The human body typically maintains blood glucose levels between 70-100 mg/dL (3.9-5.6 mmol/L)—a remarkably precise balance considering the varying amounts of carbohydrates we consume. When this balance falters and diagnosing diabetes becomes necessary, medical science relies not on one test, but on multiple sophisticated measurements that reveal different aspects of glucose metabolism.
But what exactly happens during these tests? Why might your doctor order an HbA1c test instead of a fasting glucose test? And perhaps most importantly—how close are you to having diabetes without realizing it?
These questions become even more critical when we consider that the early stages of diabetes often produce no symptoms. According to research in the British Medical Journal, beta cell function in the pancreas may decrease by up to 50% before blood glucose levels rise enough to meet diagnostic criteria for diabetes. This means your body could be struggling with insulin resistance or production for years before conventional testing detects a problem.
At IFitCenter, we explore the science of diagnosing diabetes through its full spectrum—from borderline values to definitive diagnosis. Whether you’re concerned about your risk factors, confused by recent test results, or simply want to understand the difference between prediabetes and full diabetes, this guide will provide clarity on the diagnostic methods that reveal your metabolic health status.
Let’s unravel the complexity of diabetes diagnostic criteria together, giving you the knowledge to understand your test results and take proactive steps toward metabolic health.
Diabetes Diagnosis Criteria
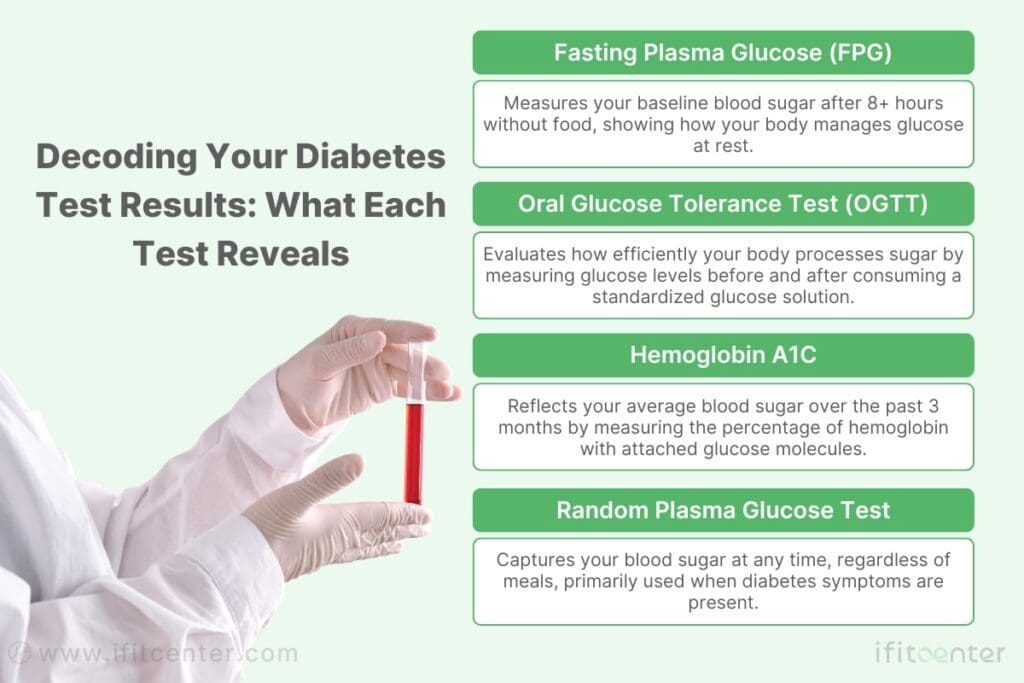
When it comes to diagnosing diabetes, medical professionals rely on several well-established tests that measure how your body processes glucose. Each test offers unique insights, and understanding what they measure can help you make sense of your results. Let’s explore these diagnostic methods in detail.
Fasting Plasma Glucose (FPG) Test
The Fasting Plasma Glucose test is often the first test doctors order when screening for diabetes. As the name suggests, this test measures the amount of glucose (sugar) in your blood after a period of fasting.
