Do you put down that glass of wine at social gatherings because you have diabetes? Have you wondered if that occasional beer with friends is secretly damaging your health? For the millions living with diabetes worldwide, these aren’t just casual questions—they reflect a genuine dilemma about balancing enjoyable social activities with careful health management. Can people with diabetes safely consume alcohol? If so, how much is too much? And what precautions should be taken?
These questions touch on a common concern—navigating normal life pleasures while managing a condition that demands vigilant attention to what enters your body. The relationship between alcohol and diabetes is nuanced, with important implications for blood sugar management, medication effectiveness, and overall wellbeing. At IFitCenter, we recognize that understanding this relationship is essential for making informed choices that support both your health goals and quality of life.
Contrary to what some might believe, having diabetes doesn’t necessarily mean complete abstinence from alcohol. For many people with well-controlled diabetes, moderate consumption may be possible with the right knowledge and precautions. This article offers a comprehensive examination of alcohol consumption with diabetes—addressing permissible amounts, necessary safeguards, and potential side effects based on current medical understanding.
Let’s explore what you need to know to make safe, informed decisions about alcohol while effectively managing your diabetes.
Is Alcohol Consumption Allowed with Diabetes?
The short answer is: it depends. For many people with well-controlled diabetes, moderate alcohol consumption may be permissible—but this isn’t a universal green light. Understanding how alcohol interacts with your body’s glucose management system is essential for making informed decisions.
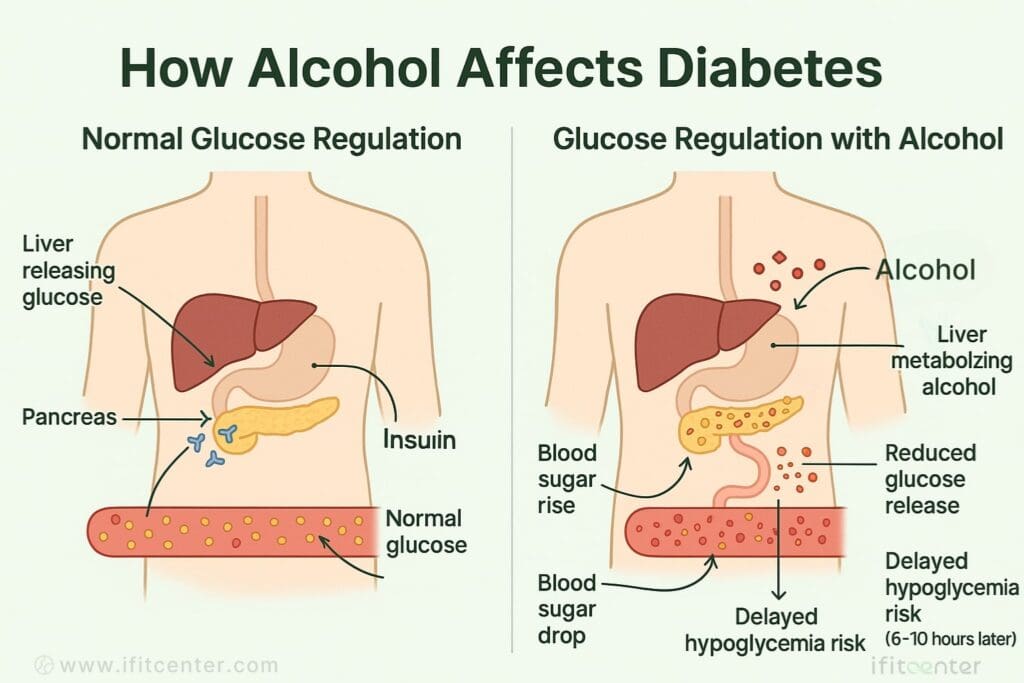
When you consume alcohol, your liver treats it as a toxin and immediately prioritizes metabolizing it above all other functions—including its critical role in regulating your blood glucose. Think of your liver as a multitasking worker who suddenly receives an urgent assignment. Everything else—including releasing stored glucose when your blood sugar drops—takes a backseat until the alcohol is processed.
This creates a complex situation where alcohol can affect your blood sugar in two opposing ways:
- Initial rise: Alcoholic beverages containing carbohydrates (beer, sweet wines, cocktails with mixers) can initially raise blood glucose levels
- Delayed drop: Hours later, alcohol can prevent your liver from releasing stored glucose, potentially leading to dangerous hypoglycemia (low blood sugar)—especially if you’re taking insulin or certain diabetes medications
This dual effect makes alcohol consumption particularly tricky for people with diabetes. As one study published in Diabetologia noted, “The relationship between alcohol consumption and blood glucose regulation is complex and depends on several factors including the amount consumed, timing relative to meals, and individual metabolic responses.”
