What if the timing of your meals could be as powerful as the medications prescribed for blood sugar control? What if the solution to reversing prediabetes didn’t require counting every calorie or completely eliminating your favorite foods, but instead involved changing when you eat?
If you’re among the millions living with prediabetes, you likely have these questions. You may be wondering if there’s a more sustainable approach than restrictive dieting—one that works with your body’s natural rhythms rather than against them.
These questions are at the heart of why intermittent fasting for prediabetes has become one of the most researched dietary approaches in recent years. The idea that simply adjusting your eating window could help normalize your blood sugar levels seems almost too simple. Yet clinical trials are showing promising results that challenge our traditional understanding of diabetes prevention.
At IFitCenter Clinic, we’re examining this approach comprehensively, looking beyond the hype to understand what the science actually reveals. Is intermittent fasting truly effective for prediabetes management? Which fasting protocol shows the best results? And most importantly—is it right for you?
In this evidence-based guide, we’ll answer these questions by exploring the latest clinical research, breaking down the different fasting methods, and providing practical guidance for those considering this approach to blood sugar management.
The Science Behind Intermittent Fasting and Blood Sugar Control
To understand why intermittent fasting may help with prediabetes, we need to explore what happens in your body during periods without food. Far from being a simple absence of eating, fasting triggers a cascade of metabolic changes that directly affect how your body processes glucose.
“Many of my patients mistakenly believe that fasting and starvation are the same physiological process. They are fundamentally different. During therapeutic intermittent fasting, your body enters a controlled metabolic state where it preferentially burns stored fat while preserving muscle tissue. Stress hormones remain balanced, and cellular repair mechanisms activate. In contrast, starvation is an uncontrolled, prolonged caloric deficit that increases stress hormones, breaks down muscle protein, and suppresses metabolic rate. This distinction is why properly implemented intermittent fasting can improve insulin sensitivity while chronic caloric restriction often fails.”
Dr. Babak Jamalian, Family Physician.
What Happens When We Fast: The Metabolic Switch
When you eat, your body breaks down carbohydrates into glucose, which enters your bloodstream. This triggers your pancreas to release insulin, a hormone that acts like a key, unlocking your cells so glucose can enter and be used for energy.
In prediabetes, this system begins to falter. Your cells become resistant to insulin’s message—imagine the locks on your cells becoming rusty, requiring more and more keys (insulin) to open them. Your pancreas compensates by producing extra insulin, but eventually, it can’t keep up, and blood glucose levels start to rise.
During fasting, something remarkable happens. When you haven’t eaten for several hours (typically beyond 12 hours), your body depletes its glucose reserves and begins a metabolic shift:
- Phase 1 (0-12 hours): Your body uses remaining glucose from your last meal and then taps into glycogen (stored glucose) in your liver.
- Phase 2 (12-18 hours): As glycogen depletes, your body increases fat burning for energy, producing ketones as an alternative fuel source.
- Phase 3 (18+ hours): Your metabolism shifts more completely toward fat utilization, and cellular repair processes intensify.
Think of this like giving your pancreas a much-needed vacation. During this break from constant insulin production, insulin levels naturally decrease, and something critically important happens: your cells begin to regain their sensitivity to insulin—those rusty locks start working more smoothly again.
How Fasting Improves Insulin Sensitivity
Research suggests that intermittent fasting can improve insulin sensitivity through several mechanisms:
- Reduced Insulin Levels: Lower insulin production during fasting periods allows cellular insulin receptors to reset and become more responsive.
- Weight Loss: Even modest weight reduction (5-7%) can significantly improve insulin sensitivity.
- Decreased Inflammation: Fasting appears to reduce inflammatory markers that contribute to insulin resistance.
- Improved Mitochondrial Function: Fasting enhances the efficiency of your cells’ energy-producing components.
As Dr. Eric Berg explains in his educational materials, “When you cut out the carbs, you give [the pancreas] a chance to rest. Also, don’t eat so frequently—do an intermittent fasting program. If you just combine those two actions for a period of 3 days, it’s going to get really easy—your appetite’s going to go away, you’re going to start feeling better right off the bat, and you’ll produce some pancreatic relief.”
