Did you know that over 45% of patients attempting to treat insulin resistance focus solely on blood sugar levels, potentially missing the most effective treatment approaches? This common misconception leads many to overlook crucial aspects of insulin resistance treatment that could dramatically improve their results.
Here at IFitCenter, we frequently encounter questions about treating insulin resistance effectively. The most common concern? “I’ve tried everything, but nothing seems to work.” The reality is that successful treatment of insulin resistance isn’t about finding a single solution – it’s about understanding and implementing a comprehensive approach that addresses multiple aspects of metabolic health.
Think of insulin resistance like a stuck door in your house. Just as you wouldn’t keep pushing harder on a stuck door (which might actually make the problem worse), simply taking medication or following a strict diet alone isn’t always the answer. Instead, you need to understand why the door is stuck and address the root causes – maybe the hinges need oil, or the frame has shifted. Similarly, treating insulin resistance effectively requires a thorough understanding of various treatment approaches and how they work together.
In this comprehensive guide, we’ll explore both natural and medical treatment options for insulin resistance, backed by the latest scientific research. You’ll discover why some treatments work better than others, what the scientific evidence says about each approach, and how to implement them effectively in your daily life.
Can Insulin Resistance be Reversed?
Just as a car needs the right type of fuel and proper maintenance to run efficiently, your body requires specific dietary and lifestyle adjustments to overcome insulin resistance naturally. Research shows that natural interventions can improve insulin sensitivity by up to 58% when properly implemented.
Evidence-Based Dietary Interventions for Insulin Resistance Reversal
Think of insulin as a key that unlocks your cells to let glucose in. When you have insulin resistance, this key doesn’t work as well. However, certain dietary choices can help “repair the lock” and make insulin more effective again.
“One of the most overlooked aspects of insulin resistance treatment is meal timing and sequence. Most people focus solely on what they eat, but in my clinical experience, eating protein and vegetables before carbohydrates in a meal can reduce the insulin response by up to 30%. This simple change in meal sequence, which requires no dietary restrictions, can significantly improve treatment outcomes.” Dr. Babak Jamalian, Family Physician.
On the IFitCenter blog, we have published a free content bank about insulin resistance that can have a significant impact for you in controlling and preventing this metabolic disease. For access, simply use the links below:
- understanding insulin resistance
- insulin resistance symptoms
- insulin resistance test
- foods for insulin resistance
- Can Fasting Reverse Insulin Resistance?
Optimal Nutrient Balance
Research suggests the following optimal ratios for improving insulin sensitivity:
- Proteins: 25-30% of daily calories
- Healthy fats: 30-35% of daily calories
- Complex carbohydrates: 35-45% of daily calories
Foods That Enhance Insulin Sensitivity

- High-fiber vegetables: Act like natural blood sugar regulators
- Fatty fish: Rich in omega-3s that improve cell membrane function
- Lean proteins: Support muscle maintenance without spiking insulin
- Berries: Contain compounds that enhance insulin signaling
Strategic Meal Timing
Recent studies show that when you eat can be just as important as what you eat. Consider implementing these evidence-based timing strategies:
- Allow 4-5 hours between meals
- Finish eating 3 hours before bedtime
- Consider a 12-14 hour overnight fasting window
Foods to Avoid
Just as certain foods can improve insulin sensitivity, others can worsen insulin resistance:
- Refined carbohydrates and sugars
- Processed vegetable oils high in omega-6
- Excessive alcohol
Exercise Protocols for Treating Insulin Resistance
Think of exercise as a master switch that can temporarily bypass insulin resistance. When you exercise, your muscles can take in glucose even without insulin’s help – like having a spare key for your cells.
“Many patients are surprised to learn that short bursts of movement throughout the day can be more effective for insulin sensitivity than a single long workout. I’ve observed that taking a 2-3 minute walk after meals, combined with standing up every hour, can improve insulin sensitivity markers more effectively than a 45-minute workout followed by prolonged sitting. It’s not about finding time for long exercise sessions – it’s about breaking up sedentary periods.” Dr. Babak Jamalian, Family Physician.