Think of it like checking your car’s idle speed. Just as a mechanic measures how your engine runs when it’s not actively working, the FPG test reveals how your body manages glucose when it’s not processing food. This baseline measurement provides valuable information about your body’s natural glucose regulation.
How the Test Is Performed
Preparation for an FPG test is straightforward but important:
- You must fast for at least 8 hours before the test (typically overnight)
- Water is permitted during the fasting period
- Medications should be taken as directed by your healthcare provider
- The test involves a simple blood draw, usually from a vein in your arm
- Results are typically available within a day or two
“Many patients make the mistake of having a small snack or drinking coffee before their fasting glucose test, not realizing even a tiny amount of food or caffeine can significantly affect the results. For the most accurate FPG test, stick to plain water only during your fast, and schedule your test for early morning to minimize the fasting period.”
Dr. Babak Jamalian, Family Physician.
Understanding FPG Results
The FPG test results are measured in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L). Here’s how to interpret your results:
| Result | Classification | What It Means |
|---|---|---|
| Below 100 mg/dL (5.6 mmol/L) | Normal | Your fasting blood glucose is within the normal range |
| 100-125 mg/dL (5.6-6.9 mmol/L) | Prediabetes | Your blood glucose is higher than normal but not high enough to be diagnosed as diabetes |
| 126 mg/dL (7.0 mmol/L) or higher* | Diabetes | These results suggest diabetes |
Advantages and Limitations
Advantages:
- Simple and widely available
- Relatively inexpensive
- Provides a clear baseline measurement
Limitations:
- Requires fasting, which may be difficult for some people
- Provides only a snapshot of glucose levels at one moment in time
- May miss diabetes in some people whose fasting glucose is normal but who have abnormal glucose levels after eating
- Can be affected by recent illness, stress, or medications
The FPG test is most appropriate for routine screening, especially in individuals who don’t have symptoms but may have risk factors for diabetes. It’s also useful for monitoring glucose levels in people already diagnosed with diabetes.
Oral Glucose Tolerance Test (OGTT)
While the FPG test measures your baseline glucose level, the Oral Glucose Tolerance Test (OGTT) evaluates how your body handles a glucose challenge. This test provides a more dynamic picture of your body’s glucose metabolism.
You can think of the OGTT as a stress test for your body’s glucose processing system. Just as a cardiologist might have you exercise on a treadmill to see how your heart responds to exertion, the OGTT challenges your body with a dose of glucose to see how effectively your insulin system responds.
Testing Protocol
The OGTT is more involved than other diabetes tests:
- You’ll need to fast for at least 8 hours before the test
- A healthcare professional will draw your blood to measure your fasting glucose level
- You’ll drink a sweet solution containing 75 grams of glucose (for adults)
- Blood samples are taken at timed intervals, typically at 1 hour and 2 hours after drinking the solution
- Throughout the test, you’ll need to remain seated and cannot eat or drink anything else
Understanding OGTT Results
The most important measurement in the OGTT is your blood glucose level 2 hours after consuming the glucose solution:
| 2-Hour Result | Classification | What It Means |
|---|---|---|
| Below 140 mg/dL (7.8 mmol/L) | Normal | Your body processes glucose normally |
| 140-199 mg/dL (7.8-11.0 mmol/L) | Prediabetes (Impaired Glucose Tolerance) | Your body has difficulty processing glucose efficiently |
| 200 mg/dL (11.1 mmol/L) or higher | Diabetes | These results suggest diabetes |
When OGTT Is Preferred
The OGTT is particularly useful in certain situations:
- When results from other tests are borderline or inconclusive
- For diagnosing gestational diabetes during pregnancy
- When there’s a strong suspicion of diabetes despite normal fasting glucose
- For detecting diabetes at an earlier stage, as postprandial (after-meal) glucose elevations often occur before fasting glucose becomes abnormal
Special Considerations for Pregnancy
Gestational diabetes testing follows a modified protocol:
- Initial screening typically occurs between 24-28 weeks of pregnancy
- A 50-gram glucose challenge may be used first (without fasting)
- If screening results are elevated, a full OGTT with 100 grams of glucose is performed
- Blood glucose is measured fasting and at 1, 2, and 3 hours after glucose consumption
- Diagnostic thresholds are lower during pregnancy due to the increased risks of elevated blood glucose for both mother and baby
On the IFitCenter blog, we have provided a comprehensive guide for diabetes, completely free of charge and based on the latest research. By viewing these articles, in addition to increasing your general knowledge in this field, you can easily manage this disease in a principled manner. To access the first part of the articles, simply use the links below:
- What is Diabetes?