The Timing Connection: When You Eat Matters
Recent research has revealed that our bodies process the same foods differently depending on when we eat them. A study published in the Journal of Diabetes Investigation found that the identical meal consumed late at night results in higher blood glucose levels than when eaten earlier in the day.
This phenomenon occurs because:
- Our insulin sensitivity follows a circadian rhythm, naturally decreasing in the evening and night
- Eating in alignment with this rhythm (earlier in the day) improves glucose tolerance
- Extended overnight fasting periods allow for more complete metabolic reset
Think of your metabolism like a factory that needs time for maintenance. If the factory runs 24/7 without breaks, equipment starts to wear down, efficiency drops, and problems develop. Regular scheduled downtime (fasting periods) allows for necessary repairs, making the entire operation more efficient when it’s running.
On the IFitCenter blog, we have prepared an essential guide on the topic of ‘Prediabetes.’ By reviewing it, you will not only increase your awareness about this issue but also gain the ability to control and manage it.
On the IFitCenter blog, we have prepared a comprehensive guide for pre-diabetes, completely free of charge. Using this guide will make controlling and preventing pre-diabetes much easier for you or your loved ones. To access the first part of the content, simply use the links below:
- prediabetes definition
- symptoms of prediabetes
- test for prediabetes
- how to lower prediabetes naturally
- foods prediabetics should avoid
Intermittent Fasting Protocols: Finding Your Fasting Window
Several intermittent fasting approaches have been studied specifically for their effects on blood sugar control. The most common include:
| Protocol | Description | Research Findings |
|---|---|---|
| Time-Restricted Eating (16:8) | Eating within an 8-hour window, fasting for 16 hours daily | 4.02% weight loss, 30.91 mg/dL reduction in fasting blood glucose in a 12-week study |
| Time-Restricted Eating (14:10) | Eating within a 10-hour window, fasting for 14 hours daily | 3.15% weight loss, 28.06 mg/dL reduction in fasting glucose in the same study |
| 5:2 Approach | 5 days of normal eating, 2 non-consecutive days of significant caloric restriction (500-600 calories) | Average 5% weight loss and improved HbA1c in 12 weeks |
| Alternate-Day Fasting | Alternating between normal eating days and fasting or very low-calorie days | Similar benefits to daily time restriction but may be harder to maintain |
Research from 2024 suggests that the 16:8 approach may offer slightly better results than 14:10 for improving blood glucose levels in people with metabolic concerns. However, the best approach is ultimately the one you can maintain consistently.
It’s worth noting that even practicing intermittent fasting just three days per week has shown significant benefits in clinical trials. This “part-time” approach may be more sustainable for many people while still providing meaningful metabolic improvements.
In the next section, we’ll explore the specific research evidence showing how these protocols have performed in clinical trials focused on prediabetes.
Research Evidence: Can Intermittent Fasting Reverse Prediabetes?
Let’s look at what scientific research actually reveals about intermittent fasting and prediabetes. Recent studies offer compelling insights into whether adjusting your meal timing could help normalize blood sugar levels.
“One misconception I frequently address with prediabetic patients is that regular, frequent eating is necessary to maintain stable blood sugar. The research actually suggests the opposite for many people. Strategic fasting periods can give pancreatic beta cells critical recovery time while simultaneously improving insulin receptor sensitivity. What’s particularly encouraging about the recent clinical evidence is that even part-time implementation—fasting just three days per week—shows significant benefits. This makes the approach much more accessible for patients who find daily fasting protocols challenging to maintain in their lifestyle.”
Dr. Babak Jamalian, Family Physician.
The Latest Meta-Analysis: Strong Support for Intermittent Fasting
In 2024, researchers published a comprehensive meta-analysis in the journal Diabetes, Obesity and Metabolism examining intermittent fasting’s effects on people with prediabetes and type 2 diabetes. This analysis compiled data from 14 studies with over 1,100 participants.