Most Effective Exercise Types
- Resistance Training: Creates more “glucose storage space” by building muscle
- High-Intensity Interval Training (HIIT): Improves insulin sensitivity for up to 48 hours
- Moderate-intensity cardio: Enhances overall metabolic health
For optimal results, combine these types throughout the week, allowing for proper recovery between sessions.
Exercise Timing
New research suggests that evening exercise might be particularly effective for insulin resistance, though any consistent exercise timing can be beneficial. Aim for:
- 30-45 minutes per session
- 3-5 sessions per week
- At least 150 minutes total weekly activity
Lifestyle Modifications for Insulin Resistance Treatment
Managing insulin resistance extends beyond diet and exercise. Consider these crucial lifestyle factors:
Sleep Optimization
- Aim for 7-9 hours of quality sleep
- Maintain consistent sleep-wake times
- Create a cool, dark sleeping environment
Stress Management
Chronic stress can worsen insulin resistance by elevating cortisol levels. Implement these strategies:
- Regular meditation or deep breathing exercises
- Time in nature
- Regular social connections
- Mindfulness practices
Remember, these natural treatments work synergistically. Like a well-conducted orchestra, each element plays its part in improving insulin sensitivity.
Medical Treatment Options for Insulin Resistance
While lifestyle changes form the foundation of insulin resistance treatment, some individuals may require medical intervention. It’s crucial to understand these options while recognizing that medication should complement, not replace, lifestyle modifications.
Understanding Medications Used to Treat Insulin Resistance
Think of insulin resistance medications like different types of keys – each designed to unlock your body’s ability to use insulin more effectively, but in slightly different ways. However, these medications require careful consideration and professional guidance.
Common Prescription Medications
- Insulin sensitizers: Help cells respond better to insulin
- GLP-1 receptor agonists: Improve insulin release and sensitivity
- DPP-4 inhibitors: Help maintain natural insulin regulation
⚠️ Important: Never start or modify medication without professional medical supervision. Self-medication can lead to serious complications and mask underlying health issues.
Understanding Metformin for Insulin Resistance Treatment
Metformin stands out as one of the most studied medications for insulin resistance. However, its effectiveness depends on proper use and understanding.
To access the second part of the insulin resistance content, I invite you to use the links below:
- insulin resistance in kids
- supplements for insulin resistance
- how to stop insulin weight gain
- can insulin resistance lead to diabetes
- How Long Does Insulin Resistance Treatment Take?
How Metformin Works
Imagine your liver as a sugar factory. In insulin resistance, this factory often produces too much sugar. Metformin helps regulate this production while improving how your body responds to insulin.
Clinical Research Findings
Recent studies demonstrate that metformin can improve insulin sensitivity To an appreciable extent when combined with lifestyle changes. However, these results vary significantly between individuals.
Potential Side Effects
- Digestive discomfort (most common)
- Vitamin B12 deficiency (with long-term use)
- Temporary fatigue or weakness
🔔 Medical Supervision: Regular monitoring is essential to ensure safe and effective treatment with metformin. Your doctor should track your progress and adjust dosage as needed.
Emerging Medical Treatments for Insulin Resistance
The field of insulin resistance treatment continues to evolve, with promising new approaches on the horizon.
Latest Treatment Developments
- New insulin sensitizers: Target specific cellular pathways
- Gut microbiome therapies: Focus on metabolic health
- Targeted anti-inflammatory treatments: Address underlying causes
Clinical Trial Insights
Some studies suggest that combination approaches that target multiple aspects of insulin resistance may have better outcomes than single-drug therapies, but more research is needed.
Remember, medical treatments work best when integrated into a comprehensive approach that includes proper diet, exercise, and lifestyle modifications. The key is finding the right combination under professional guidance.
