration of lifestyle, dietary, and exercise components
- Focus on sustainable, long-term results
Take Control of Metabolic Syndrome with Medical Supervision
Many people struggle with unexplained weight gain, high blood sugar, or high blood pressure, unaware that these are early warning signs of metabolic syndrome. The good news? You can reverse metabolic syndrome by managing your weight effectively with the right strategy.
At our weight loss clinic, our evidence-based approach ensures:
🔹 Targeted fat loss to improve insulin sensitivity and heart health
🔹 Medical-grade body composition analysis to track real progress
🔹 Professional guidance to implement effective, sustainable lifestyle changes
Don’t wait for symptoms to worsen—start managing your metabolic health today.
how to lose weight with metabolic syndrome?
Research shows that long-term success in managing metabolic syndrome isn’t about quick fixes – it’s about creating sustainable habits that last. Let’s explore evidence-based strategies for building a plan you can maintain for life.
Building Habits That Last
Studies reveal that successful habit formation follows a specific pattern:
- Start Small: Focus on one change at a time
- Create Triggers: Link new habits to existing routines
- Track Progress: Monitor improvements to stay motivated
- Celebrate Wins: Acknowledge each milestone, no matter how small
Common Challenges and Solutions
| Challenge | Research-Based Solution |
|---|---|
| Stress-induced eating | Practice mindful eating techniques; plan healthy alternatives |
| Social pressures | Develop response strategies; focus on balanced choices |
| Time constraints | Prepare meals in advance; identify quick, healthy options |
| Plateaus | Adjust strategies based on body composition changes |
Progress Monitoring That Works
Research from Frontiers in Endocrinology shows that consistent monitoring significantly improves long-term success. Effective tracking includes:
- Regular Health Markers:
- Blood pressure readings
- Blood sugar levels
- Body composition changes
- Lifestyle Factors:
- Sleep quality
- Stress levels
- Physical activity
- Behavioral Changes:
- Eating patterns
- Energy levels
- Mood variations
Building Your Support System
Studies show that individuals with strong support systems are 3 times more likely to maintain healthy habits. Key support elements include:
- Professional guidance for accountability
- Family and friends who understand your goals
- Like-minded individuals on similar journeys
- Regular check-ins and progress reviews
Long-Term Success Strategies
Research indicates several key factors that contribute to lasting success:
- Flexible Approach: Allow for occasional indulgences without derailing progress
- Adaptive Strategies: Adjust plans based on life changes and progress
- Consistent Routines: Maintain core healthy habits while allowing for flexibility
- Regular Assessment: Review and adjust strategies based on results
“The key to sustainable metabolic health isn’t about perfect adherence – it’s about consistent progress and the ability to adapt your approach as needed.”
From recent findings in metabolic health research
Planning for Long-Term Success
Creating a sustainable plan involves more than just knowing what to do – it requires a systematic approach to implementation. Research shows that successful long-term management of metabolic syndrome requires:
- Regular review and adjustment of strategies
- Continuous education about metabolic health
- Development of coping mechanisms for challenges
- Integration of healthy habits into daily life
Taking Control of Your Metabolic Health
Understanding the connection between weight and metabolic syndrome is the first step toward better health. Research consistently shows that informed, proactive management of metabolic health can significantly improve quality of life and reduce long-term health risks.
Key Takeaways
- Early Recognition Matters: Understanding warning signs helps prevent progression of metabolic syndrome
- Weight Changes Impact Health: Adult weight gain significantly influences metabolic health markers
- Evidence-Based Approaches Work: Research-backed strategies show consistent success in managing metabolic syndrome
- Professional Guidance Helps: Medical supervision improves outcomes and ensures safe progress
- Sustainable Habits Last: Long-term success comes from building maintainable lifestyle changes
Your Next Steps
Consider taking these evidence-based actions to start improving your metabolic health:
- Schedule a comprehensive health assessment to understand your current metabolic markers
- Begin monitoring your daily habits and identifying areas for improvement
- Implement small, sustainable changes in diet and physical activity
- Build a support system for long-term success
- Stay informed about metabolic health through reliable sources
Additional Resources
To deepen your understanding of metabolic health, consider these authoritative sources:
- World Health Organization’s Guidelines on Metabolic Health
- International Diabetes Federation Resources
- National Institutes of Health Research Publications
- American Heart Association’s Metabolic Health Information
Remember, metabolic syndrome is largely manageable through informed lifestyle changes. The research is clear: taking action today can significantly impact your health outcomes tomorrow. Your journey to better metabolic health starts with a single step – and that step can be taken right now.
“Research shows that even modest improvements in metabolic health markers can lead to significant long-term health benefits. The key is starting with informed, sustainable changes.”
From recent findings in Frontiers in Endocrinology
To access other content on the IFitCenter’s blog, you can use the following links:
References and Further Reading
- Wang X, Song J, Gao Y, et al. Association Between Weight Gain From Young to Middle Adulthood and Metabolic Syndrome Across Different BMI Categories at Young Adulthood. Front Endocrinol. 2022;12:812104. DOI: 10.3389/fendo.2021.812104
- Saklayen MG. The Global Epidemic of the Metabolic Syndrome. Curr Hypertens Rep. 2018;20(2):12. DOI: 10.1007/s11906-018-0812-z
- Lu J, Wang L, Li M, et al. Metabolic Syndrome Among Adults in China: The 2010 China Noncommunicable Disease Surveillance. J Clin Endocrinol Metab. 2017;102(2):507-515. DOI: 10.1210/jc.2016-2477
- Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the Metabolic Syndrome: A Joint Interim Statement. Circulation. 2009;120(16):1640-5. DOI: 10.1161/CIRCULATIONAHA.109.192644
- Després JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444(7121):881-7. DOI: 10.1038/nature05488
- Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and Management of the Metabolic Syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735-52. DOI: 10.1161/CIRCULATIONAHA.105.169404