The findings were significant. When compared to control diets, intermittent fasting produced:
- Body weight reduction of 4.56 kg
- BMI decrease of 1.99 kg/m²
- HbA1c reduction of 0.81%
- Fasting glucose decrease of 0.36 mmol/L
- Improvements in total cholesterol and triglycerides
What makes this meta-analysis particularly valuable is its size and recency, representing the most up-to-date synthesis of evidence on this topic. The researchers concluded that “intermittent fasting is effective for weight loss and specific cardiometabolic health markers in individuals with prediabetes or type 2 diabetes.”
The PROFAST Trial: Focused on Prediabetes
The PROFAST trial, published in the journal Nutrients, specifically examined how intermittent fasting affects people with prediabetes. In this 12-week study, participants followed a 5:2 intermittent fasting regimen—eating normally for five days each week and restricting calories significantly (600-650 calories) for two non-consecutive days.
The results were promising:
- Average 5% weight loss over 12 weeks
- HbA1c decreased from 43 ± 2.7 mmol/mol to 41 ± 2.3 mmol/mol
- Improved quality of life measures
Comparing Fasting Protocols: Which Works Best for Prediabetes?
A 2024 study published in the Journal of Diabetes Investigation directly compared two popular intermittent fasting protocols—16:8 (fasting for 16 hours, eating within an 8-hour window) and 14:10 (fasting for 14 hours, eating within a 10-hour window).
The study had participants follow these protocols for just three days per week over three months. The results showed:
| Protocol | Weight Loss | Fasting Glucose Reduction |
|---|---|---|
| 16:8 Group | 4.02% | 30.91 mg/dL |
| 14:10 Group | 3.15% | 28.06 mg/dL |
| Control Group | 0.55% | 9.09 mg/dL |
Both intermittent fasting protocols significantly outperformed the control group, with the 16:8 method showing slightly better results than the 14:10 approach. Importantly, these improvements occurred with intermittent fasting performed just three days weekly, not daily.
To access the second part of pre-diabetes content, I invite you to use the links below:
- prediabetes weight loss
- difference between prediabetes and diabetes
- prediabetes and obesity connection
- vitamin d prediabetes
- diabetes numbers and what they mean
- what is hba1c blood test
Safety and Practical Considerations
A legitimate concern about intermittent fasting is whether it’s safe for people with blood sugar issues. The INTERFAST-2 trial, published in Diabetes Care, addressed this question directly.
The researchers found that properly implemented intermittent fasting with appropriate medical guidance led to no severe hypoglycemic events (dangerously low blood sugar). Participants experienced significant benefits including improved glucose control, weight loss, and reduced medication needs.
This safety finding is significant because it suggests that intermittent fasting, when properly implemented, can be both safe and effective. However, proper implementation is key—particularly for those taking medications that could affect blood sugar levels.
The Evidence in Context
An umbrella review published in The Wiley in 2024 provides important context. While finding beneficial associations between intermittent fasting and metabolic health outcomes, particularly for overweight or obese individuals, it noted that the quality of evidence varies considerably across studies.
This highlights the importance of individualized approaches and proper medical guidance. The same fasting protocol that works well for one person may not be optimal for another, depending on their unique health profile.
Professional guidance can help determine the most appropriate protocol based on your health status, medications, lifestyle, and personal preferences—potentially optimizing your results while ensuring safety.
Key Takeaways from Research on Intermittent Fasting for Prediabetes
- Multiple clinical trials show benefits for weight, HbA1c, and fasting glucose
- The 16:8 protocol may offer slightly better results than 14:10
- Even practicing intermittent fasting 3 days weekly shows significant benefits
- Properly implemented, intermittent fasting appears safe for prediabetic individuals
- Results vary between individuals—a personalized approach is optimal
In the next section, we’ll explore practical steps for implementing intermittent fasting safely if you have prediabetes.