- Symptoms and Signs of Diabetes
- Difference Between Type 1 and Type 2 Diabetes
- What Are the Complications of Diabetes?
- Can Diabetes Be Cured?
- The Connection Between Obesity and Diabetes
Hemoglobin A1C (HbA1C) Test
Unlike tests that measure glucose levels directly, the Hemoglobin A1C test provides insight into your average blood glucose level over the past 2-3 months. This makes it an invaluable tool for both diagnosing diabetes and monitoring long-term glucose control.
Imagine your glucose monitoring as similar to checking the weather. The FPG and OGTT tests are like looking at the temperature right now, while the A1C test is like reviewing the seasonal average. Both provide valuable but different perspectives on the same situation.
What HbA1C Measures
Hemoglobin is the protein in red blood cells that carries oxygen. When glucose circulates in your bloodstream, some of it naturally attaches to hemoglobin, creating glycated hemoglobin (HbA1c). Since red blood cells typically live for about 3 months, measuring the percentage of hemoglobin that has glucose attached provides a view of your average blood glucose level over that period.
How the Test Is Performed
One of the major advantages of the HbA1C test is its simplicity:
- No fasting or special preparation is required
- The test can be performed at any time of day
- It involves a standard blood draw
- Results are typically reported as a percentage
Understanding Hb1AC Results
| A1C Result | Classification | Estimated Average Glucose |
|---|---|---|
| Below 5.7% | Normal | Below 117 mg/dL (6.5 mmol/L) |
| 5.7% to 6.4% | Prediabetes | 117-137 mg/dL (6.5-7.6 mmol/L) |
| 6.5% or higher | Diabetes | 140 mg/dL (7.8 mmol/L) or higher |
Each 1% change in HbA1C corresponds to approximately 29 mg/dL (1.6 mmol/L) change in average blood glucose. For example, an A1C of 8% corresponds to an average blood glucose level of about 183 mg/dL (10.2 mmol/L).
Advantages and Limitations
Advantages:
- No fasting required
- Reflects glucose control over several months, not just a single point in time
- Less affected by daily fluctuations, stress, or illness
- Predicts risk for diabetes complications
Limitations:
- Can be inaccurate in certain conditions affecting red blood cells (anemia, sickle cell disease, recent blood loss or transfusion)
- May be affected by ethnicity (some studies show differences in A1C that aren’t reflected in average glucose levels)
- Not reliable during pregnancy
- Does not provide information about daily glucose fluctuations or hypoglycemia (low blood sugar)
Random Plasma Glucose Test
The Random Plasma Glucose (RPG) test measures blood glucose levels regardless of when you last ate. As the name suggests, this test can be performed at any random time, making it convenient but less precise than other diagnostic methods.
What This Test Measures
The RPG test simply measures the concentration of glucose in your blood at a given moment, regardless of food intake. While other tests control variables like fasting or specific glucose challenges, the RPG provides a snapshot of your glucose level in real-world conditions.