Reversing Insulin Resistance with a Medically Supervised Plan
If you’ve been struggling to improve your insulin sensitivity despite making changes, a personalized, medically supervised plan may be the missing piece. At IFitCenter, we take a scientific, multi-faceted approach to insulin resistance treatment, ensuring that every intervention is based on clinical evidence and tailored to your body’s response.
Our expert-led program, supervised by Dr. Babak Jamalian, includes:
✔ Detailed metabolic screening to pinpoint the root causes of insulin resistance
✔ Professional guidance on meal timing, nutrition, and exercise for maximum impact
✔ Ongoing monitoring and treatment adjustments for sustained, long-term success
Reversing insulin resistance requires more than general advice—it demands a strategic, science-backed plan. Start your journey toward better metabolic health today.
Professional Medical Treatment Programs for Insulin Resistance
A comprehensive medical treatment program for insulin resistance goes beyond simple dietary advice or medication prescriptions. It requires a systematic approach that addresses multiple aspects of metabolic health simultaneously.
Components of Professional Treatment Programs
At IFitCenter, under the medical supervision of Dr. Babak Jamalian, treatment programs integrate multiple components to ensure optimal results. Each program includes:
- Initial Health Assessment: Comprehensive blood work analysis measuring 72 different parameters
- Body Composition Analysis: Regular InBody scans to track changes in muscle mass and body fat
- Customized Treatment Plans: Individually tailored protocols based on your specific metabolic profile
- Ongoing Medical Supervision: Regular consultations to ensure safe and effective progress
The Role of Professional Medical Supervision
Professional medical supervision ensures that your treatment journey is both safe and effective. Dr. Babak Jamalian’s approach includes:
- Regular monitoring of key health markers
- Timely adjustments to treatment protocols
- Professional guidance through challenges
- Integration of latest treatment methods
Regular Monitoring and Progress Tracking
Treatment success relies heavily on consistent monitoring. The IFitCenter monitoring system includes:
- Bi-weekly body composition analyses
- Regular blood work review
- Progress photo documentation
- Detailed measurement tracking
Integrating Different Treatment Approaches
A successful treatment program combines multiple approaches in a synchronized manner. At IFitCenter, this includes:
- Scientifically formulated nutrition protocols
- Customized exercise recommendations
- Lifestyle modification guidance
- Medical intervention when necessary
Through this comprehensive approach, patients receive the support and guidance needed to achieve lasting improvements in their insulin sensitivity and overall metabolic health.
Monitoring Your Insulin Resistance Treatment Progress
Successfully treating insulin resistance isn’t just about following a treatment plan – it’s about understanding and tracking your progress. Think of monitoring your treatment like using a GPS during a journey; it helps you know if you’re moving in the right direction and when you need to make adjustments.
Essential Markers to Track During Treatment
Several key indicators can help you measure improvements in insulin sensitivity:
- Primary Markers:
- Fasting insulin levels
- Triglyceride to HDL ratio
- Fasting blood glucose
- Waist circumference
- Secondary Markers:
- Blood pressure readings
- Body composition changes
- Energy levels
- Sleep quality