Implementing Intermittent Fasting for Prediabetes: A Practical Guide
If you’re considering intermittent fasting to help manage prediabetes, getting started safely is crucial. Let’s translate the research findings into practical steps you can follow, while acknowledging that individual responses vary.
Getting Started: Which Intermittent Fasting Plan Is Best for Prediabetes?
Research suggests starting with a more moderate approach and gradually increasing fasting duration as your body adapts:
- Beginner Level: 12:12 protocol (12 hours eating, 12 hours fasting)
- Intermediate Level: 14:10 protocol (10 hours eating, 14 hours fasting)
- Advanced Level: 16:8 protocol (8 hours eating, 16 hours fasting)
the best approach is one you can maintain consistently. The 2024 research comparing 16:8 and 14:10 protocols found that even practicing intermittent fasting just three days per week produced significant benefits.
Step-by-Step Implementation
- Week 1: Begin with a 12-hour overnight fast. For example, finish dinner by 7:00 PM and don’t eat again until 7:00 AM. This establishes the fasting habit while minimizing discomfort.
- Week 2-3: Extend your fasting window to 14 hours (14:10 protocol). Try finishing dinner by 7:00 PM and having breakfast at 9:00 AM.
- Week 4+: If comfortable, advance to a 16:8 protocol, perhaps eating between 11:00 AM and 7:00 PM. Research shows this approach may offer optimal benefits for blood sugar control.
- Alternative: If daily fasting feels challenging, consider the 5:2 approach—normal eating for 5 days, with 2 non-consecutive days of reduced calories (500-600)—which showed a 5% weight reduction in the PROFAST trial.
Remember that consistency matters more than intensity. The PROFAST trial showed significant benefits with just two fasting days per week, so find an approach you can maintain long-term.
What to Eat During Your Eating Window
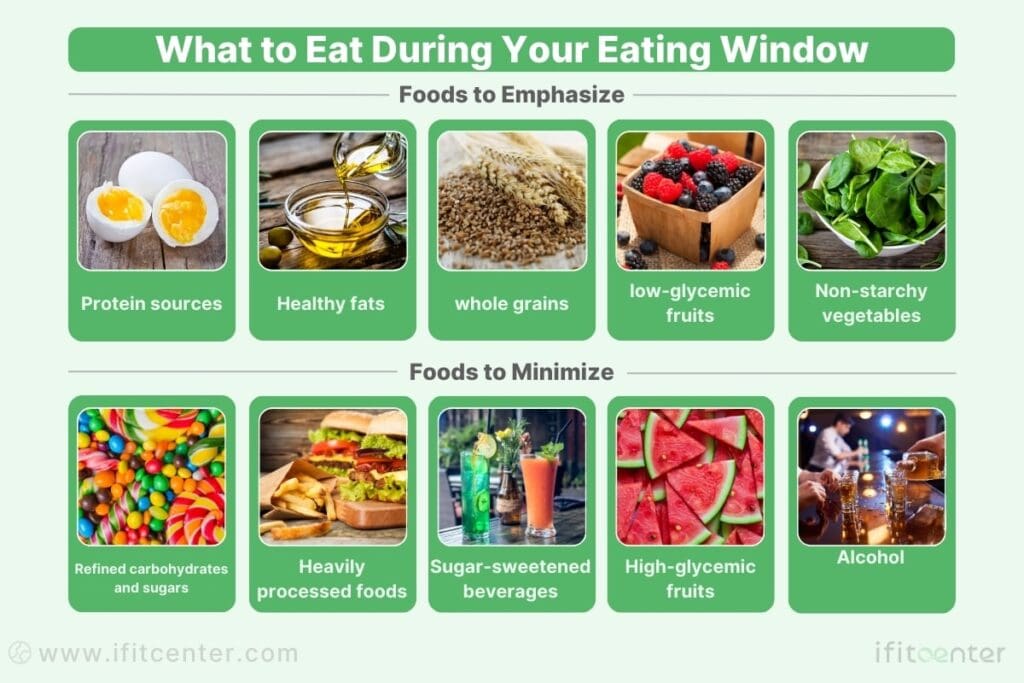
Intermittent fasting isn’t just about when you eat—what you eat still matters, especially for blood sugar management. During your eating window, prioritize:
Foods to Emphasize
- Protein sources (fish, poultry, tofu, eggs)
- Healthy fats (avocados, olive oil, nuts)
- Non-starchy vegetables
- Limited amounts of whole grains
- Small portions of berries and other low-glycemic fruits
Foods to Minimize
- Refined carbohydrates and sugars
- Heavily processed foods
- Sugar-sweetened beverages
- High-glycemic fruits in large quantities
- Alcohol (can disrupt blood sugar patterns)
Tracking Your Progress
Monitoring your progress helps ensure you’re on the right track and allows for timely adjustments if needed:
- Blood Glucose: Consider tracking fasting blood glucose 2-3 times weekly using a home glucometer
- HbA1c: Have this checked every 3 months to assess your average blood sugar
- Weight: Weekly weigh-ins can help track progress, but don’t become overly focused on the scale
- Symptoms: Monitor energy levels, hunger patterns, and any prediabetes symptoms
- Adherence: Track your fasting schedule to monitor consistency
Consider keeping a simple journal documenting your fasting periods, meals, and how you feel. This can help identify patterns and optimize your approach.
