What if the most powerful intervention for insulin resistance isn’t what you eat, but when you don’t eat? Could extending the time between meals outperform medications for improving insulin sensitivity? These questions are at the heart of research on intermittent fasting for insulin resistance—a condition where cells become increasingly unresponsive to insulin’s signals, affecting millions of people worldwide.
At IFitCenter, we’re examining the science behind fasting and insulin resistance to understand this powerful relationship. The evidence reveals surprising insights: eating identical foods within an early 8-hour window dramatically improves metabolic health compared to consuming them over 14 hours, and strategic meal timing can trigger changes in gene expression that govern glucose metabolism. We’ll explore which fasting approaches have the strongest research support for reversing insulin resistance.
The Relationship Between Fasting and Insulin Function
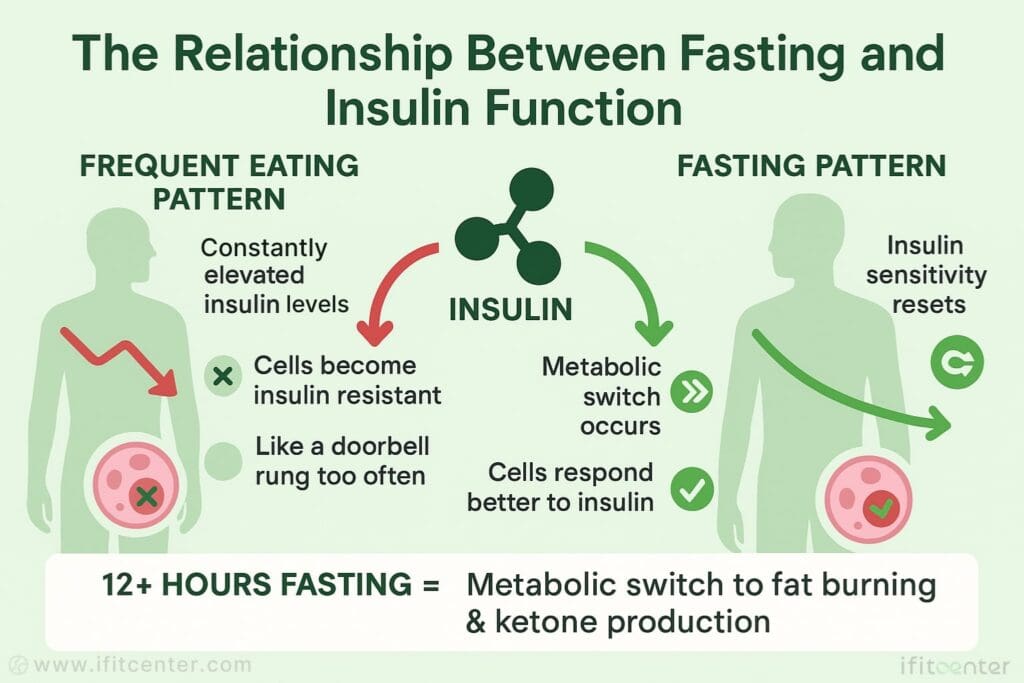
To understand how fasting affects insulin resistance, we first need to examine what happens to insulin and glucose in your body during periods without food. When you eat, especially carbohydrate-rich foods, your blood glucose rises, triggering your pancreas to release insulin. Think of insulin as a key that unlocks cells, allowing glucose to enter and be used for energy. In someone with normal insulin sensitivity, this process works efficiently—like a well-oiled lock and key.
However, with frequent eating—particularly the common pattern of three meals plus snacks throughout the day—insulin levels remain elevated almost continuously. Imagine your cell’s insulin receptors like doorbells that, when rung too frequently, eventually stop getting answered. This is essentially what happens with insulin resistance: cells become increasingly unresponsive to insulin’s signals, requiring more insulin to achieve the same glucose-lowering effect.
The Metabolic Switch During Fasting
When you extend the time between meals through fasting, a remarkable metabolic switch occurs. After approximately 12 hours without food, your body depletes its readily available glucose and glycogen (stored glucose) supplies. This triggers a transition from glucose metabolism to fat metabolism—a state some researchers call “flipping the metabolic switch.”
