When was the last time you thought about your liver health? If you’re like most people, probably not recently. Yet here’s a question that might change that: Did you know your liver could be storing dangerous amounts of fat even if you feel perfectly healthy? Or that traditional liver function tests might miss early signs of fatty liver disease entirely?
Consider this: What if the standard blood test your doctor ordered isn’t telling the whole story? What if those “normal” test results are giving you a false sense of security? These aren’t hypothetical questions – they’re real concerns that medical professionals at IFitCenter and worldwide grapple with daily.
The challenge lies not just in getting tested, but in understanding what these tests really mean. With multiple testing methods available – from basic blood work to advanced imaging – how do you know which tests matter? What numbers should you pay attention to? And most importantly, what do these results mean for your health?
Whether you’re concerned about your liver health, have been advised to get tested, or simply want to be proactive about your well-being, understanding fatty liver tests is crucial. Let’s explore the complete picture of liver testing, breaking down complex medical concepts into clear, actionable information.
Understanding Fatty Liver Grades and Symptoms
Imagine your liver as a vital filter for your body. When this filter starts accumulating fat, it gradually becomes less efficient – much like a clogged water filter. But exactly how much fat accumulation is concerning, and what signs should you watch for? Let’s break down the stages of fatty liver disease in clear, practical terms.
What makes fatty liver disease particularly challenging is its silent progression in early stages. In my years of clinical experience, I’ve observed that patients with normal liver enzymes can still have significant fat accumulation. This is why understanding the different grades of fatty liver disease is crucial – it helps us identify and address issues before they progress to more serious stages.
Dr. Babak Jamalian, Family Physician Specialist.
The Four Grades of Fatty Liver: What Do They Mean?
Medical science classifies fatty liver into four distinct grades, each representing different levels of fat accumulation in liver cells:
- Grade 0 (Normal): Your liver is healthy with minimal fat (less than 5%)
- Grade 1 (Mild): Fat affects 5-33% of your liver cells – often reversible with lifestyle changes
- Grade 2 (Moderate): 33-66% of liver cells contain fat – requires medical attention
- Grade 3 (Severe): Over 66% fat accumulation – needs immediate medical intervention
“Recent studies show that early detection and intervention in Grade 1 fatty liver can prevent progression to more severe stages in over 90% of cases.”
Hepatology Journal, 2023
Key Symptoms at Each Grade
Fatty liver is often called a “silent disease” because symptoms may not be obvious, especially in early stages. However, each grade may present different signals:
- Grade 1 Symptoms:
- Often no visible symptoms
- Mild fatigue
- Slight discomfort in upper right abdomen
- Grade 2 Symptoms:
- Increased fatigue
- Persistent abdominal discomfort
- Unexplained weight changes
- Grade 3 Symptoms:
- Noticeable fatigue
- Visible yellowing of skin or eyes
- Swelling in legs or abdomen
- Dark urine color
Warning Signs That Shouldn’t Be Ignored
While some symptoms might seem minor, certain signs warrant immediate medical attention:
- Persistent fatigue that doesn’t improve with rest
- Pain or discomfort in the upper right side of your abdomen
- Unexplained weight loss
- Any yellowing of skin or eyes
- Swelling in your legs or abdomen
Risk Factors to Consider
Understanding your risk factors is crucial for early detection. Key risk factors include:
- Being overweight or obese
- Type 2 diabetes or prediabetes
- High cholesterol or triglycerides
- Rapid weight changes
- Poor dietary habits
- Sedentary lifestyle
When to Seek Medical Help
Don’t wait for severe symptoms to appear. Consider getting tested if you:
- Have two or more risk factors mentioned above
- Experience persistent unexplained fatigue
- Notice any of the warning signs listed
- Have a family history of liver disease
Early detection through proper testing remains your best defense against fatty liver progression. Understanding these grades and symptoms empowers you to take control of your liver health before serious complications develop.
To access other scientific articles on the blog, you can use the following links:
- Is Coffee Good for Fatty Liver?
- Is Dark Chocolate Good for Fatty Liver?
- What is Fatty Liver Disease?
- Best and Worst Drinks for Fatty Liver
- What is Prediabetes?
- Best Diet for Fatty Liver
- insulin resistance weight gain
- Understanding Metabolic Syndrome
- cooking oil name list
Essential Blood Tests for Fatty Liver
When it comes to detecting fatty liver disease, blood tests serve as your first line of investigation. Think of these tests as a detailed health report card for your liver, revealing important information about how well it’s functioning and whether there might be any underlying issues.
