Here’s a startling fact: 25% of people worldwide have fatty liver disease – that’s one in four people walking past you on the street. Even more alarming? This number has doubled in the past decade, with experts projecting it will affect half the global population by 2030.
But here’s the silver lining from recent research: A modest 5-7% reduction in body weight can significantly improve liver health in most cases. Scientists at the International Liver Congress 2023 revealed that sustainable weight loss could reverse fatty liver disease in up to 90% of early-stage cases.
At IFitCenter, these statistics aren’t just numbers – they represent real people seeking answers about the connection between their weight and liver health. The science is clear: understanding this relationship could be the key to preventing one of the most common yet underrecognized health threats of our time.
Understanding Fatty Liver Disease
Imagine your liver as your body’s processing plant. Just like a well-run factory, it filters toxins, processes nutrients, and helps manage your body’s energy storage. When fat starts accumulating in liver cells – much like boxes piling up in a warehouse – we call this condition fatty liver disease.
Recent research shows that when fat makes up more than 5% of your liver’s weight, it’s considered fatty liver disease. Think of it this way: if your liver were a 100-piece puzzle, having more than 5 pieces covered in fat would signal a problem.
Two Main Types of Fatty Liver
Fatty liver disease comes in two distinct forms:
- Alcoholic Fatty Liver Disease: Caused by excessive alcohol consumption, where the liver becomes overwhelmed trying to process large amounts of alcohol.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Develops in people who drink little to no alcohol, often linked to lifestyle and metabolic factors.
On the IFitCenter blog, we have published a free content database about fatty liver disease that can have a significant impact for you in controlling and preventing this disease. For access, simply use the links below:
- what is a fatty liver and what causes it
- causes of fatty liver
- fatty liver signs
- fatty liver disease diagnosis
- does 12hour fasting help fatty liver
- types of fatty liver disease
Risk Factors Beyond Weight
While weight plays a significant role, several other factors can increase your risk of developing fatty liver disease:
- High blood sugar levels or type 2 diabetes
- Elevated cholesterol or triglycerides
- Metabolic syndrome
- Rapid weight loss through extreme dieting
- Certain medications
- Genetic factors
“Non-alcoholic fatty liver disease is now recognized as the most common form of chronic liver disease in Western countries, affecting up to 25% of the general population.”
Journal of Hepatology, 2023
The Silent Nature of Fatty Liver
Fatty liver disease is often called a “silent condition” because it typically develops without obvious symptoms. This silence is precisely what makes it concerning – many people don’t realize they have it until the condition has progressed significantly.
Early Warning Signs to Watch For
While fatty liver disease might not cause obvious symptoms initially, some subtle signs may indicate its presence:
- Unexplained fatigue or weakness
- Discomfort in the upper right side of the abdomen
- Loss of appetite
- Nausea or queasiness
- Yellowing of the skin or eyes (in advanced cases)
“Early recognition of fatty liver disease is crucial as lifestyle interventions can prevent progression to more serious liver conditions.”
The Lancet Gastroenterology & Hepatology, 2024
Why Does Fatty Liver Go Undetected?
Several factors contribute to fatty liver disease remaining undetected:
- Symptoms are often subtle or nonexistent in early stages
- Many people dismiss mild symptoms as everyday fatigue or stress
- Regular check-ups don’t always include liver function tests
- The condition can develop even in people who appear healthy
Common Misconceptions That Delay Detection
Understanding these common misconceptions can help you stay vigilant about your liver health:
| Misconception | Reality |
| “Only overweight people get fatty liver” | Even people with normal weight can develop fatty liver disease |
| “You need to drink alcohol to have liver problems” | Non-alcoholic fatty liver disease is increasingly common |
| “No symptoms means no problems” | Fatty liver often develops silently without early symptoms |
| “It’s not serious if I feel fine” | Without intervention, fatty liver can progress to serious liver damage |
Understanding these warning signs and misconceptions is crucial because early detection can make a significant difference in treatment outcomes. Regular health check-ups that include liver function tests are especially important if you have risk factors for fatty liver disease.
Diagnosis Methods: From Blood Tests to Imaging
Diagnosing fatty liver disease typically requires a combination of different tests, as no single test can tell the complete story. Understanding these tests can help you better engage with your healthcare journey.