During this transition, your body begins converting stored fat into ketone bodies, which serve as an alternative fuel source. This process is somewhat like your car switching from gasoline to a reserve fuel tank when the main tank runs empty. These ketones aren’t just an energy substitute—they appear to influence gene expression related to metabolism, potentially improving insulin sensitivity through multiple pathways.,
On the IFitCenter blog, we have published a free content bank about insulin resistance that can have a significant impact for you in controlling and preventing this metabolic disease. For access, simply use the links below:
- understanding insulin resistance
- how to reverse insulin resistance
- insulin resistance symptoms in females
- insulin resistance test
- insulin resistance supplements
How Frequent Eating Patterns Contribute to Insulin Resistance
Modern eating patterns often involve consuming food from early morning until late evening, keeping insulin levels constantly elevated. Research suggests this persistent insulin stimulation is a key driver of insulin resistance. When cells are continuously exposed to insulin, they gradually downregulate their insulin receptors—a protective mechanism to prevent excessive glucose uptake.
Consider your body’s insulin response like a spring that gets compressed each time you eat. With adequate recovery time between meals, the spring fully extends. But with constant compression (frequent eating), the spring loses elasticity over time. Intermittent fasting for insulin resistance works by giving this metaphorical spring time to fully recover, restoring its responsiveness.
Hormonal Changes During Fasting That Benefit Insulin Sensitivity
Fasting triggers several hormonal changes that collectively improve insulin sensitivity. When insulin levels drop during fasting, noradrenaline, growth hormone, and cortisol increase. These counterregulatory hormones help mobilize stored glucose and fat for energy. While this might temporarily raise blood glucose (a phenomenon sometimes observed during fasting), it’s actually part of the body’s adaptive process of accessing stored energy.
Additionally, fasting appears to enhance the expression of SIRT1, a protein involved in regulating metabolism. Think of SIRT1 as a cellular maintenance worker that becomes more active during fasting periods. Research suggests increased SIRT1 activity may improve insulin sensitivity and protect against oxidative stress. Studies examining early time-restricted feeding protocols have reported increased SIRT1 gene expression following these regimens.
Types of Fasting Approaches for Insulin Resistance
Different fasting protocols have shown promise for improving insulin sensitivity, each with unique characteristics that may make them more suitable for different individuals. Let’s explore the most well-researched approaches for addressing insulin resistance.
Time-Restricted Feeding (TRF)
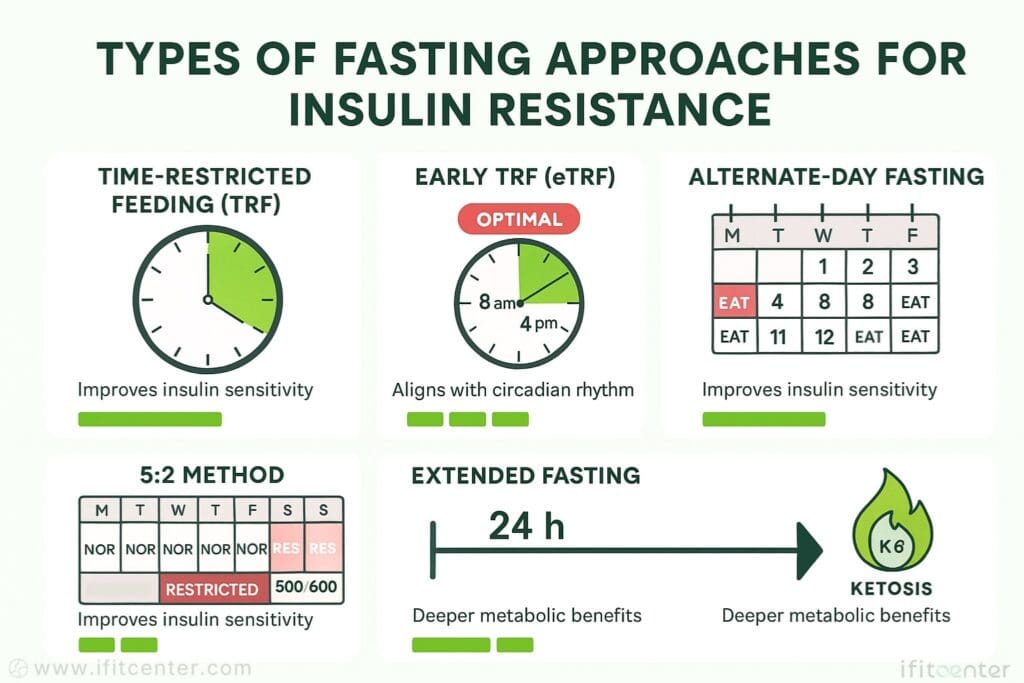
Time-restricted feeding involves limiting daily eating to a specific window (typically 8-10 hours) while fasting for the remaining hours. This approach aligns eating patterns with your body’s natural circadian rhythms. Unlike some other fasting methods, TRF primarily focuses on when you eat rather than reducing calories, though many naturally consume fewer calories when their eating window shrinks.