Key Blood Tests for Liver Health
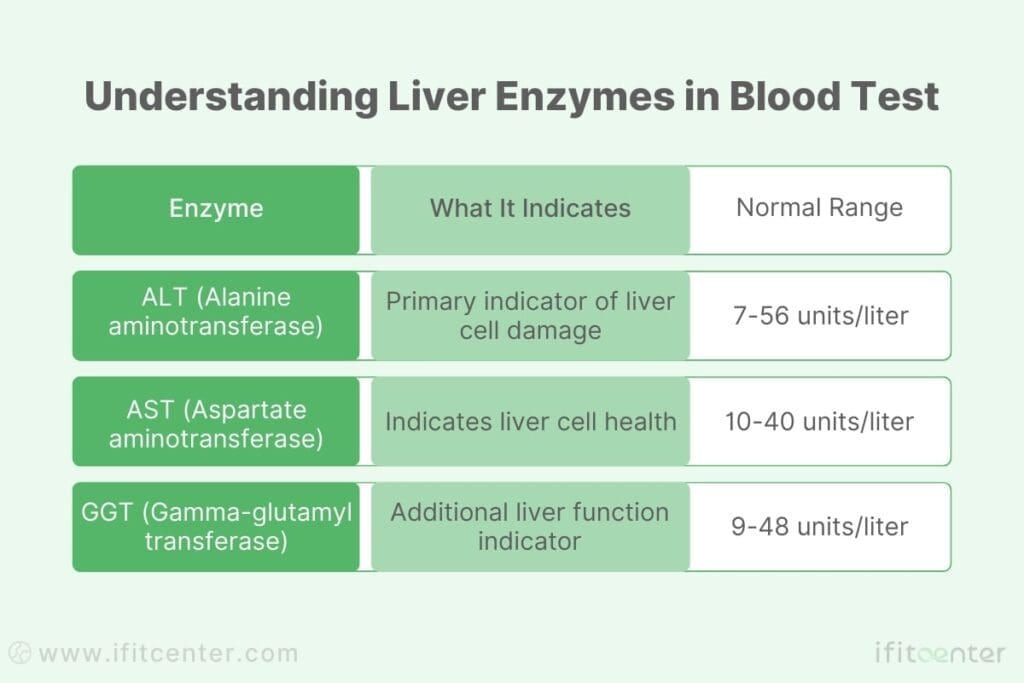
Several specific blood markers help doctors evaluate liver health. Let’s explore what each of these important tests means:
- ALT (Alanine Aminotransferase): This enzyme typically lives inside liver cells. When found in your blood, it may indicate liver cell damage
- Normal range: 7-56 units/liter
- Elevated levels might suggest liver inflammation
- AST (Aspartate Aminotransferase): Another enzyme that can signal liver stress
- Normal range: 10-40 units/liter
- Often evaluated alongside ALT
- GGT (Gamma-Glutamyl Transferase): An enzyme that can indicate bile duct issues
- Normal range: 9-48 units/liter
- Can be elevated in early stages of fatty liver
Understanding Fatty Liver Blood Test Results
Blood test results aren’t always straightforward. Here’s what different patterns might indicate:
- Mild Elevation: ALT or AST between 1-3 times normal range
- May suggest early-stage fatty liver
- Often reversible with lifestyle changes
- Moderate Elevation: 3-5 times normal range
- Could indicate active liver inflammation
- Requires medical evaluation
- Significant Elevation: More than 5 times normal range
- Suggests serious liver issues
- Needs immediate medical attention
“Recent research shows that liver enzymes can be normal in up to 80% of people with fatty liver disease, highlighting why comprehensive testing is crucial for accurate diagnosis.”Journal of Hepatology, 2023
Beyond Basic Liver Tests
A complete fatty liver assessment often includes additional blood tests:
- Lipid Profile: Measures cholesterol and triglycerides
- Blood Sugar Tests: Checks for diabetes risk
- Albumin Levels: Indicates liver’s protein production capability
- Platelet Count: Can signal advanced liver disease
When Should You Get Tested?
Consider liver function testing if you:
- Are overweight or obese
- Have type 2 diabetes
- Experience unexplained fatigue
- Have a family history of liver disease
- Notice changes in your digestion or energy levels
Remember: Normal blood test results don’t always rule out fatty liver disease. They’re just one piece of the diagnostic puzzle, often needing to be combined with other tests for a complete picture of your liver health.