“One of the most overlooked aspects of alcohol consumption in diabetes is its biphasic effect on blood glucose. What many patients don’t realize is that while carbohydrate-containing drinks may initially raise blood sugar, the real danger often comes 6-10 hours later when the liver, still focused on metabolizing alcohol, cannot release glucose to counter falling blood sugar levels. This delayed hypoglycemic effect is particularly risky during sleep, when warning signs may go unnoticed.”
Dr. Babak Jamalian, Family Physician.
Whether alcohol is safe for you depends on several key factors:
- Your diabetes type and overall control: People with well-controlled diabetes generally have more flexibility than those with unstable blood glucose levels
- Your medication regimen: Insulin and sulfonylureas significantly increase hypoglycemia risk when combined with alcohol
- Presence of complications: Existing diabetes complications like neuropathy or liver disease may be worsened by alcohol
- Your overall health status: Other health conditions might make alcohol consumption more risky
A 2020 study in PLOS ONE focusing on Korean adults found that consuming at least 16g of alcohol daily (approximately two standard drinks) significantly increased type 2 diabetes risk, particularly in individuals with lower BMI. This challenges the common assumption that alcohol-related health risks primarily affect those who are overweight, suggesting that lean individuals may be more vulnerable to alcohol’s metabolic effects.
Similarly, research published in Scientific Reports in 2024 examining Japanese individuals found that excessive alcohol consumption was associated with a 73-78% increased risk of developing diabetes after adjusting for confounding factors.
While these findings suggest caution, they don’t indicate that all alcohol consumption is prohibited for people with diabetes. The American Diabetes Association acknowledges that moderate alcohol intake may be incorporated into the meal plans of many people with diabetes—provided they take appropriate precautions and have no contraindications.
However, some individuals with diabetes should avoid alcohol entirely. This includes people with:
- A history of alcohol abuse
- Pancreatitis
- Advanced neuropathy
- Significant liver disease
- Poorly controlled diabetes
- Pregnancy or planning pregnancy
Medical experts generally agree that if you choose to drink with diabetes, moderation is crucial, along with careful monitoring and awareness of how your body responds. In the next sections, we’ll explore specific guidelines for safer consumption and important precautions to take.
Safe Consumption Guidelines: How Much is Too Much?
For people with well-controlled diabetes who choose to drink, understanding appropriate limits is essential. While individual responses vary, there are general guidelines that can help minimize risks.
On the IFitCenter blog, we have provided a completely free database about diseases, especially diabetes, for you dear readers. This information will be very useful for you in controlling and preventing diseases. To access the first section of information, you can use the links below:
- what is diabetes difinition?
- what is type 1 diabetes?
- what is type 2 diabetes?
- Early signs of diabetes in men
- Lab tests for diabetes patients
- Genetic diabetes symptoms
Recommended Consumption Limits
Medical organizations including the American Diabetes Association suggest these general limits for people with well-controlled diabetes:
- Women: Up to one standard drink per day
- Men: Up to two standard drinks per day
A “standard drink” contains approximately 14 grams of pure alcohol, which equals:
- 5 ounces (150 ml) of wine
- 12 ounces (360 ml) of regular beer
- 1.5 ounces (45 ml) of distilled spirits (vodka, whiskey, gin, etc.)
These guidelines are more conservative than recommendations for the general population—with good reason. Research published in Diabetologia examining over 70,000 Danish adults found that while moderate alcohol consumption showed certain patterns in the general population, the relationship between alcohol and blood glucose regulation is more complex for those with diabetes.
The Glycemic Impact of Different Alcoholic Beverages
Not all alcoholic drinks affect blood sugar equally. When choosing beverages, consider their glycemic impact:
Lower Glycemic Impact Options:
- Dry wines: Contain minimal residual sugar (1-2g carbohydrate per 5 oz serving)
- Light beers: Have fewer carbohydrates (3-6g per 12 oz) than regular beers
- Distilled spirits: Contain virtually no carbohydrates when consumed without mixers (gin, vodka, whiskey, rum)
Higher Glycemic Impact Options (Best Limited or Avoided):
- Sweet wines: Can contain 10-20g of carbohydrates per serving
- Regular beers: Typically contain 10-15g of carbohydrates per 12 oz
- Cocktails with sweet mixers: Can contain substantial sugar from juices, syrups, and sodas
- Liqueurs and dessert wines: Often have high sugar content
The glycemic index of alcoholic beverages isn’t typically measured like food items, but the carbohydrate content gives a good indication of potential blood sugar impact. Dry wines and spirits without mixers would be considered “low GI alcohol” options for those with diabetes.