For insulin resistance, research suggests TRF may improve glycemic responses and insulin sensitivity throughout the day. The simplicity of this approach—for example, eating only between 10am and 6pm—makes it accessible for many people new to fasting.
Early Time-Restricted Feeding (eTRF)
Early time-restricted feeding is a specialized form of TRF where the eating window is positioned earlier in the day—typically starting in the morning and ending in mid-afternoon (e.g., 8am to 4pm). Research indicates this timing may be particularly beneficial for insulin resistance and intermittent fasting outcomes.
The advantage of eTRF appears linked to our body’s natural insulin sensitivity, which is higher in the morning and declines throughout the day. By consuming meals when insulin sensitivity is naturally at its peak, eTRF may enhance the metabolic benefits of fasting. Studies comparing early versus later eating windows show superior improvements in insulin markers with the earlier schedule.
Alternate-Day Fasting
Alternate-day fasting involves cycling between eating normally one day and either completely fasting or significantly restricting calories (usually to about 500-600 calories) the next day. This creates a pattern where the body regularly experiences extended periods without significant food intake.
For those with insulin resistance, this approach provides longer fasting periods that may more thoroughly deplete glycogen stores and extend the metabolic benefits of the fasting state. However, the more extended fasting periods can make this approach challenging for beginners.
The 5:2 Method
The 5:2 method involves eating normally for five days of the week while restricting calories to approximately 500-600 calories on two non-consecutive days. This creates a modified form of intermittent fasting that many find easier to sustain than daily restricted eating windows.
Research has found moderate-quality evidence that the 5:2 diet for insulin resistance can reduce fasting insulin levels in women with overweight or obesity. The approach may be particularly valuable for those who find daily fasting schedules difficult to maintain in their lifestyle.
Extended Fasting
Extended fasting involves periods without caloric intake lasting 24 hours or longer. These longer fasts are typically practiced less frequently—perhaps once a week or once a month—rather than as a daily pattern. During extended fasts, the body moves more deeply into ketosis and autophagy (cellular cleanup).
For insulin resistance, extended fasting may offer more profound metabolic benefits but should be approached cautiously, especially for those with existing health conditions. This approach is generally recommended only after establishing comfort with shorter fasting protocols.
When selecting the best intermittent fasting schedule for insulin resistance, consider not just effectiveness but also sustainability. Research suggests consistency is key—the most effective protocol is one you can maintain over time. For many people, starting with time-restricted eating and gradually extending the fasting window offers a balanced approach to improving insulin sensitivity while adapting to the fasting lifestyle.
Scientific Evidence: What the Research Shows
The relationship between fasting and insulin resistance has been examined through numerous high-quality studies in recent years. Let’s look at what the research reveals about the effectiveness of different fasting approaches.
Time-Restricted Feeding Studies
A systematic review published in Nutrients (2022) analyzed 24 randomized controlled trials on time-restricted feeding and found that TRF may lead to improved insulin sensitivity and glycemic responses throughout the day in individuals with overweight or obesity. The review noted that when combined with caloric restriction, the benefits for metabolic health were even more pronounced.
Particularly notable was the finding that a fasting duration of 14 hours appeared to be as effective as 16 hours for metabolic benefits, suggesting that extreme fasting windows may not be necessary to improve insulin resistance.
Early vs. Mid-Day Time-Restricted Feeding
A revealing randomized controlled trial published in Nature Communications (2022) directly compared early TRF (eating between 6:00-15:00) with mid-day TRF (eating between 11:00-20:00) in healthy volunteers. The results were striking: early TRF was significantly more effective at improving insulin sensitivity.