Common Challenges and Solutions
| Challenge | Solution |
|---|---|
| Initial hunger | Start with shorter fasting periods and gradually extend. Stay hydrated with water, black coffee, or unsweetened tea. This typically improves within 1-2 weeks as your body adapts. |
| Social situations | Consider adjusting your fasting window to accommodate important social events. The partial implementation approach (3 days/week) used in clinical studies can allow flexibility while still providing benefits. |
| Energy fluctuations | Ensure adequate hydration and electrolytes. During eating windows, focus on nutrient-dense, balanced meals rather than highly processed foods. |
| Plateaus in progress | Consider varying your fasting schedule occasionally. The research suggests that metabolic adaptations may require periodic adjustments to continue seeing benefits. |
The PROFAST trial reported that 48% of participants experienced mild side effects initially, including headaches (17%), dizziness/nausea (13%), and irritability (13%). However, most found these manageable, rating the difficulty as 3.8 out of 10, and 93% indicated they would continue with intermittent fasting after the study.
Most challenges are temporary as your body adapts to the new eating pattern. Patience and gradual implementation are key.
Get Professional Support to Reverse Prediabetes
Reversing prediabetes isn’t about cutting calories—it’s about choosing the right foods that balance blood sugar, improve insulin sensitivity, and restore metabolic health. A well-structured diet can help lower your A1C, reduce cravings, and prevent diabetes—but only if it’s tailored to your needs.
At IFitCenter, we offer:
✔ Scientifically designed meal plans to control blood sugar naturally
✔ Guidance on portion sizes, meal timing, and food combinations
✔ A personalized approach to prediabetes reversal through proper nutrition
Take charge of your health with an expert-led diet plan today!
Safety Considerations: Is Intermittent Fasting with Prediabetes Safe?
While research shows intermittent fasting can help prediabetes, it’s not appropriate for everyone. Certain medical conditions and medications require special consideration to ensure safety and effectiveness.
Who Should Exercise Caution with Intermittent Fasting?
The INTERFAST-2 trial published in Diabetes Care demonstrated that intermittent fasting can be safe for people with blood sugar concerns when properly implemented. However, certain groups should approach with caution:
- Pregnant or breastfeeding women should avoid intermittent fasting
- People with a history of eating disorders may find the restriction triggers unhealthy patterns
- Those with advanced diabetes complications require medical supervision
- People with significant weight loss (BMI below 18.5) should not fast
- Individuals with other chronic conditions (kidney disease, advanced heart disease) need medical guidance
The 2024 umbrella review in The Wiley emphasized that individual responses to intermittent fasting vary considerably, highlighting the importance of personalized approaches based on individual health profiles.