Frequency Considerations
Research suggests that how often you drink matters as much as how much you drink. The Danish study found that consuming alcohol 3-4 days weekly (in moderate amounts) showed different associations than the same total amount consumed in 1-2 days.
For people with diabetes, spreading consumption across days (rather than concentrated drinking) may be preferable, but several alcohol-free days each week are recommended to avoid potential liver stress.
Individual Variations and Monitoring
Perhaps most importantly, your individual response to alcohol should guide your choices. Factors affecting your response include:
- Your specific type of diabetes
- Your medication regimen
- The timing of alcohol relative to meals
- Your body weight
- Your overall metabolism
The only reliable way to understand your personal response is through careful monitoring. Check your blood glucose before drinking, while drinking, and for up to 24 hours afterward to identify patterns in how different beverages affect you.
Remember that guidelines are just starting points. Your healthcare provider can help develop recommendations tailored to your specific situation, considering your overall diabetes management and health status.
Precautions for Safer Alcohol Consumption with Diabetes
While the World Health Organization (WHO) states that no level of alcohol consumption is safe for health, if you have diabetes and still choose to drink alcohol, these practical precautions can significantly reduce your risk of experiencing complications, particularly dangerous hypoglycemia (low blood sugar).
Balance Diabetes and Lifestyle with IFitCenter
Navigating lifestyle choices like alcohol consumption with diabetes requires expert guidance. At IFitCenter, under Dr. Babak Jamalian’s supervision, we offer personalized weight management programs that support healthy diabetes control and lifestyle balance. Our focused services include:
✔ Tailored nutritional and lifestyle planning
✔ Professional guidance for safe and effective weight loss
✔ Continuous monitoring for optimized blood glucose levels
Achieve your best health while enjoying life responsibly—consult our experts today.
Essential Safety Strategies
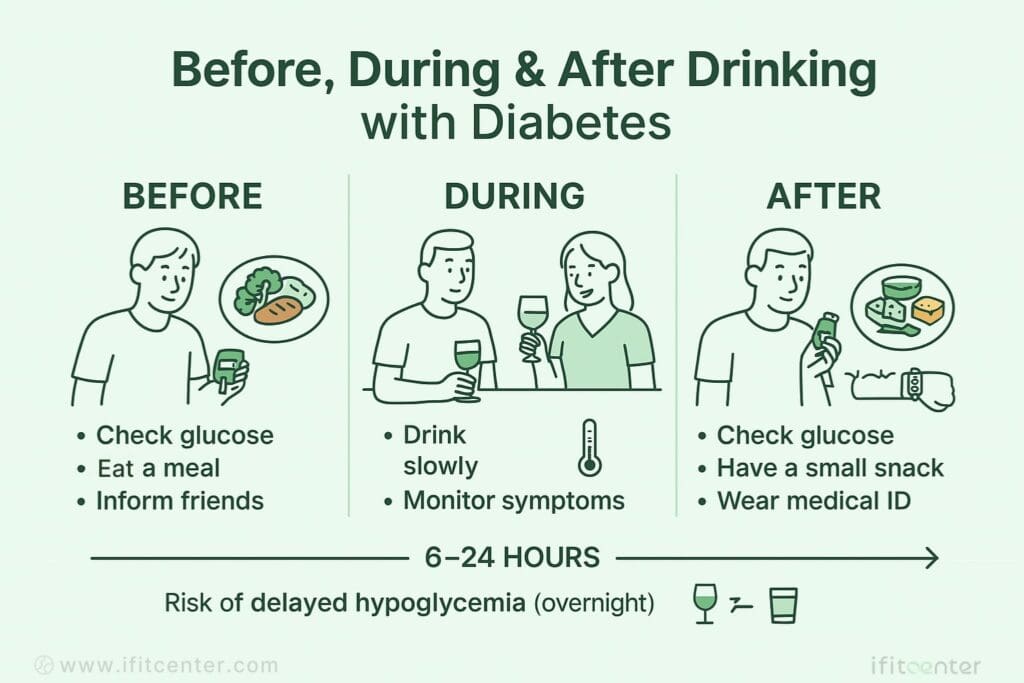
- Never drink on an empty stomach. Food helps slow alcohol absorption and provides glucose to counter potential drops in blood sugar. Opt for meals containing both carbohydrates and protein.