The early TRF group showed a larger reduction in HOMA-IR (a measure of insulin resistance) compared to both the mid-day TRF group and the control group. This suggests that intermittent fasting for insulin resistance may be optimized by aligning the eating window with the earlier part of the day when insulin sensitivity is naturally higher.
Fasting vs. Continuous Caloric Restriction
A systematic review and meta-analysis published in Nutrients (2024) compared fasting-based strategies to continuous caloric restriction in obese adults. In the short term (up to 6 months), fasting led to a significant reduction in fasting insulin levels and HOMA-IR compared to continuous caloric restriction.
In the long term (beyond 6 months), fasting-based approaches showed a slight but significant reduction in fasting glucose levels. This suggests that fasting to reverse insulin resistance may offer some advantages over traditional calorie-counting approaches, particularly for insulin-related markers.
The 5:2 Diet Evidence
An umbrella review of meta-analyses published in JAMA Network Open (2021) found moderate-quality evidence that the 5:2 diet for 3-6 months was associated with reduced fasting insulin in women with overweight or obesity compared to continuous energy restriction. This supports the 5:2 approach as a viable option for improving insulin markers in this population.
Consistency and Adherence Findings
A secondary analysis of a 14-week randomized trial found that participants who consistently adhered to early time-restricted eating showed significantly greater improvements in insulin resistance and fasting glucose compared to those following a control eating schedule with similar caloric restriction.
This highlights an important point about intermittent fasting and insulin resistance: consistency appears to be key. The most effective fasting schedule for insulin resistance is one that can be maintained regularly over time.
Short-Term vs. Long-Term Effects
Research suggests that metabolic improvements from fasting can begin relatively quickly. Studies show beneficial changes in insulin sensitivity markers within 2-4 weeks of beginning fasting protocols. However, the research also indicates that these benefits become more pronounced and stable with longer adherence.
A notable pattern in the research is that while many fasting approaches show promise for insulin resistance, the early time-restricted feeding pattern (eating earlier in the day) consistently demonstrates superior results for improving insulin sensitivity compared to other timing approaches. This aligns with our understanding of circadian biology and the body’s natural rhythm of insulin sensitivity.
Time-Restricted Eating: Why Timing Matters for Insulin Sensitivity
When it comes to intermittent fasting for insulin resistance, research increasingly shows that when you eat may be just as important as what you eat or how much you fast. The timing of your eating window can significantly impact how your body processes glucose and responds to insulin.
To access the second part of the insulin resistance content, I invite you to use the links below:
- best foods for insulin resistance
- insulin resistance in kids
- how to stop insulin resistance weight gain
- is insulin resistance related to diabetes?
- How Long Does It Take to Reverse Insulin Resistance?
Early vs. Later Eating Windows
A pivotal study published in Nature Communications directly compared early time-restricted feeding (eTRF, eating between 6:00-15:00) with mid-day TRF (eating between 11:00-20:00). The results were clear: the early TRF group showed significantly greater improvement in insulin sensitivity than the mid-day TRF group, despite both groups fasting for the same duration (16 hours).
This finding suggests that for fasting to reverse insulin resistance, an early eating window that aligns with the morning and early afternoon may be more effective than an eating window that extends into the evening.
The Circadian Connection
Our bodies operate on a circadian rhythm—an internal clock that regulates various physiological processes. Insulin sensitivity follows this rhythm, typically peaking during daylight hours and declining in the evening. This natural pattern helps explain why eating earlier in the day may enhance the benefits of intermittent fasting and insulin resistance.
Research indicates that eating in alignment with this natural rhythm—consuming food when insulin sensitivity is naturally higher—may enhance the body’s ability to process glucose efficiently. Conversely, late-night eating occurs when insulin sensitivity is at its lowest, potentially worsening insulin resistance over time.
Morning vs. Evening Metabolism
Studies comparing identical meals consumed at different times of day have found that the same food produces a larger glucose response when eaten in the evening compared to the morning. This difference exists even in healthy individuals, but becomes more pronounced in those with insulin resistance.
