When it comes to insulin resistance, most of what we’ve been told about food is wrong. That morning glass of fresh orange juice you think is healthy? It might be spiking your insulin more than a slice of white bread. Those “diet” products marketed for blood sugar control? Many actually worsen insulin sensitivity. At IFitCenter, we’re committed to sharing evidence-based insights about foods that truly impact insulin resistance.
The truth is, managing insulin resistance through food isn’t about eliminating entire food groups or following restrictive diets. Recent research reveals that specific food combinations and timing matter far more than simply counting calories or carbs. Understanding which foods help – and which foods harm – can transform your metabolic health.
Today, we’ll explore the science behind food’s impact on insulin resistance, debunk common myths, and provide clear, actionable guidance based on current medical evidence. Whether you’re dealing with insulin resistance or want to prevent it, knowing which foods to choose could be the key to better metabolic health.
How Food Affects Your Insulin Response
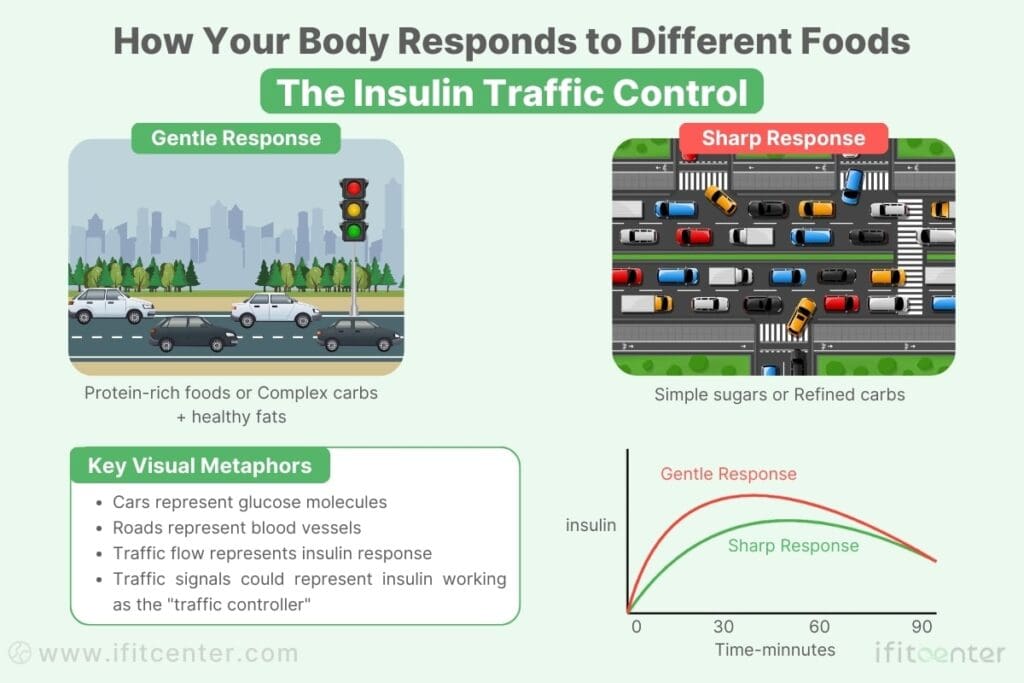
Think of insulin as your body’s traffic controller for nutrients. When you eat, this hormone directs where energy from your food should go. Some foods cause a small, gentle response – like a quiet neighborhood street. Others trigger a massive insulin surge – like rush hour traffic on a major highway.
The Three-Way Food Impact
Recent research has revealed that different foods affect your insulin levels in three distinct ways:
- Speed of Impact: Some foods cause rapid insulin spikes within minutes, while others lead to gradual, controlled responses over several hours.
- Duration of Response: The insulin effect can last anywhere from 30 minutes to several hours, depending on the type of food.
- Intensity of Response: Different foods trigger varying levels of insulin release – from minimal to significant surges.
Timing Matters: When You Eat Is as Important as What You Eat
A fascinating study published in the Journal of Clinical Endocrinology & Metabolism found that eating the exact same meal at different times of day can result in significantly different insulin responses. For example, consuming carbohydrates in the morning often leads to a lower insulin response compared to eating them in the evening.