When It’s Used
The Random Plasma Glucose test is typically used in specific circumstances:
- When a person shows classic symptoms of diabetes (excessive thirst, frequent urination, unexplained weight loss)
- In emergency situations where waiting for fasting tests isn’t practical
- As an initial screening tool that may lead to more definitive testing
- For monitoring people with known diabetes
Understanding Your Results
Interpretation of Random Plasma Glucose test results is straightforward:
- A result of 200 mg/dL (11.1 mmol/L) or higher, along with classic symptoms of diabetes, indicates diabetes
- Lower values don’t rule out diabetes and generally require follow-up testing
Follow-up Testing
If your Random Plasma Glucose test suggests diabetes, your healthcare provider will likely request one of the following tests to confirm the diagnosis:
- A repeat Random Plasma Glucose test
- A Fasting Plasma Glucose test
- An Oral Glucose Tolerance Test
- A Hemoglobin A1C test
Confirmation with a second test is standard practice to ensure accurate diagnosis, as temporary factors like stress or illness can sometimes cause transient elevations in blood glucose.
Comparing Standard Tests for Diabetes
Each diabetes diagnostic test has its own strengths and limitations. Understanding how they compare can help you appreciate why your healthcare provider might choose one test over another.
| Test | Preparation Required | Time Required | What It Shows | Best For |
|---|---|---|---|---|
| Fasting Plasma Glucose (FPG) | 8+ hours fasting | Quick (one blood draw) | Baseline glucose level | Initial screening, convenience |
| Oral Glucose Tolerance Test (OGTT) | 8+ hours fasting plus dietary preparation | 2-3 hours | How body responds to glucose challenge | Detecting early diabetes, pregnancy screening |
| Hemoglobin A1C | None | Quick (one blood draw) | Average glucose over 2-3 months | Convenience, long-term monitoring |
| Random Plasma Glucose | None | Quick (one blood draw) | Point-in-time glucose level | Emergency situations, symptomatic patients |
“While A1C testing is convenient because it doesn’t require fasting, it’s not always the best first-line test for everyone. For patients with certain conditions like anemia, recent blood loss, or hemoglobin variants, A1C can give misleading results. In these cases, I often recommend combining a fasting glucose test with a 2-hour post-meal glucose check to get a more accurate picture.”
Dr. Babak Jamalian, Family Physician.
When One Test Is Preferred Over Others
Certain situations may call for specific testing approaches:
- Pregnancy: OGTT is the preferred test for gestational diabetes
- Anemia or blood disorders: FPG or OGTT may be preferred over A1C
- Convenience concerns: A1C requires no fasting or time commitment
- Monitoring established diabetes: A1C is typically used for long-term monitoring
- Suspected daily glucose fluctuations: OGTT may reveal problems not evident on fasting tests
How Doctors Choose Tests
Healthcare providers consider multiple factors when selecting diagnostic tests:
- Patient’s risk factors and symptoms
- Convenience and practicality for the patient
- Reliability of different tests for specific populations
- Cost and insurance coverage
- Need for immediate results versus comprehensive information
The Value of Confirmation
Diabetes is a serious, lifelong condition requiring significant management. For this reason, proper diagnosis typically requires confirmation:
- A single abnormal test result is usually not enough for diagnosis
- Confirmation may involve repeating the same test or using a different test
- Consistent results across different tests provide greater confidence in diagnosis
- Borderline results may warrant closer monitoring or lifestyle interventions even without formal diagnosis
Specialized and Advanced Diagnostic Approaches
While standard tests can diagnose diabetes, healthcare providers often need specialized testing to determine which type of diabetes a person has, which is crucial for proper treatment.
To access the second part of the articles related to diabetes, you can use the following links:
- The Difference Between Prediabetes and Diabetes
- Insulin Resistance and Diabetes
- Understanding Blood Sugar Numbers
- Weight Loss for Type 2 Diabetes
- What is Type 1 Diabetes?
- Best Superfoods for Blood Sugar Control
Distinguishing Between Diabetes Types
Determining whether someone has Type 1 or Type 2 diabetes is essential for effective treatment. The types have different causes, progression patterns, and management requirements.