The systematic review published in Nutrients noted that early TRF may particularly benefit individuals with impaired glucose metabolism in terms of glycemic control. For those using intermittent fasting for insulin resistance, this timing element could significantly enhance results.
“What many people don’t realize is that the same meal eaten at 9 AM versus 9 PM can have dramatically different effects on insulin response. In my clinical experience, patients who shift their eating window earlier in the day often see more significant improvements in insulin sensitivity than those who simply reduce calories but continue to eat late into the evening. This aligns perfectly with what circadian research is now confirming—our bodies process carbohydrates much more efficiently in the morning and early afternoon.”
Dr. Babak Jamalian, Family Physician.
Optimal Eating Windows Based on Research
Based on current research, the most beneficial fasting schedule for insulin resistance appears to be an early time-restricted feeding pattern with an 8-10 hour eating window that begins in the morning (around 8:00 AM) and ends in the mid-afternoon to early evening (between 4:00-6:00 PM).
This approach creates the “best of both worlds” scenario: it provides a sufficiently long fasting period (14-16 hours) while also aligning food intake with the body’s natural peak insulin sensitivity. Research suggests that this timing approach may be particularly effective for individuals with existing insulin resistance or prediabetes.
For those who find a morning-to-afternoon eating window challenging to maintain due to social or work schedules, even shifting the eating window earlier when possible may provide some benefit compared to extending eating late into the evening. The key insight from the research is that when implementing fasting and insulin resistance protocols, timing deserves as much consideration as fasting duration.
Physiological Mechanisms: How Fasting Improves Insulin Sensitivity
Understanding the biological mechanisms behind fasting and insulin resistance helps explain why this approach can be effective when other interventions fail. Fasting triggers several complementary processes that collectively improve how cells respond to insulin.
Autophagy: Cellular Cleanup and Renewal
Fasting activates autophagy, a process where cells remove damaged components and recycle materials. Think of autophagy as your body’s internal housekeeping service that becomes more active during fasting periods. This cellular cleanup can improve the function of insulin receptors and signaling pathways.
Research shows that energy deficiency during intermittent fasting for insulin resistance downregulates mTOR (a nutrient-sensing protein), which in turn upregulates autophagy. Studies have found that early time-restricted feeding increases expression of autophagy-related genes, potentially contributing to improved metabolic health.
Changes in Gene Expression
Fasting influences the expression of genes involved in metabolism and insulin signaling. When you practice intermittent fasting, your body enhances the expression of genes that promote insulin sensitivity while reducing the expression of genes linked to insulin resistance.
Particularly important are clock genes—those involved in regulating your circadian rhythm. Research suggests that fasting, especially early time-restricted feeding, may enhance the daily rhythms of human clock genes like BMAL1 and PER2, which play key roles in metabolic regulation and insulin sensitivity.
SIRT1 Activation and Insulin Signaling
SIRT1 is a protein that regulates important cellular processes related to metabolism and aging. Fasting for insulin resistance appears to activate SIRT1, which can increase insulin sensitivity and protect against oxidative stress.
Studies examining early time-restricted feeding have reported increased SIRT1 gene expression following these protocols. This increased SIRT1 activity appears to be one of the ways fasting improves metabolic health independently of weight loss.
The Metabolic Switch to Ketones
After approximately 12-14 hours of fasting, the body depletes its readily available glucose and begins producing ketone bodies from stored fat. This “metabolic switch” represents a shift from glucose dependency to fat utilization and ketone production.
Ketones aren’t just alternative fuel—they act as signaling molecules that influence gene expression and cellular function. Mild ketonemia (elevated ketones in the blood) may increase the body’s antioxidant capacity and reduce oxidative stress, which can contribute to improved insulin signaling.
Inflammation Reduction
Chronic low-grade inflammation is closely linked to insulin resistance. Research shows that intermittent fasting and insulin resistance have an inverse relationship partly because fasting reduces inflammatory markers in the body.
Studies have found that fasting, particularly early time-restricted feeding, can decrease inflammatory cytokines like Tumor Necrosis Factor-α (TNF-α) and increase anti-inflammatory components like regulatory T cells. This reduction in inflammation may help restore normal insulin signaling pathways.