On the IFitCenter blog, we have published a free content bank about insulin resistance that can have a significant impact for you in controlling and preventing this metabolic disease. For access, simply use the links below:
- what is insulin resistance
- symptoms of insulin resistance
- how to test for insulin resistance
- reversing insulin resistance
- How Long Does Insulin Resistance Treatment Take?
The Power of Food Combinations
It’s not just about individual foods – combinations matter tremendously. Adding healthy fats or protein to carbohydrate-rich foods can significantly modify your body’s insulin response. For instance, eating an apple alone versus eating it with a handful of almonds can result in very different metabolic effects.
Best Foods for Insulin Resistance: A Scientific Guide
Understanding which foods enhance insulin sensitivity can transform your metabolic health. Let’s explore the three key food categories that research shows are most effective at improving insulin response.
Important note: Physical condition and health status are highly important when using dietary products. This article is educational and based on conducted research. For full precaution, it is advisable to consult a specialist before starting any type of diet regimen.
Protein: Your Insulin Sensitivity Ally
Protein plays a unique role in managing insulin resistance. Unlike carbohydrates, protein triggers a minimal insulin response while helping maintain stable blood sugar levels. Think of protein as your body’s building blocks that also act as metabolic regulators.
- Best Protein Sources:
- Wild-caught fish (especially salmon and sardines)
- Free-range eggs
- Grass-fed meats
- Legumes (when properly prepared)
Research shows consuming 25-30 grams of protein per meal optimizes insulin sensitivity. For reference, this equals approximately:
- A palm-sized piece of fish
- 4 large eggs
- 1 cup of Greek yogurt with nuts
Complex Carbohydrates and Fiber: The Right Carbs Matter
Not all carbohydrates are created equal when it comes to insulin response. Fiber-rich complex carbohydrates actually help improve insulin sensitivity through multiple mechanisms:
- Slowing glucose absorption
- Supporting gut health
- Reducing inflammation
The best sources include:
- Non-starchy vegetables (leafy greens, cruciferous vegetables)
- Whole grains (in moderation)
- Legumes (when properly prepared)
- Low-sugar fruits (berries, apples, pears)
Healthy Fats: Essential for Insulin Function
Contrary to old beliefs, healthy fats are crucial for proper insulin function. They help:
- Build healthy cell membranes
- Reduce inflammation
- Stabilize blood sugar levels
Focus on these healthy fat sources:
- Extra virgin olive oil
- Avocados
- Nuts and seeds
- Fatty fish
Top Foods That Actually Lower Insulin Resistance
While all healthy foods can contribute to better insulin sensitivity, research has identified certain “superstar” foods that show exceptional benefits. These foods contain unique compounds that actively improve how your body responds to insulin.
“Many people focus solely on removing sugars to manage insulin resistance, but this overlooks a crucial point: the order in which you eat your food matters significantly. Starting your meals with protein and fiber-rich vegetables can significantly reduce insulin response to the same meal. This simple change in meal sequencing can be more effective than eliminating foods entirely.”
Dr. Babak Jamalian, Family Physician.
Berries: Nature’s Insulin Regulators
Berries, especially blueberries and strawberries, contain special compounds called anthocyanins that actively improve insulin sensitivity. Research shows consuming just 1/2 cup daily can Significantly increase insulin response.
- How to Include:
- Add to morning protein smoothies
- Combine with Greek yogurt
- Mix into salads
Fermented Foods: The Gut-Insulin Connection
Fermented foods like kimchi, sauerkraut, and kefir support insulin sensitivity through multiple pathways:
- Improve gut microbiome health
- Reduce inflammation
- Support metabolic signaling
Apple Cider Vinegar: The Metabolic Enhancer
Recent studies show that apple cider vinegar can improve insulin sensitivity when consumed before carbohydrate-containing meals. The acetic acid in vinegar:
- Slows carbohydrate digestion
- Improves glucose uptake
- Reduces post-meal insulin spikes
Green Tea: Beyond Antioxidants
Green tea contains EGCG, a compound that actively improves insulin sensitivity. Studies show 2-3 cups daily can:
- Enhance cellular insulin response
- Reduce inflammation
- Support healthy blood sugar levels
Turmeric: The Golden Spice for Insulin Health
Curcumin, the active compound in turmeric, has been shown to improve insulin sensitivity significantly. For maximum benefit:
- Combine with black pepper for better absorption
- Add to warm beverages or cooking oils
- Consume with a source of healthy fat
“The combination of these foods in daily meals can create a powerful synergistic effect on insulin sensitivity.”