Why Type Differentiation Matters
- Treatment approach: Type 1 always requires insulin therapy; Type 2 may be managed with lifestyle changes, oral medications, and sometimes insulin
- Management intensity: Type 1 requires more rigorous glucose monitoring
- Addressing root causes: Type 1 involves autoimmunity; Type 2 primarily involves insulin resistance
Diagnostic Tests for Type 1 Diabetes
Autoantibody Testing
- What it measures: Antibodies against beta cell components (GAD65, IAA, ICA, IA-2, IA-2β)
- How performed: Standard blood draw
- Interpretation: Positive results strongly suggest Type 1 diabetes, especially in younger patients
C-peptide Test
- What it measures: Natural insulin production
- Interpretation: Low levels suggest Type 1 diabetes; normal/high levels typically indicate Type 2
Diagnostic Assessments for Type 2 Diabetes
Insulin Resistance Measurements
- HOMA-IR: Calculated using fasting glucose and insulin levels
- Insulin Level Test: Elevated insulin with normal/high glucose suggests insulin resistance
Additional Metabolic Markers
- Lipid Panel: Measures triglycerides and cholesterol
- Liver Function Tests: Fatty liver is common in Type 2 diabetes
- Metabolic indicators: Blood pressure and waist circumference
Special Diagnostic Considerations
Age-Related Considerations
- Children: Type 1 more common but Type 2 increasing
- Adults: Consider late-onset Type 1 or LADA in non-obese individuals
- Elderly: Age-related changes in glucose regulation may affect results
Ethnic Variations
- Asian populations may develop Type 2 at lower BMI thresholds
- A1C values can vary by ethnicity independent of glucose levels
- African descent individuals may have naturally higher A1C levels
Factors Affecting Test Results
- Blood disorders: Anemia, hemoglobinopathies can affect A1C results
- Medications: Corticosteroids, antipsychotics, beta-blockers, diuretics
- Pregnancy: Alters glucose metabolism; requires specific testing protocols
- Other factors: Acute illness, surgery, stress, liver/kidney disease
When to Consider Additional Testing
- Unclear diagnosis after standard testing
- Clinical presentation doesn’t match typical diabetes types
- Family history of unusual diabetes forms
- Poor response to standard treatments
- Early onset without typical risk factors
Emerging Diagnostic Technologies
The field of diabetes diagnosis continues to advance with innovative approaches that may provide earlier and more precise detection. These technologies are changing how we identify and classify diabetes.
Continuous Glucose Monitoring (CGM) in Diagnosis
While typically used for diabetes management, CGM systems are increasingly valuable for diagnostic purposes:
- Provides detailed glucose patterns over multiple days
- Can detect abnormal glucose fluctuations even when standard tests appear normal
- Reveals nocturnal glucose patterns not captured by traditional testing
- May help identify diabetes subtypes based on distinct glucose variation patterns
New Biomarkers Under Investigation
Researchers are exploring additional markers to improve diagnostic accuracy:
- 1,5-anhydroglucitol (1,5-AG): Reflects glucose control over 1-2 weeks
- Glycated albumin: Shows average glucose over 2-3 weeks
- Inflammatory markers: May help identify diabetes risk before glucose abnormalities appear
- MicroRNAs: Small RNA molecules showing promise as early indicators of diabetes
Genetic Testing for Specific Diabetes Types
Genetic analysis is becoming more accessible for identifying less common forms of diabetes:
- Can identify monogenic forms like MODY (Maturity Onset Diabetes of the Young)
- Helps distinguish between diabetes types when clinical features are ambiguous
- May predict risk and guide prevention strategies
- Particularly valuable for diagnosing diabetes in children without typical Type 1 or Type 2 features
Research on Diabetes Subtypes
Recent research suggests Type 2 diabetes may actually comprise several distinct subtypes:
- Severe Insulin-Resistant Diabetes (SIRD)
- Severe Insulin-Deficient Diabetes (SIDD)
- Mild Age-Related Diabetes (MARD)
- Mild Obesity-Related Diabetes (MOD)
These subtypes may have different progression patterns and respond differently to treatments, highlighting the potential for more personalized approaches.