Weight Loss vs. Independent Effects
While weight loss typically improves insulin sensitivity, research indicates that fasting to reverse insulin resistance works through mechanisms beyond simple weight reduction. Studies controlling for weight loss show that fasting produces metabolic benefits that cannot be explained by caloric reduction alone.
For example, studies comparing time-restricted feeding to continuous caloric restriction with equivalent weight loss still show superior improvements in insulin sensitivity with the fasting approach. This suggests that the timing of food intake and the fasting-induced cellular processes contribute unique benefits for metabolic health.
These multiple, complementary mechanisms explain why intermittent fasting for insulin resistance can be effective even when other approaches have failed. Rather than targeting a single pathway, fasting creates a comprehensive shift in metabolism that collectively improves how the body processes glucose and responds to insulin.
Factors Affecting Fasting’s Impact on Insulin Resistance
While research supports the effectiveness of fasting for insulin resistance, individual responses can vary significantly. Understanding these variables can help you determine the most effective approach for your specific situation.
Individual Variation in Responses
Not everyone responds identically to the same fasting protocol. Research shows that while most people experience improvements in insulin sensitivity with fasting, the degree of improvement varies widely. Some individuals show dramatic reductions in insulin resistance markers, while others see more modest changes.
This variation means that finding the best intermittent fasting for insulin resistance often requires some personal experimentation. Monitoring your response through periodic blood tests (when possible) can help determine which approach works best for your body.
Baseline Insulin Resistance Severity
The existing severity of insulin resistance appears to influence fasting’s effectiveness. Research suggests that individuals with more pronounced insulin resistance may initially see more dramatic improvements, particularly with consistent adherence to fasting protocols.
Studies examining early time-restricted feeding found that participants with prediabetes or impaired glucose metabolism often experienced greater relative improvements in insulin sensitivity compared to those with normal baseline values. This suggests that fasting to reverse insulin resistance may be particularly valuable for those already showing metabolic dysfunction.
Age and Gender Considerations
Research indicates that age and gender may influence how the body responds to intermittent fasting and insulin resistance protocols. Some studies have found that women may experience different responses to certain fasting protocols than men.
For example, one study noted in the umbrella review found moderate-quality evidence specifically for women with overweight or obesity experiencing reduced fasting insulin with the 5:2 diet. This highlights the importance of considering gender-specific responses when selecting a fasting approach.
Genetic Factors
Emerging research suggests that genetic variations may influence how effectively intermittent fasting for insulin resistance works for different individuals. Genes related to circadian rhythm regulation, glucose metabolism, and fat utilization can all affect how the body responds to fasting.
While personalized genetic testing for fasting response is still in its infancy, this area of research may eventually help explain why some people thrive with certain fasting protocols while others see less benefit from the same approach.
Duration Needed for Results
“The most successful patients I work with understand that consistency trumps perfection when it comes to fasting for insulin resistance. It’s far better to maintain a modest 14-hour overnight fast reliably than to attempt more extreme fasting protocols sporadically. I’ve observed that metabolic improvements typically begin after 3-4 weeks of consistent practice, but the most significant changes in insulin sensitivity often emerge after 2-3 months of regular fasting.”
Dr. Babak Jamalian, Family Physician.
How long does it take for fasting and insulin resistance improvements to become apparent? Research indicates that some metabolic benefits can begin within days, but meaningful changes in insulin sensitivity typically require consistent practice over weeks to months.
Studies examining early time-restricted feeding have shown measurable improvements in insulin markers within 2-4 weeks, but the most significant benefits often emerge after 8-12 weeks of consistent practice. This aligns with the secondary analysis finding that adherent completers who consistently followed their fasting protocol saw greater improvements than those with inconsistent adherence.
The key takeaway is that patience and consistency matter when using fasting for insulin resistance. The best intermittent fasting schedule for insulin resistance is ultimately one that you can maintain consistently over time, as the research suggests that adherence is a critical factor in achieving meaningful metabolic improvements.
Conclusion: Can Fasting Reverse Insulin Resistance?
The scientific evidence clearly supports intermittent fasting for insulin resistance as an effective approach. Research consistently shows that early time-restricted feeding provides the most significant benefits, with eating windows earlier in the day aligning with our natural metabolic rhythms and enhancing insulin sensitivity.