Blood Tests: Understanding Liver Enzymes
Your liver’s health is often first evaluated through blood tests that measure specific enzymes:
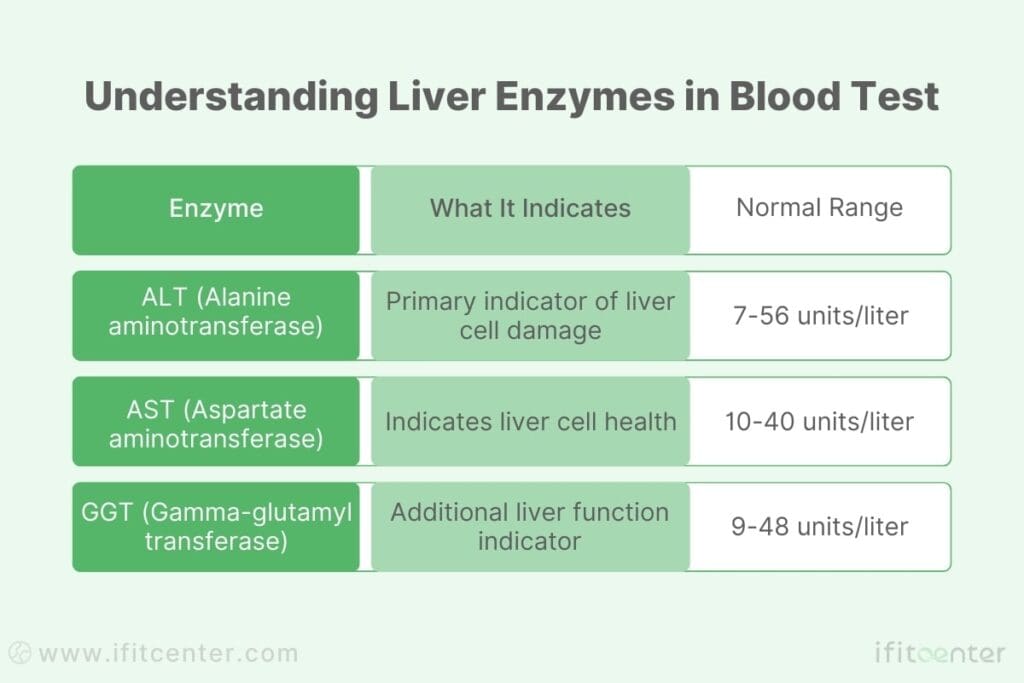
However, it’s important to note that normal liver enzyme levels don’t rule out fatty liver disease – up to 80% of people with fatty liver disease show normal enzyme levels in early stages.
Ultrasound Imaging: Seeing Inside Your Liver
Ultrasound is the most common imaging method used to diagnose fatty liver disease. During this painless procedure, sound waves create pictures of your liver, allowing doctors to:
- Observe the size and shape of your liver
- Detect increased echogenicity (brightness) indicating fat accumulation
- Compare liver tissue density with other organs
- Assess the texture of liver tissue
Understanding the Grading System
Fatty liver disease is typically graded into three levels based on ultrasound findings:
- Grade 1 (Mild): Slight increase in liver echogenicity with normal visualization of blood vessels
- Grade 2 (Moderate): Increased liver echogenicity with slightly impaired visualization of blood vessels
- Grade 3 (Severe): Marked increase in echogenicity with poor or no visualization of blood vessels
Why Multiple Tests Are Needed
Different tests provide different pieces of the diagnostic puzzle:
- Blood tests show liver function and inflammation
- Imaging reveals physical changes in the liver
- Medical history helps identify risk factors
- Physical examination can reveal additional symptoms
“A comprehensive approach to diagnosis, combining various testing methods, provides the most accurate assessment of fatty liver disease and helps guide treatment decisions.”
Journal of Hepatology, 2024
Grades of Fatty Liver Disease
Understanding the different grades of fatty liver disease helps you recognize the seriousness of your condition and the importance of taking action. Like many health conditions, fatty liver disease progresses through distinct stages, each with its own implications for your health.