A Medically Supervised Approach to Fatty Liver Management
Understanding your liver test results is just the beginning. Managing fatty liver effectively requires a comprehensive approach that goes beyond standard testing. At IFitCenter, under the medical supervision of Dr. Babak Jamalian, we provide a scientifically-backed weight management program designed to reduce liver fat, improve metabolic health, and prevent complications.
Our structured three-phase program focuses on:
✅ Medically guided weight loss to reduce liver fat accumulation
✅ Nutritional and lifestyle coaching tailored to your specific needs
✅ Regular monitoring of liver function and metabolic markers
Don’t wait for fatty liver to progress—take control of your liver health today.
Advanced Diagnostic Methods
While blood tests provide important clues about liver health, advanced diagnostic methods offer a more detailed view of what’s happening inside your liver. These techniques help doctors not only confirm the presence of fatty liver but also determine its severity and monitor treatment progress.
The effectiveness of fatty liver diagnosis lies in our ability to combine multiple diagnostic approaches. While ultrasound can detect moderate to severe fatty liver, early stages often require a more comprehensive assessment. By integrating various testing methods – from blood work to advanced imaging – we can create a more accurate picture of liver health and intervene at the most effective time.
Dr. Babak Jamalian, Family Physician Specialist.
Imaging Technologies: Seeing Inside Your Liver
Ultrasound Examination and Fatty Liver Test Name
Ultrasound is typically the first imaging test used to check for fatty liver. Think of it as taking a detailed picture of your liver using sound waves. During this painless examination:
- A special gel is applied to your abdomen
- Sound waves create real-time images of your liver
- Different textures indicate varying levels of fat accumulation
- Results are immediately available for discussion
FibroScan Technology
FibroScan represents the next generation of liver assessment. This specialized ultrasound:
- Measures liver stiffness to assess fibrosis
- Provides a controlled attenuation parameter (CAP) score for fat measurement
- Takes just 5-10 minutes to complete
- Offers immediate, quantifiable results
Advanced Imaging Options
In some cases, additional imaging may be recommended:
- CT Scans: Provide detailed cross-sectional images of your liver
- MRI: Offers the most detailed view of liver tissue and fat content
- MRI-PDFF: Most accurate method for measuring liver fat percentage
“Magnetic resonance imaging techniques can detect as little as 3% liver fat content, making them the most sensitive tools for early detection.”Journal of Hepatology, 2023
Specialized Non-Invasive Tests
Modern medicine has developed several scoring systems that combine different test results to assess liver health:
- Fatty Liver Index (FLI):
- Combines BMI, waist circumference, triglycerides, and other markers
- Scores range from 0-100
- Highly accurate for predicting fatty liver
- NAFLD Fibrosis Score:
- Assesses risk of advanced fibrosis
- Uses age, blood tests, and other factors
- Helps determine need for further testing
When Is Liver Biopsy Necessary?
While non-invasive tests are usually sufficient, a liver biopsy might be recommended when:
- Other test results are inconclusive
- There’s suspicion of other liver conditions
- Advanced liver disease needs to be assessed
- Treatment decisions require precise staging
Emerging Diagnostic Technologies
The field of liver diagnostics continues to evolve with promising new technologies:
- Advanced blood biomarkers for early detection
- Artificial intelligence analysis of imaging results
- New non-invasive measurement techniques
- Improved scoring systems for better accuracy
Interpreting Your Test Results
Making sense of your fatty liver test results can feel like decoding a complex puzzle. Let’s break down what these numbers and reports really mean for your health, and what patterns might indicate the need for closer attention.