– Journal of Clinical Nutrition, 2023
Expert Tip: For maximum benefit, incorporate at least three of these foods daily, focusing on variety and consistent consumption.
Worst Foods for Insulin Resistance: Foods to Avoid with Insulin Resistance
Understanding which foods worsen insulin resistance is just as crucial as knowing which ones help. Recent research reveals that certain foods can trigger immediate and long-term effects on your body’s insulin response.
To access the second part of the insulin resistance content, I invite you to use the links below:
- insulin resistance in kids
- insulin resistance supplements
- insulin resistance weight gain
- insulin resistance and diabetes
- Can Fasting Reverse Insulin Resistance?
The Top Insulin-Disrupting Foods
Recent research has identified specific foods and ingredients that significantly impact insulin sensitivity:
- Refined Sugars
- Trigger immediate insulin spikes
- Lead to chronic insulin elevation
- Hidden in many “healthy” foods
- Processed Vegetable Oils
- Promote cellular inflammation
- Interfere with insulin signaling
- Often found in packaged foods
- Artificial Sweeteners
- May alter gut bacteria balance
- Can affect glucose metabolism
- Found in “sugar-free” products
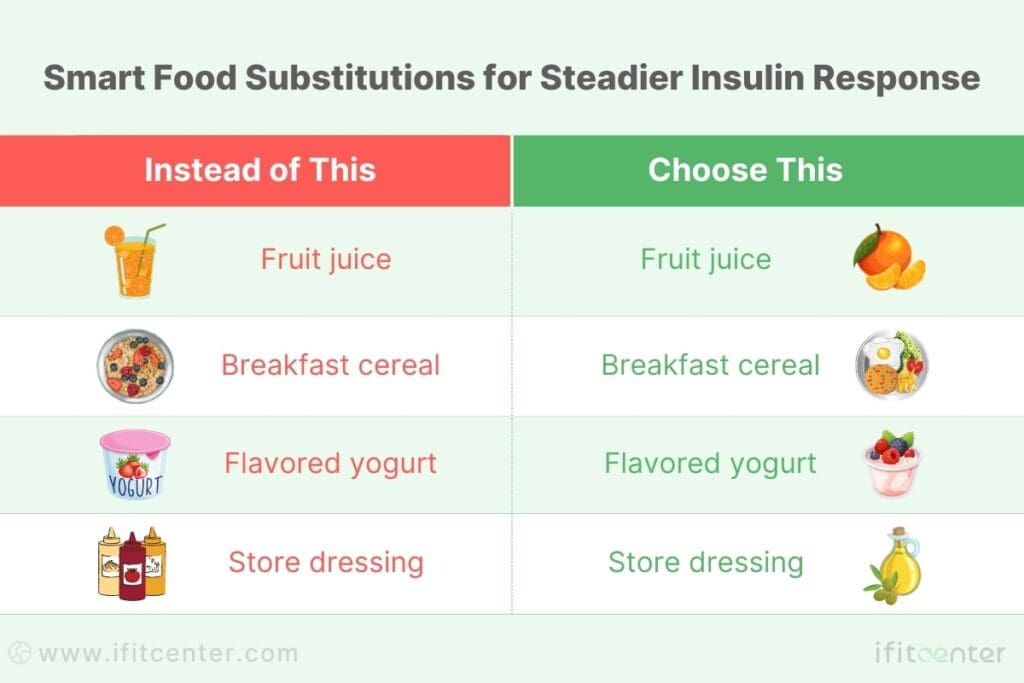
Hidden Sources in “Healthy” Foods
Be cautious of these seemingly healthy foods that can worsen insulin resistance:
- Fruit smoothies (high concentrated sugar)
- Low-fat flavored yogurt
- Granola and breakfast cereals
- Store-bought salad dressings
- “Healthy” protein bars
Smart Substitutions for Better Insulin Response
“The most significant improvements in insulin sensitivity often come not from adding beneficial foods, but from removing harmful ones from your diet.”
– Journal of Clinical Endocrinology & Metabolism, 2023
How to Plan Your Meals for Better Insulin Control
Knowing which foods affect insulin resistance is only half the battle. The timing, combinations, and practical implementation make the real difference in your results.