Understanding the Stages
| Grade | Characteristics | Health Implications |
| Grade 1 (Mild) | Small amounts of fat in liver cells, minimal inflammation | Usually reversible with lifestyle changes |
| Grade 2 (Moderate) | Increased fat accumulation, some inflammation present | Requires more focused intervention |
| Grade 3 (Severe) | Significant fat accumulation, inflammation, possible scarring | Risk of permanent liver damage |
Impact on Your Health
Each grade of fatty liver disease affects your health differently:
- Grade 1: Often discovered during routine tests
- Minimal impact on daily life
- Excellent chance of reversal
- May not show obvious symptoms
- Grade 2: More noticeable effects
- Increased liver enzyme levels
- Possible fatigue and discomfort
- Higher risk of metabolic issues
- Grade 3: Significant health concerns
- Risk of permanent liver damage
- Increased chance of complications
- May require medical intervention
How Progression Occurs
Fatty liver disease typically progresses through several phases:
- Initial Fat Accumulation: Fat begins to build up in liver cells
- Inflammatory Response: The body reacts to fat accumulation with inflammation
- Cellular Changes: Continued stress leads to liver cell damage
- Potential Scarring: In advanced cases, scar tissue may develop
“Early intervention in fatty liver disease can prevent progression to more severe stages. Research shows that improvements in lifestyle factors can reverse the condition, particularly in early grades.”
American Journal of Gastroenterology, 2023
It’s important to understand that progression isn’t inevitable. With proper intervention, especially in early stages, fatty liver disease can be halted or even reversed. The key is recognizing your grade and taking appropriate action.
The Weight Connection: Scientific Evidence
The relationship between body weight and liver health is more complex than simply “being overweight causes fatty liver.” Recent scientific research has revealed fascinating insights into how weight affects our liver function and overall health.
“What many people don’t realize is that the relationship between weight and fatty liver is bidirectional. While excess weight can contribute to fatty liver development, the liver’s condition also influences how effectively the body manages weight. This is why any approach to addressing fatty liver through weight management must consider both factors simultaneously.”
Dr. Babak Jamalian, Family Physician.
How Weight Impacts Your Liver
Scientific research published in the Journal of Hepatology reveals three key ways excess weight affects liver health:
- Fat Storage Overflow: When fat cells in other parts of your body become full, excess fat begins accumulating in the liver
- Inflammatory Response: Excess weight triggers inflammation throughout the body, including the liver
- Metabolic Stress: Extra weight affects how your body processes and stores energy
The Numbers Tell the Story
Recent studies have uncovered striking statistics about the weight-liver connection:
| Weight Change | Impact on Liver Health |
| 5-7% weight loss | Can reduce liver fat by 30-40% |
| 10% weight loss | May reverse fatty liver in early stages |
| Every 1 kg/m² BMI increase | Raises fatty liver risk by 13% |
“Even a modest weight reduction of 5% can significantly improve liver health, particularly in the early stages of fatty liver disease.”
Lancet Gastroenterology & Hepatology, 2024
Understanding the Metabolic Connection
The relationship between weight and liver health involves several metabolic factors:
- Insulin Resistance: Excess weight can make cells less responsive to insulin, forcing the liver to store more fat
- Oxidative Stress: Higher body weight increases oxidative stress, potentially damaging liver cells
- Hormonal Changes: Body fat produces hormones that can affect liver function
Interestingly, research shows that not all body fat affects the liver equally. Abdominal fat, particularly visceral fat around organs, has a stronger connection to fatty liver disease than fat in other areas of the body.
The Normal Weight Paradox
Recent studies have revealed an important finding: while excess weight increases fatty liver risk, approximately 7-20% of people with normal body weight can develop fatty liver disease. This highlights the importance of considering multiple health factors beyond just weight.
To access the second part of the fatty liver content, I invite you to use the links below:
- foods good for fatty liver
- is omega 3 good for liver disease?
- fatty liver and eggs
- is dark chocolate good for fatty liver?
- fatty liver blood test results
- treating fatty liver disease with diet
- best vitamins for fatty liver
Weight Loss as a Natural Treatment Approach
Scientific research consistently shows that weight loss can be one of the most effective natural treatments for fatty liver disease. Understanding how much weight loss is needed and how to achieve it safely can make a significant difference in your liver health.
Evidence-Based Benefits of Weight Loss
Recent clinical studies have revealed impressive results about how weight loss affects fatty liver disease:
| Weight Loss Amount | Liver Health Improvement |
| 3-5% body weight | Reduction in liver fat |
| 5-7% body weight | Significant improvement in liver inflammation |
| 7-10% body weight | Potential reversal of liver damage |
How Much Weight Loss Is Needed?
The amount of weight loss needed varies depending on your starting point and the severity of fatty liver disease:
- For mild fatty liver: Even a modest weight loss of 3-5% can show improvements
- For moderate cases: Aim for 5-7% weight reduction
- For severe cases: A 7-10% weight loss may be necessary
“Weight loss achieved through lifestyle modification significantly improves liver histology in non-alcoholic fatty liver disease.”