Reading Your Blood Test Report
Your blood test report typically includes several key sections that tell different parts of your liver health story:
- Reference Range: The normal range for each marker
- Your Result: Your specific test value
- Units: How the result is measured (often in U/L or mg/dL)
- Flag: Indicators like H (High) or L (Low) when results are outside normal ranges
Key Patterns to Understand
Different combinations of test results can tell different stories about your liver health:
- Pattern 1: Elevated ALT with Normal AST
- Often seen in early fatty liver
- Usually reversible with lifestyle changes
- Pattern 2: Both ALT and AST Elevated
- May indicate more advanced liver issues
- Requires medical evaluation
- Pattern 3: Normal Enzymes but High Imaging Scores
- Can still indicate fatty liver
- Shows why multiple tests are important
Understanding Imaging Reports
Imaging reports use specific terms to describe liver appearance and condition:
- Echogenicity: How bright your liver appears on ultrasound
- Normal: Similar to kidney brightness
- Increased: Brighter than kidney, suggesting fat
- Texture: The pattern of liver tissue
- Homogeneous: Even texture throughout
- Heterogeneous: Uneven texture needing investigation
- Size: Liver measurements
- Normal: Usually less than 15.5 cm
- Enlarged: May indicate inflammation
Red Flags in Test Results
Watch for these warning signs that may require immediate medical attention:
- Liver enzymes more than 3 times the upper limit of normal
- Rapid changes in test results over short periods
- Significant size increase noted on imaging
- New texture changes in follow-up scans
“Understanding your test results is crucial for taking control of your liver health. Regular monitoring and proper interpretation can help catch problems early when they’re most treatable.”Journal of Hepatology, 2023
Taking Action Based on Results
Different result patterns may require different responses:
- Mild Changes: Lifestyle modifications often help
- Moderate Changes: May need medical intervention
- Significant Changes: Require immediate medical attention
Want to better understand your fatty liver test results? Download our comprehensive guide to test interpretation. This free resource helps you make sense of your numbers and know when to seek medical attention.
Building Your Care Plan
Once you understand your fatty liver test results, the next crucial step is developing a comprehensive care plan. Think of this plan as your roadmap to liver health – it needs to be both practical and sustainable for your lifestyle.
Follow-Up Testing Schedule
Your testing frequency should align with your risk level and current test results:
- Early Stage (Grade 1):
- Liver function tests every 6 months
- Annual ultrasound examination
- Regular body composition analysis
- Moderate Stage (Grade 2):
- Liver function tests every 3-4 months
- Ultrasound every 6 months
- Consider FibroScan annually
- Advanced Stage (Grade 3):
- Monthly liver function monitoring
- Quarterly imaging assessments
- Regular specialist consultations
“Regular monitoring through appropriate testing is crucial for tracking improvement and catching any potential complications early.”
Annals of Hepatology, 2023
Lifestyle Modifications Based on Test Results
Different test results may require different lifestyle approaches:
- For Elevated Liver Enzymes:
- Reduce processed food intake
- Increase fiber consumption
- Monitor portion sizes
- Regular moderate exercise
- For High Fat Content on Imaging:
- Focus on lean proteins
- Limit saturated fats
- Include liver-supporting foods
- Structured physical activity plan
- For Multiple Abnormal Markers:
- Comprehensive dietary review
- Supervised exercise program
- Stress management techniques
- Regular sleep schedule
Long-Term Management Strategy
Successful long-term management involves several key components:
- Regular Monitoring:
- Keep track of all test results
- Document lifestyle changes
- Note any new symptoms
- Health Markers to Track:
- Body weight and composition
- Blood pressure readings
- Blood sugar levels
- Energy and fatigue levels
- Lifestyle Consistency:
- Maintain dietary improvements
- Regular exercise routine
- Stress management practices
Adjusting Your Plan
Your care plan should be flexible and adjust based on:
- Changes in test results
- Response to lifestyle modifications
- New health developments
- Personal circumstances and challenges
Prevention Through Early Detection
When it comes to fatty liver disease, prevention and early detection can make a dramatic difference in health outcomes. Research shows that early intervention can prevent up to 90% of fatty liver cases from progressing to more serious stages.
Why Regular Screening Matters
Regular screening serves as your early warning system for liver health issues. Consider these key benefits:
- Early Intervention:
- Detect changes before symptoms appear
- Prevent progression to serious stages
- More treatment options available
- Better Outcomes:
- Higher success rates with early treatment
- Lower risk of complications
- More effective lifestyle interventions
- Cost-Effective:
- Prevents expensive treatments later
- Reduces need for advanced care
- Minimizes health complications
Risk-Based Testing Schedules
Your optimal testing schedule depends on your risk factors and current health status:
- Low Risk:
- Annual liver function tests
- Regular physical examinations
- Basic health screenings
- Moderate Risk:
- Bi-annual liver function tests
- Annual imaging studies
- Regular metabolic screening
- High Risk:
- Quarterly liver function tests
- Regular specialized imaging
- Comprehensive health monitoring
“The most effective strategy against fatty liver disease is catching it early through regular screening and monitoring.”