For those looking to implement fasting to reverse insulin resistance, start with a sustainable approach—perhaps a 12-hour overnight fast—and gradually extend your fasting window as your body adapts. Position your eating window earlier in the day when possible, and remember that consistency matters more than intensity.
Emerging research continues to refine our understanding of how individual factors like chronotype, genetics, and baseline metabolic health influence fasting’s effectiveness. While not a standalone solution, intermittent fasting and insulin resistance research suggests this approach can produce meaningful improvements for many people when practiced consistently as part of a comprehensive health strategy.
The most important takeaway? The timing of when we eat deserves as much consideration as what we eat. By aligning our eating patterns with our body’s natural metabolic rhythms through thoughtful fasting protocols, we can potentially unlock significant improvements in insulin sensitivity and overall metabolic health.
To access other content on the IFitCenter’s blog, you can use the following links:
References
- Centofanti, S., Heilbronn, L. K., Wittert, G., Dorrian, J., Coates, A. M., Kennaway, D., Gupta, C., Stepien, J. M., Catcheside, P., Yates, C., Grosser, L., Matthews, R. W., & Banks, S. (2024). Fasting as an intervention to alter the impact of simulated night-shift work on glucose metabolism in healthy adults: a cluster randomised controlled trial. Diabetologia, 68(1), 203-216. DOI: 10.1007/s00125-024-06279-1
- Steger, F. L., Jamshed, H., Bryan, D. R., Richman, J. S., Warriner, A. H., Hanick, C. J., Martin, C. K., Salvy, S., & Peterson, C. M. (2022). Early Time-Restricted Eating Affects Weight, Metabolic Health, Mood, and Sleep in Adherent Completers: A Secondary Analysis. Obesity (Silver Spring), 31(Suppl 1), 96-107. DOI: 10.1002/oby.23614
- Siles-Guerrero, V., Romero-Márquez, J. M., García-Pérez, R. N., Novo-Rodríguez, C., Guardia-Baena, J. M., Hayón-Ponce, M., Tenorio-Jiménez, C., López-de-la-Torre-Casares, M., & Muñoz-Garach, A. (2024). Is Fasting Superior to Continuous Caloric Restriction for Weight Loss and Metabolic Outcomes in Obese Adults? A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Nutrients, 16(20), 3533. DOI: 10.3390/nu16203533
- Bitsanis, D., Giannakou, K., Hadjimbei, E., & Chrysostomou, S. (2022). The Effect of Early Time-Restricted Feeding on Glycemic Profile in Adults: A Systematic Review of Interventional Studies. Rev Diabet Stud, 18(1), 10-19. DOI: 10.1900/RDS.2022.18.10
- Xie, Z., Sun, Y., Ye, Y., Hu, D., Zhang, H., He, Z., Zhao, H., Yang, H., & Mao, Y. (2022). Randomized controlled trial for time-restricted eating in healthy volunteers without obesity. Nature Communications, 13(1003). DOI: 10.1038/s41467-022-28662-5
- Tsitsou, S., Zacharodimos, N., Poulia, K. A., Karatzi, K., Dimitriadis, G., & Papakonstantinou, E. (2022). Effects of Time-Restricted Feeding and Ramadan Fasting on Body Weight, Body Composition, Glucose Responses, and Insulin Resistance: A Systematic Review of Randomized Controlled Trials. Nutrients, 14(22), 4778. DOI: 10.3390/nu14224778
- Moro, T., Tinsley, G., Pacelli, F. Q., Marcolin, G., Bianco, A., & Paoli, A. (2021). Twelve Months of Time-restricted Eating and Resistance Training Improves Inflammatory Markers and Cardiometabolic Risk Factors. Medicine & Science in Sports & Exercise, 53(12), 2577-2585. DOI: 10.1249/MSS.0000000000002738
- Patikorn, C., Roubal, K., Veettil, S. K., Chandran, V., Pham, T., Lee, Y. Y., Giovannucci, E. L., Varady, K. A., & Chaiyakunapruk, N. (2021). Intermittent Fasting and Obesity-Related Health Outcomes: An Umbrella Review of Meta-analyses of Randomized Clinical Trials. JAMA Network Open, 4(12), e2139558. DOI: 10.1001/jamanetworkopen.2021.39558