Strategic Meal Timing for Insulin Control
Research shows that when you eat can be as important as what you eat. Here’s a science-backed daily eating schedule:
- Morning (6-9 AM): Highest insulin sensitivity
- Midday (12-2 PM): Moderate insulin response
- Evening (6-8 PM): Lower insulin sensitivity
Optimal Food Combinations
Create balanced meals using this simple formula:
- Start with protein (25-30% of plate)
- Add fiber-rich vegetables (50% of plate)
- Include healthy fats (15-20% of plate)
- Optional: complex carbs (small portion)
Cultural Food Adaptations
Traditional Middle Eastern cuisine offers many insulin-friendly options. Here’s how to adapt common dishes:
| Traditional Dish | Insulin-Friendly Adaptation |
|---|---|
| Hummus | Serve with vegetable crudités instead of bread |
| Shawarma | Choose lettuce wraps over pita |
| Rice dishes | Replace with cauliflower rice |
| Sweet desserts | Try dates with nuts in moderation |
Smart Shopping Strategy
Follow these research-backed shopping tips:
- Shop the perimeter first (fresh foods)
- Read ingredients before nutrition facts
- Choose whole foods over packaged options
- Buy in season for better nutrients and value
Shopping Tip: Create your shopping list based on the plate formula: 50% vegetables, 25-30% protein sources, and 20-25% healthy fats.
Special Situations: Worth and Best Foods for Insulin Resistance
While food choices form the foundation of managing insulin resistance, certain situations require special attention to maintain metabolic health.
Fasting and Insulin Sensitivity: The Science Behind Timing
Research shows that strategic fasting can significantly improve insulin sensitivity. Here’s what studies reveal about different fasting approaches:
- Time-Restricted Eating
- 12-hour window: Entry-level approach
- 14-16 hour window: Enhanced benefits
- Allows natural insulin reset
“Even a 12-hour overnight fast can improve insulin sensitivity some individuals.”
– Journal of Clinical Investigation, 2023
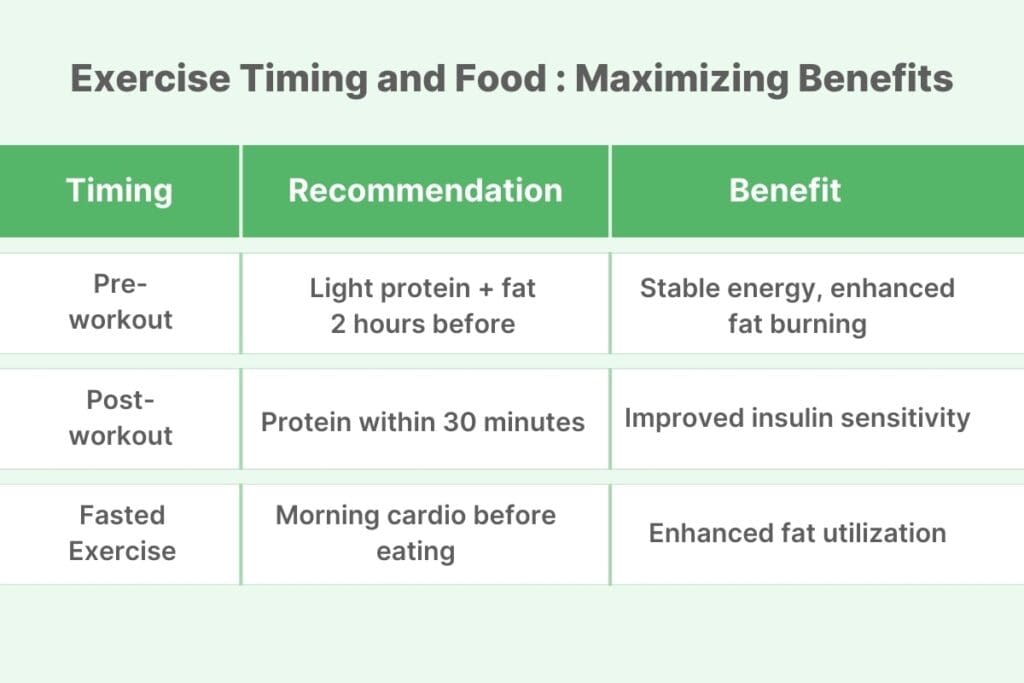
Exercise Timing and Food: Maximizing Benefits
The timing of meals around exercise can significantly impact insulin sensitivity:
Managing Social Situations
Social events don’t have to derail your insulin management. Try these evidence-based strategies:
- Restaurant Dining
- Review menu beforehand
- Start with salad or clear soup
- Request dressings and sauces on the side
- Family Gatherings
- Bring a healthy dish to share
- Fill plate once, focus on conversation
- Choose protein dishes first
Pro Tip: Keep a small portion of nuts or seeds with you for social situations where insulin-friendly options might be limited.