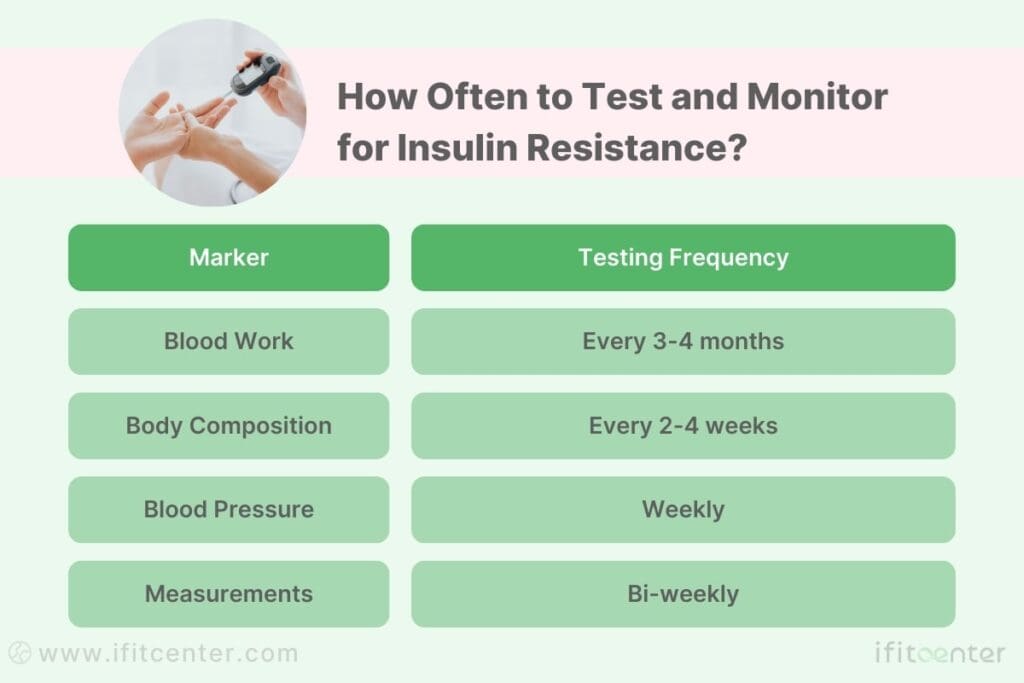
How Often to Test and Monitor
Different markers require different monitoring schedules for optimal tracking:
Recognizing Signs of Improvement
Progress in treating insulin resistance often appears in stages:
- Early Signs (2-4 weeks):
- Improved energy levels
- Better sleep quality
- Reduced sugar cravings
- Intermediate Signs (1-3 months):
- Reduced waist circumference
- Improved blood pressure
- More stable mood and energy
- Long-term Signs (3-6 months):
- Normalized blood markers
- Sustainable weight management
- Improved metabolic flexibility
When to Adjust Your Treatment Approach
Consider adjusting your treatment plan if you notice:
- No improvements in markers after 6-8 weeks
- Plateau in progress for more than 3 weeks
- Unexpected changes in blood markers
- New symptoms or concerns
Remember that small adjustments are often more effective than dramatic changes. Always consult with your healthcare provider before making significant modifications to your treatment plan.
Successful monitoring is about consistency and understanding what your results mean. Track your progress systematically, and you’ll be better equipped to make informed decisions about your treatment journey.
Maintaining Long-Term Results in Insulin Resistance Treatment
Successfully treating insulin resistance is like building a house – the initial construction is crucial, but maintaining it over time requires consistent care and attention. Understanding how to maintain your results can mean the difference between lasting success and frustrating setbacks.
Sustainable Strategies for Long-Term Success
Long-term success requires strategies that you can maintain for life, not just for a few weeks or months:
- Build Sustainable Habits:
- Create realistic meal plans you enjoy
- Choose physical activities that bring satisfaction
- Develop stress management routines that fit your lifestyle
- Establish consistent sleep patterns
- Monitor Key Indicators:
- Regular body composition checks
- Periodic blood work review
- Energy level tracking
- Sleep quality assessment
Preventing Relapse in Insulin Resistance
Understanding common relapse triggers helps you develop effective prevention strategies:
- Early Warning Signs:
- Return of sugar cravings
- Decreased energy levels
- Changes in sleep patterns
- Increased stress sensitivity
- Prevention Strategies:
- Regular progress tracking
- Maintaining support systems
- Planning for high-risk situations
- Regular health check-ups
Integrating Healthy Habits Into Daily Life
Success comes from making healthy choices part of your normal routine, not seeing them as temporary restrictions:
- Social Situations:
- Strategies for dining out
- Handling family gatherings
- Managing workplace challenges
- Travel planning techniques
- Daily Routines:
- Meal preparation systems
- Exercise scheduling
- Stress management practices
- Sleep optimization
Overcoming Common Maintenance Challenges
| Challenge | Solution |
| Time constraints | Batch cooking, quick workout routines, efficient meal planning |
| Social pressure | Communication strategies, alternative social activities, healthy dining options |
| Stress eating | Alternative stress management techniques, mindfulness practices |
| Travel disruptions | Portable healthy snacks, hotel room exercises, restaurant navigation skills |
Remember that maintaining your results doesn’t mean perfection. It’s about creating a sustainable lifestyle that supports your metabolic health while being flexible enough to enjoy life’s moments. The key is finding the right balance between vigilance and flexibility.