- Check blood glucose before, during, and after drinking. Start with normal levels and monitor more frequently for up to 24 hours after alcohol consumption.
- Carry fast-acting carbohydrates. Always have glucose tablets, juice, or hard candies available to treat hypoglycemia quickly if needed.
- Stay hydrated. Alternate alcoholic beverages with water to maintain hydration and help moderate alcohol intake.
- Eat a bedtime snack after drinking. A snack containing carbohydrates and protein before sleep can help prevent overnight hypoglycemia, especially important if your glucose levels are below 140 mg/dL (7.8 mmol/L) at bedtime.
- Wear medical identification. Hypoglycemia symptoms (confusion, slurred speech) can resemble intoxication, making proper identification crucial in emergencies.
- Educate companions. Ensure friends know you have diabetes and can recognize hypoglycemia symptoms and how to help if needed.
Medication-Specific Considerations
Different diabetes medications interact with alcohol in various ways:
- Insulin users: Consider reducing insulin doses before planned alcohol consumption (only with healthcare provider guidance). Monitor blood glucose more vigilantly as alcohol can increase insulin sensitivity and prolong hypoglycemic effects.
- Sulfonylurea users: Medications like glipizide, glimepiride, and glyburide significantly increase hypoglycemia risk when combined with alcohol. Extra caution and more frequent monitoring are essential.
- Metformin users: While this combination has fewer acute risks, excessive alcohol with metformin can rarely lead to lactic acidosis, particularly in those with kidney or liver issues.
- GLP-1 receptor agonist users: These medications can slow gastric emptying, potentially altering alcohol absorption rates.
- SGLT-2 inhibitor users: The combination may increase risk of dehydration and, rarely, diabetic ketoacidosis.
Monitoring Your Personal Response
Because individual responses to alcohol vary significantly, tracking your own patterns is crucial:
- Keep a simple log of what you drink, when you drink it, and your blood glucose readings before, during, and after
- Note any symptoms that might indicate alcohol-induced diabetes symptoms (unusual thirst, fatigue, headaches, etc.)
- Pay attention to delayed effects—hypoglycemia can occur many hours after drinking
- Identify which beverages and situations cause the least disruption to your glucose levels
This personalized approach helps identify your unique risk factors and tolerances. Over time, this information becomes invaluable for making safer choices about alcohol consumption.
Understanding your individual response to alcohol is complex and varies based on many factors including diabetes type, medication regimen, and overall health. Working with a healthcare professional who specializes in diabetes management can provide personalized guidance tailored to your specific situation and help develop an individualized approach to alcohol consumption that prioritizes both safety and quality of life.
Potential Side Effects and When to Avoid Alcohol Completely
While moderate alcohol consumption may be possible for some people with diabetes, understanding the potential risks and recognizing when abstinence is necessary are crucial aspects of responsible diabetes management.
To access the second section of diabetes-related content, you can use the links below to access the most up-to-date information about diabetes:
- How does obesity cause diabetes
- Complications of diabetes type 1
- Difference between prediabetes and diabetes
- How to Prevent Diabetes?
- Is vinegar good for diabetics?
- Fruits to Avoid with Diabetes
Potential Risks and Side Effects
- Delayed hypoglycemia: Alcohol can cause dangerous blood sugar drops up to 24 hours after consumption, particularly risky while sleeping.
- Masked hypoglycemia symptoms: Alcohol effects (dizziness, sleepiness) can make it difficult to recognize low blood sugar symptoms.
- Initial high blood sugar: Alcoholic beverages containing carbohydrates can temporarily raise blood glucose before the later drop.
- Worsened neuropathy: Alcohol can aggravate existing nerve damage, increasing pain and numbness sensations.
- Liver function interference: The liver must prioritize processing alcohol over maintaining glucose balance, potentially stressing an already taxed organ.
- Impaired judgment: Alcohol affects decision-making about diabetes self-care, potentially leading to missed medication doses or poor food choices.
- Medication interactions: Alcohol can enhance the glucose-lowering effects of insulin and certain diabetes medications.
- Weight management challenges: Alcoholic beverages add calories without nutritional value, potentially complicating weight control efforts.