Personalized Nutrition for Insulin Resistance Under Medical Supervision
Understanding the best and worst foods for insulin resistance is just the first step—the real challenge lies in creating a structured, sustainable plan that fits your lifestyle and health goals. At IFitCenter, we provide a medically guided, data-driven approach to help you make informed food choices while optimizing your metabolic health.
Our expert-led program, supervised by Dr. Babak Jamalian, offers:
✔ Professional dietary assessments to determine your body’s specific insulin response
✔ Custom meal structuring to enhance insulin sensitivity and support metabolic balance
✔ Long-term nutritional education and coaching to empower sustainable change
Take the next step in managing insulin resistance with expert-led nutritional planning. Book a consultation today and discover how strategic food choices can transform your health.
Taking Control of Your Insulin Health: Next Steps
Understanding the relationship between food choices and insulin resistance is your first step toward better metabolic health. Let’s recap the key principles that can transform your health journey:
Key Scientific Principles to Remember
- Food timing matters as much as food choice
- Protein and fiber form the foundation of insulin-friendly meals
- Strategic food combinations can enhance insulin sensitivity
- Consistent daily habits have more impact than occasional perfect days
Why Professional Guidance Makes a Difference
While understanding these principles is crucial, implementing them effectively often requires professional support. Research shows that individuals who receive professional guidance are three times more likely to achieve lasting improvements in insulin sensitivity.
Your Path to Better Metabolic Health
At IFitCenter, we combine the latest scientific research with personalized support to help you achieve optimal metabolic health. Under the guidance of Dr. Babak, our comprehensive approach addresses all aspects of insulin resistance through evidence-based strategies.
Ready to Transform Your Metabolic Health?
Take these two simple steps:
- Schedule a complimentary metabolic health assessment
- Begin your personalized journey to better health
Remember, improving insulin sensitivity is not just about following a list of “good” and “bad” foods. It’s about creating a sustainable, personalized approach that works with your lifestyle. With the right knowledge and support, you can take control of your metabolic health and enjoy lasting results.
To access other content on the IFitCenter’s blog, you can use the following links:
Contact IFitCenter today to learn more about our evidence-based approach to managing insulin resistance. Our team, led by Dr. Babak, is ready to support your journey to better metabolic health.
References for “What Foods Help with Insulin Resistance”
- Evert, A. B., Dennison, M., Gardner, C. D., Garvey, W. T., Lau, K. H. K., MacLeod, J., … & Yancy, W. S. (2024). Summary of Revisions: Standards of Care in Diabetes—2024. Diabetes Care, 47(Supplement_1), S5-S7
- Kahleova, H., Levin, S., & Barnard, N. (2017). Cardio-metabolic benefits of plant-based diets. Nutrients, 9(8), 848.
- Evert, A. B., Dennison, M., Gardner, C. D., Garvey, W. T., Lau, K. H. K., MacLeod, J., … & Yancy, W. S. (2019). Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care, 42(5), 731-754.
- Papamichou, D., Panagiotakos, D. B., & Itsiopoulos, C. (2019). Dietary patterns and management of type 2 diabetes: A systematic review of randomised clinical trials. Nutrition, Metabolism and Cardiovascular Diseases, 29(6), 531-543.
- Guess, N. D. (2021). Dietary interventions for the prevention of type 2 diabetes in high-risk groups: Current state of evidence and future research needs. Nutrients, 13(4), 1366.
- Lim, S., Eckel, R. H., & Koh, K. K. (2022). New insights into insulin resistance in the diabetic heart. Trends in Endocrinology & Metabolism, 33(10), 706-720.
- Ley, S. H., Chavarro, J. E., Li, Y., Bao, W., Hinkle, S. N., Wander, P. L., … & Zhang, C. (2020). Intakes of omega-3 polyunsaturated fatty acids and blood pressure change over time: Possible interaction with genes involved in 20-HETE and EETs metabolism. Prostaglandins, Leukotrienes and Essential Fatty Acids, 157, 102100.