Gastroenterology, 2023
Timeline for Seeing Results
Understanding realistic timelines helps set appropriate expectations:
- First 4-8 weeks: Initial improvements in liver enzymes may be seen
- 3-6 months: Noticeable reduction in liver fat content
- 6-12 months: Significant improvements in liver health markers
Key Success Factors
Research has identified several factors that contribute to successful weight loss for liver health:
- Gradual, sustainable weight loss (1-2 pounds per week)
- Regular monitoring of progress
- Personalized approach based on individual health status
- Professional guidance for safe and effective results
While weight loss can be effective, it’s important to approach it correctly. Rapid weight loss through extreme dieting can actually worsen liver health. For the best results, consider consulting with healthcare professionals who can create a personalized plan that takes into account your specific situation and health goals.
Understanding Weight Loss Medication Risks
While the desire for quick weight loss results is understandable, certain approaches can potentially worsen your liver health. Understanding these risks is crucial for making informed decisions about your weight loss journey.
The Hidden Dangers of Quick Fixes
Research has identified several ways that unsupervised weight loss methods can impact your health:
- Rapid Weight Loss: Losing weight too quickly can increase liver stress
- Nutritional Imbalances: Extreme dieting often lacks essential nutrients your liver needs
- Metabolic Disruption: Some methods can disturb your body’s natural metabolic processes
“Rapid weight loss of more than 1.6kg per week may actually increase the risk of liver complications, especially in people with existing fatty liver disease.”
Journal of Hepatology, 2023
Impact on Liver Health
Unmonitored weight loss medications can affect your liver in several ways:
| Risk Factor | Potential Impact |
| Drug-induced stress | Additional burden on an already compromised liver |
| Harmful interactions | Complications with existing medications or conditions |
| Metabolic changes | Disruption of liver’s natural fat-processing ability |
Warning Signs to Watch For
Be aware of these potential red flags when using weight loss products:
- Unexplained fatigue or weakness
- Increased liver enzyme levels
- Digestive discomfort or nausea
- Unusual changes in appetite
- Rapid, unexplained weight loss
The Importance of Medical Supervision
Professional medical supervision during weight loss is crucial because it provides:
- Regular monitoring of liver function
- Personalized approach based on your health status
- Early detection of potential complications
- Safe, sustainable weight loss strategies
- Proper dosage and timing adjustments when needed
Remember that sustainable weight loss takes time, and there are no safe shortcuts when it comes to your liver health. Any weight loss approach should be discussed with healthcare professionals who understand your complete medical history and can monitor your progress safely.
Reverse Fatty Liver Safely with the IFitCenter Medically Supervised Diet
Fatty liver disease is no longer an untreatable condition. Scientific research proves that losing just 5-7% of your body weight can significantly improve liver function and, in many cases, even reverse fatty liver disease. However, not all weight loss approaches are safe or effective—rapid weight loss and extreme diets can actually worsen liver health.
At IFitCenter, we offer a medically supervised, science-based weight loss program designed to:
✔ Help you lose weight safely and effectively without harming your liver
✔ Reduce liver fat and inflammation through balanced, nutrient-rich meals
✔ Monitor your liver health throughout your weight loss journey to ensure lasting results
If you’ve been diagnosed with fatty liver or are at risk, take action now. Start your weight loss journey with a structured plan designed for liver health.
Safe Approaches to Weight Management
Research shows that sustainable weight loss is most effective for improving liver health. Understanding evidence-based approaches can help you make informed decisions about your weight management journey.
“In my three decades of clinical experience, I’ve observed that the most successful weight management approaches for improving liver health are those that focus on gradual, sustainable changes. A reduction of even 5% in body weight, when achieved steadily over time, often shows more significant improvements in liver health markers than rapid weight loss.”
Dr. Babak Jamalian, Family Physician.
Evidence-Based Lifestyle Modifications
Scientific studies have identified several key components of successful weight management:
- Balanced Nutrition:
- Regular meal timing
- Portion awareness
- Focus on whole foods
- Physical Activity:
- 150 minutes of moderate activity per week
- Combination of cardio and strength training
- Gradual increase in intensity
- Behavioral Changes:
- Stress management techniques
- Regular sleep patterns
- Mindful eating practices
“Sustainable lifestyle changes, not short-term diets, lead to lasting improvements in both weight and liver health.”