Who Should Avoid Alcohol Completely
For certain individuals with diabetes, the risks of alcohol consumption significantly outweigh any potential benefits. Complete abstinence is recommended for:
- People with alcoholism or history of alcohol abuse: Including those with type 1 diabetes and a history of alcohol dependency
- Individuals with advanced diabetes complications: Particularly those with significant neuropathy, retinopathy, or nephropathy
- Those with pancreatitis or severe liver disease: Alcohol can worsen these conditions substantially
- Pregnant women with diabetes: Due to risks to both maternal health and fetal development
- People with hypoglycemia unawareness: Those unable to detect early warning signs of low blood sugar face heightened risk
- Individuals with poor glucose control: Uncontrolled diabetes can be further destabilized by alcohol
- Those taking medications that interact with alcohol: Some medications used for diabetes complications have severe interactions
Sugar Alcohols vs. Alcoholic Beverages: Clearing the Confusion
Many people with diabetes encounter “sugar alcohols” on food labels and wonder about their relationship to alcoholic beverages. Despite the similar name, these are entirely different substances:
- Sugar alcohols (such as xylitol, sorbitol, maltitol, and erythritol) are carbohydrate-based sweeteners commonly used in sugar-free products
- Unlike alcoholic beverages, sugar alcohols do not contain ethanol and cannot cause intoxication
- Sugar alcohols do raise blood sugar, but generally less than regular sugar because they’re incompletely absorbed
- They may cause digestive symptoms like gas and diarrhea when consumed in large amounts
This distinction is important—avoiding alcoholic beverages doesn’t mean you need to avoid foods containing sugar alcohols, though their blood glucose impact should still be monitored.
Understanding your individual risk factors and monitoring your responses to both alcohol and sugar alcohols are essential parts of diabetes management. For personalized guidance tailored to your specific health profile, medical history, and diabetes management approach, consulting with a healthcare provider specializing in diabetes care can provide valuable insights and recommendations.
Conclusion
Navigating alcohol consumption while managing diabetes requires balancing enjoyment with health considerations. As we’ve explored, moderate alcohol consumption may be possible for some people with well-controlled diabetes, but this decision should be approached with careful consideration of your individual circumstances.
Remember these key points:
- Alcohol can cause both initial high blood sugar and delayed hypoglycemia, creating complex management challenges
- Lower-glycemic options like dry wines, light beers, or spirits with sugar-free mixers generally have less immediate impact on blood glucose
- Never drink on an empty stomach, always monitor your blood glucose, and have fast-acting carbohydrates available
- Some individuals with diabetes should avoid alcohol completely, particularly those with complications, hypoglycemia unawareness, or certain medical conditions
Your body’s response to alcohol is highly individual and may change over time as your diabetes evolves. What works safely for someone else may not work for you. Personal monitoring and attentiveness to your body’s signals are essential for making informed decisions about alcohol consumption.
To access other content on the IFitCenter’s blog, you can use the following links:
References
- Cao, C., Wei, C., Han, Y., et al. (2024). Association between excessive alcohol consumption and incident diabetes mellitus among Japanese based on propensity score matching. Scientific Reports, 14, 17274. DOI: 10.1038/s41598-024-68202-3
- Baik, I., & Park, S. I. (2020). Associations of alcohol consumption and physical activity with lean type 2 diabetes mellitus among Korean adults: A prospective cohort study. PLOS ONE. DOI: 10.1371/journal.pone.0238641
- Holst, C., Becker, U., Jørgensen, M. E., Grønbæk, M., & Tolstrup, J. S. (2017). Alcohol drinking patterns and risk of diabetes: a cohort study of 70,551 men and women from the general Danish population. Diabetologia, 60(10), 1941-1950. DOI: 10.1007/s00125-017-4359-3
- Gepner, Y., Golan, R., Harman-Boehm, I., Henkin, Y., Schwarzfuchs, D., Shelef, I., Durst, R., Kovsan, J., Bolotin, A., Leitersdorf, E., Shpitzen, S., Balag, S., Shemesh, E., Witkow, S., Tangi-Rosental, O., Chassidim, Y., Liberty, I. F., Sarusi, B., Ben-Avraham, S., Helander, A., Ceglarek, U., Stumvoll, M., Blüher, M., Thiery, J., Rudich, A., Stampfer, M. J., & Shai, I. (2015). Effects of Initiating Moderate Alcohol Intake on Cardiometabolic Risk in Adults With Type 2 Diabetes: A 2-Year Randomized, Controlled Trial. Annals of Internal Medicine, 163(8), 569-79. DOI: 10.7326/M14-1650