Success in maintaining your results comes from viewing your healthy habits not as restrictions, but as choices that empower you to live your best life. When challenges arise, remember why you started this journey and focus on the positive changes you’ve experienced.
Insulin Resistance Natural Cure – Next Steps
Throughout this guide, we’ve explored the comprehensive approach needed to effectively treat insulin resistance. Let’s review the key elements that contribute to successful treatment and outline your path forward.
Key Treatment Principles to Reversing Insulin Resistance
- Natural Treatments:
- Evidence-based dietary modifications
- Strategic exercise protocols
- Essential lifestyle changes
- Medical Interventions:
- Professional treatment options
- Medication considerations
- Regular monitoring protocols
- Long-term Success:
- Progress tracking methods
- Sustainable lifestyle integration
- Relapse prevention strategies
The Role of Professional Guidance
Treating insulin resistance effectively requires more than just information – it needs proper implementation and monitoring. Professional medical guidance ensures:
- Accurate diagnosis and monitoring
- Personalized treatment strategies
- Safe and effective progress
- Proper treatment adjustments when needed
Your Action Plan: Next Steps
To begin your journey toward improved insulin sensitivity, consider these steps:
- Schedule a comprehensive health assessment
- Begin implementing basic lifestyle changes
- Establish your monitoring system
- Create a sustainable daily routine
- Build your support network
Remember, improving insulin sensitivity is a journey, not a destination. Small, consistent steps forward will lead to significant improvements in your metabolic health over time. The key is to start with evidence-based approaches and maintain them with professional guidance and support.
Ready to take control of your metabolic health? Work with healthcare professionals who understand the complexities of insulin resistance and can guide you through your treatment journey. Your path to better health starts with that first step.
To access other content on the IFitCenter’s blog, you can use the following links:
References for “How do You Reverse Insulin Resistance?”
- Lin YC, Chang YH, Hwang SJ, et al. Effect of dietary glycemic index on insulin resistance in adults without diabetes mellitus: A systematic review and meta-analysis. Frontiers in Nutrition. 2025;12:1458353.
- Zhang X, Zhang J, Yang X, et al. Trends in insulin resistance: insights into mechanisms and therapeutic targets. Signal Transduction and Targeted Therapy. 2022;7:1-32. DOI: 10.1038/s41392-022-01073-0.
- Petersen KF, Dufour S, Savage DB, et al. Reversal of muscle insulin resistance with exercise reduces postprandial hepatic de novo lipogenesis in insulin resistant individuals. Proceedings of the National Academy of Sciences. 2011;108(33):13705-13709. DOI: 10.1073/pnas.1110105108.
- Zhang Y, Yuan C, Gao J, et al. Fecal microbiota transplantation reverses insulin resistance in type 2 diabetes mellitus. Frontiers in Cellular and Infection Microbiology. 2023;13:1089991. DOI: 10.3389/fcimb.2022.1089991.
- American Diabetes Association. (2024). “Standards of Medical Care in Diabetes.” Diabetes Care, 47(Supplement 1). DOI: 10.2337/dc24-Sint
- Endocrine Society Clinical Practice Guidelines. (2023). “Treatment of Insulin Resistance.” Journal of Clinical Endocrinology & Metabolism, 108(2), 379-404.