Turn Your Diabetes Diagnosis into Positive Action
Receiving a diabetes diagnosis can feel overwhelming, but with the right approach, you can take control of your metabolic health. At IFitCenter, we believe managing diabetes effectively starts with personalized weight management and a structured lifestyle plan designed specifically around your diagnosis.
Our specialized diabetes management services include:
- Comprehensive Metabolic Evaluations: Understand exactly what’s affecting your blood sugar levels.
- Tailored Weight Loss Programs: Reduce insulin resistance through targeted fat loss.
- Customized Dietary Support: Practical eating strategies tailored to your diagnosis and lifestyle.
- Regular Medical Follow-ups: Continuous monitoring to adjust your treatment as your health improves.
Your diabetes diagnosis doesn’t define your future—your actions do. Let’s build your path to better health together.
Understanding Your Diagnosis
Receiving a diabetes diagnosis can be overwhelming. Understanding what happens next can help you navigate this new health challenge.
What Happens After Diagnosis
- Your healthcare provider will develop a treatment plan based on your specific diabetes type
- You may be referred to a diabetes educator or endocrinologist
- Additional testing may be needed to check for existing complications
- You’ll learn self-management skills including glucose monitoring and medication administration
Key Questions to Ask Your Healthcare Provider
- “What type of diabetes do I have and how certain is this diagnosis?”
- “What are my treatment options and their pros and cons?”
- “How often should I monitor my blood glucose?”
- “What additional tests do I need now and in the future?”
- “What resources are available to help me learn about diabetes management?”
How Diagnostic Values Guide Treatment
Your specific test results inform your treatment approach:
- Higher A1C or glucose values may indicate need for more aggressive treatment
- Presence of autoantibodies suggests Type 1 diabetes requiring insulin therapy
- Evidence of insulin resistance points to lifestyle interventions and possibly medications that improve insulin sensitivity
- Borderline values might warrant a trial of lifestyle modification before medication
Importance of Ongoing Monitoring
Diabetes management requires regular assessment:
- Regular A1C testing (typically every 3-6 months)
- Periodic comprehensive eye, kidney, and foot examinations
- Adjustments to treatment plan based on changing health status
- Monitoring for development of complications or comorbidities
Conclusion
Understanding diabetes diagnostic methods is essential for proper management of this complex condition. The various testing approaches – from standard blood glucose measurements to specialized antibody testing – each provide valuable pieces of information that help healthcare providers make accurate diagnoses and develop effective treatment plans.
Proper diagnosis is the foundation of effective diabetes management. Knowing which type of diabetes you have determines your treatment approach, required monitoring, and long-term outlook. With advances in diagnostic technology and a growing understanding of diabetes subtypes, we’re moving toward increasingly personalized care.
If you have risk factors for diabetes – including family history, excess weight, sedentary lifestyle, or symptoms like increased thirst and urination – don’t hesitate to discuss appropriate testing with your healthcare provider. The earlier diabetes is diagnosed, the sooner you can begin management strategies that help prevent complications and maintain quality of life.
Remember that diabetes diagnosis isn’t a one-time event but the beginning of an ongoing process of monitoring and management. Regular check-ups and testing help ensure your treatment remains effective as your health needs change over time.
To access other content on the IFitCenter’s blog, you can use the following links:
References
- Sacks, D. B., Arnold, M., Bakris, G. L., Bruns, D. E., Horvath, A. R., Lernmark, Å., Metzger, B. E., Nathan, D. M., & Kirkman, M. S. (2023). Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus. Clinical Chemistry, 69(8), 808–868. DOI: 10.1093/clinchem/hvad080
- Kaur, G., Lakshmi, P. V. M., Rastogi, A., Bhansali, A., Jain, S., Teerawattananon, Y., Bano, H., & Prinja, S. (2020). Diagnostic accuracy of tests for type 2 diabetes and prediabetes: A systematic review and meta-analysis. PLOS ONE, November 20, 2020. DOI: 10.1371/journal.pone.0242415
- American Diabetes Association (2024). The American Diabetes Association Releases Standards of Care in Diabetes—2025. December 9, 2024. Arlington, VA.