Medication Considerations for Intermittent Fasting if Prediabetic
Certain medications require careful consideration when implementing intermittent fasting:
| Medication Type | Considerations |
|---|---|
| Diabetes medications | Medications that increase insulin (sulfonylureas, meglitinides) may need adjustment to prevent hypoglycemia during fasting periods |
| Blood pressure medications | May require monitoring and adjustment as fasting can naturally lower blood pressure |
| Medications requiring food | Some medications specify “take with food” and may need schedule adjustments |
In the INTERFAST-2 trial, researchers demonstrated safety by instructing participants to reduce their basal insulin by 20% on fasting days. This highlights how medication adjustments can make intermittent fasting safe even for those on insulin therapy—but such adjustments should only be made under medical supervision.
Warning Signs: When to Adjust Your Intermittent Fasting Plan
Be alert for these signals that your current approach may need modification:
- Persistent dizziness or lightheadedness beyond the initial adaptation period
- Excessive fatigue that interferes with daily activities
- Blood sugar readings below 70 mg/dL (hypoglycemia)
- Significant sleep disturbances
- Persistent headaches that don’t improve with hydration
- Rapid heartbeat or palpitations during fasting periods
If you experience these symptoms, consider shortening your fasting window or consulting with a healthcare provider to adjust your approach.
Intermittent Fasting and Prediabetes: Key Takeaways and Next Steps
As we’ve explored throughout this guide, intermittent fasting shows promising potential as a strategy for managing prediabetes. Let’s recap the key points and outline practical steps for those interested in this approach.
Can Fasting Reverse Prediabetes? The Evidence
Research suggests intermittent fasting may help manage and potentially reverse prediabetes through several mechanisms:
- Improved Insulin Sensitivity: Fasting periods allow insulin receptors to reset and become more responsive
- Weight Loss: Multiple studies show significant weight reduction, which itself improves blood sugar control
- Better Glucose Control: Clinical trials demonstrate notable reductions in HbA1c and fasting blood glucose
- Metabolic Flexibility: Regular fasting enhances the body’s ability to switch between different fuel sources
The PROFAST trial, which specifically studied people with prediabetes, found that a 5:2 intermittent fasting approach led to significant improvements in multiple health markers. Meanwhile, the 2024 comparative study showed both 16:8 and 14:10 protocols outperformed conventional approaches, even when practiced just three days weekly.
Prediabetes represents a critical window of opportunity where the right interventions can potentially prevent progression to full diabetes. The growing body of research on intermittent fasting suggests it may be one valuable tool in addressing this important health challenge.
To access other content on the IFitCenter’s blog, you can use the following links:
References for “Best Intermittent Fasting for Prediabetes”
The information in this article is based on the following scientific sources:
- Khalafi M, Maleki A, Symonds M, Rosenkranz S, Rohani H, Ehsanifar M. (2024). The effects of intermittent fasting on body composition and cardiometabolic health in adults with prediabetes or type 2 diabetes: A systematic review and meta-analysis. Diabetes, Obesity and Metabolism. DOI: 10.1111/dom.15730
- Tay A, Pringle H, Penning E, Plank L, Murphy R. (2020). PROFAST: A Randomized Trial Assessing the Effects of Intermittent Fasting and Lacticaseibacillus rhamnosus Probiotic among People with Prediabetes. Nutrients, 12(11), 3530. DOI: 10.3390/nu12113530
- Sukkriang N, Buranapin. (2024). Effect of intermittent fasting 16:8 and 14:10 compared with control-group on weight reduction and metabolic outcomes in obesity with type 2 diabetes patients: A randomized controlled trial. Journal of Diabetes Investigation. DOI: 10.1111/jdi.14186
- American Diabetes Association. (2025). Standards of Care in Diabetes. Diabetes Care. Guidelines for prediabetes diagnostic criteria and management approaches.
Note: The content provided in this article is for informational purposes only and should not be considered medical advice. Always consult with a qualified healthcare provider before making any changes to your diet, especially if you have prediabetes or other health conditions.