American Journal of Clinical Nutrition, 2024
The Power of Gradual Change
Research demonstrates why gradual changes are more effective:
| Approach | Benefits for Liver Health |
| Steady weight loss (1-2 lbs/week) | Allows liver cells to adapt gradually |
| Regular meal patterns | Stabilizes blood sugar and metabolism |
| Progressive exercise | Improves insulin sensitivity |
Keys to Long-Term Success
Studies have identified several factors that contribute to sustainable weight management:
- Realistic Goal Setting
- Break larger goals into smaller milestones
- Focus on progress, not perfection
- Regular Monitoring
- Track progress systematically
- Adjust approaches based on results
- Support Systems
- Professional guidance when needed
- Family and social support
While these principles are scientifically proven, implementing them effectively often benefits from professional guidance. Understanding your unique situation and health needs can help create a more targeted approach to weight management.
When to Seek Medical Help
While fatty liver disease often develops silently, certain signs and situations warrant professional medical attention. Understanding these warning signs can help you take action at the right time.
Warning Signs That Shouldn’t Be Ignored
- Physical Symptoms:
- Persistent fatigue that doesn’t improve with rest
- Unexplained discomfort in the upper right abdomen
- Noticeable changes in weight without trying
- Swelling in the abdomen or ankles
- Changes in Health Patterns:
- Decreasing energy levels despite lifestyle changes
- Difficulty losing weight despite efforts
- New or worsening digestive issues
High-Risk Situations Requiring Professional Guidance
| Risk Factor | Why It Matters |
| Family history of liver disease | Increased genetic risk for complications |
| Type 2 diabetes | Higher likelihood of liver damage progression |
| Metabolic syndrome | Complex interaction with liver health |
| Previous failed weight loss attempts | May need specialized approach |
“Early intervention in fatty liver disease can prevent progression to more serious conditions, making timely medical consultation crucial for optimal outcomes.”
World Journal of Gastroenterology, 2023
The Value of Early Intervention
Research shows that early medical intervention provides several key advantages:
- Prevention of Progression
- Early stages are more responsive to treatment
- Better chances of reversing liver damage
- Personalized Approach
- Tailored strategies based on individual health status
- Consideration of multiple health factors
- Monitored Progress
- Regular assessment of improvement
- Timely adjustments when needed
If you recognize any of these warning signs or fall into a high-risk category, consulting with healthcare professionals can provide the guidance needed for effective management. Professional support can help create a personalized plan that addresses both your liver health and weight management needs.
Understanding Your Next Steps
The connection between weight and fatty liver disease is well-established by scientific research. Understanding this relationship empowers you to make informed decisions about your health journey.
Key Takeaways to Remember
- Weight management plays a crucial role in liver health, but the approach matters as much as the goal
- Even modest weight loss of 5-7% can significantly improve liver health
- Sustainable, gradual changes are more effective than quick fixes
- Early intervention offers the best opportunity for liver health improvement
- Regular monitoring and professional guidance can help ensure safe progress
“The evidence is clear: appropriate weight management strategies can significantly improve liver health outcomes when implemented properly and monitored regularly.”Journal of Hepatology, 2024
Remember that every person’s journey is unique. While the scientific principles remain constant, the specific approach that works best for you may vary based on your individual circumstances, current health status, and lifestyle factors.
Moving Forward with Confidence
As you consider your next steps in managing fatty liver disease through weight management, focus on:
- Understanding your current health status
- Setting realistic, achievable goals
- Making sustainable lifestyle changes
- Monitoring your progress regularly
- Seeking appropriate guidance when needed
Whether you’re just beginning to explore the connection between weight and liver health or looking to enhance your current approach, remember that informed decisions lead to better outcomes. Consider scheduling a comprehensive health assessment to understand your personal risk factors and develop a tailored plan for your liver health journey.
To access other content on the IFitCenter’s blog, you can use the following links:
References
Clinical Guidelines and Practice Updates
- Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328-357. DOI: 10.1002/hep.29367
- European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64:
- Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology. 2015;149:367-378.
- Cho IY, Chang Y, Sung E, et al. Weight change and the development of nonalcoholic fatty liver disease in metabolically healthy overweight individuals. Clin Gastroenterol Hepatol. 2022;20:e583-e599. DOI: 10.1016/j.cgh.2021.04.037
- Wong VW, Wong GL, Chan RS, et al. Beneficial effects of lifestyle intervention in non-obese patients with non-alcoholic fatty liver disease. J Hepatol. 2018;69:1349-1356.
- Koutoukidis DA, Koshiaris C, Henry JA, et al. The effect of the magnitude of weight loss on non-alcoholic fatty liver disease: a systematic review and meta-analysis. Metabolism. 2021;115:154455.