Hepatology Research, 2023
Self-Monitoring Guidelines
Between professional screenings, you can monitor several important indicators:
- Physical Signs:
- Changes in energy levels
- Digestive changes
- Weight fluctuations
- Lifestyle Factors:
- Diet quality tracking
- Exercise consistency
- Sleep patterns
- Risk Behaviors:
- Alcohol consumption
- Medication use
- Stress levels
Latest Prevention Research
Recent studies have revealed new insights into fatty liver prevention:
- Dietary Factors:
- Impact of meal timing on liver health
- Role of specific nutrients
- Benefits of Mediterranean diet patterns
- Lifestyle Interventions:
- Optimal exercise types and timing
- Sleep quality importance
- Stress management benefits
- Risk Reduction:
- New preventive strategies
- Early intervention methods
- Lifestyle modification effectiveness
Action Steps for Prevention
Take these proactive steps to protect your liver health:
- Schedule regular check-ups
- Maintain a testing calendar
- Track health indicators
- Keep detailed health records
- Stay informed about liver health
Key Takeaways About Fatty Liver Testing
Understanding and monitoring your liver health doesn’t have to be overwhelming. Throughout this guide, we’ve explored the essential aspects of fatty liver testing and diagnosis, from basic blood work to advanced imaging techniques.
Important Points to Remember
- Multiple Testing Methods Matter:
- Blood tests provide initial insights
- Imaging offers detailed liver assessment
- Combined approaches give the most accurate picture
- Early Detection is Critical:
- Regular screening can prevent disease progression
- Normal blood tests don’t always rule out fatty liver
- Understanding your risk factors guides testing frequency
- Test Results Tell a Story:
- Pattern recognition helps understand progression
- Changes over time matter more than single results
- Context matters when interpreting numbers
Your Next Steps
Take these practical steps to maintain your liver health:
- Schedule Regular Testing:
- Annual liver function tests if low risk
- More frequent monitoring if high risk
- Regular imaging based on risk factors
- Track Your Results:
- Keep copies of all test results
- Monitor trends over time
- Note any significant changes
- Stay Informed:
- Learn about new testing methods
- Understand your risk factors
- Keep up with prevention strategies
The Future of Fatty Liver Testing
Exciting developments are on the horizon for liver health assessment:
- New Technologies:
- Advanced imaging techniques
- More accurate biomarkers
- Non-invasive testing methods
- Improved Diagnostics:
- Earlier detection capabilities
- More precise staging methods
- Better prediction models
- Personalized Approaches:
- Risk-based testing protocols
- Individualized monitoring plans
- Targeted intervention strategies
“The future of fatty liver testing lies in combining multiple diagnostic approaches to create a more complete and accurate picture of liver health, enabling earlier intervention and better outcomes.”
Journal of Hepatology, 2023
Remember, your liver’s health is largely in your control. Regular testing, proper interpretation of results, and timely action based on findings can help ensure your liver stays healthy for years to come. Stay informed, stay proactive, and don’t hesitate to seek professional guidance when needed.
To access other content on the IFitCenter’s blog, you can use the following links:
References
- Dyson JK, Anstee QM, McPherson S. Non-alcoholic fatty liver disease: a practical approach to diagnosis and staging. Frontline Gastroenterol. 2014;5(3):211-218. DOI: 10.1136/flgastro-2013-100403
Used for diagnostic criteria and staging guidelines - Contreras D, González-Rocha A, Clark P, Barquera S, Denova-Gutiérrez E. Diagnostic accuracy of blood biomarkers and non-invasive scores for the diagnosis of NAFLD and NASH: Systematic review and meta-analysis. Annals of Hepatology. 2023;28:100873. DOI: 10.1016/j.aohep.2022.100873
Used for blood biomarker accuracy data and test interpretation guidelines - Rinella ME, Neuschwander-Tetri BA, Siddiqui MS, et al. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology. 2023;77:1797-1835. DOI: 10.1002/hep.32723
Used for current clinical practice guidelines and diagnostic recommendations - Vali Y, Lee J, Boursier J, et al. Enhanced liver fibrosis test for the non-invasive diagnosis of fibrosis in patients with NAFLD: A systematic review and meta-analysis. J Hepatol. 2020;73(2):252-262. DOI: 10.1016/j.jhep.2020.03.036
- Boursier J, Vergniol J, Guillet A, et al. Diagnostic accuracy and prognostic significance of blood fibrosis tests and liver stiffness measurement by FibroScan in non-alcoholic fatty liver disease. J Hepatol. 2016;65(3):570-578. DOI: 10.1016/j.jhep.2016.04.023



